-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(8): 2582-2585
doi:10.5923/j.ajmms.20251508.34
Received: Jun. 5, 2025; Accepted: Jul. 3, 2025; Published: Aug. 6, 2025

Clinical and Radiological Features of Patients with Mild Chronic Generalized Periodontitis Associated with Type 2 Diabetes Mellitus
Fozilova Umida Kamalovna1, Khabibova Nazira Nasulloevna2
1Department of Stomatology, Urganch Branch of the Tashkent Medical Academy, Uzbekistan
2DSc, Professor, Bukhara State Medical Institute Department of Therapeutic Stomatology, Uzbekistan
Correspondence to: Khabibova Nazira Nasulloevna, DSc, Professor, Bukhara State Medical Institute Department of Therapeutic Stomatology, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

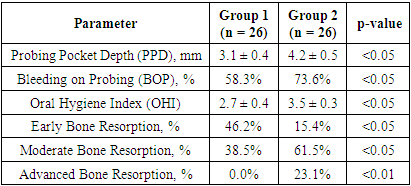
Introduction: This study investigates the clinical and radiological features of patients with mild chronic generalized periodontitis (CGP) associated with type 2 diabetes mellitus (T2DM). A cohort of 52 patients was analyzed, including individuals with newly diagnosed diabetes and those with a disease duration exceeding ten years. Results: A total of 52 patients with mild chronic generalized periodontitis (CGP) associated with type 2 diabetes mellitus (T2DM) were examined. Participants were divided into two groups based on diabetes duration. Group 1 included 26 patients with T2DM for less than five years, while Group 2 included 26 patients with T2DM for over ten years. Clinical, radiological, and hygiene parameters were analyzed to assess the progression of periodontal disease and its correlation with diabetes duration. Conclusion: This study highlights the significant impact of type 2 diabetes mellitus (T2DM) duration on the clinical and radiological progression of chronic generalized periodontitis (CGP). Patients with a longer history of T2DM exhibited more severe periodontal inflammation, deeper periodontal pockets, and greater alveolar bone resorption. These findings underscore the importance of early diagnosis and proactive management of periodontal disease in diabetic patients.
Keywords: Chronic Generalized Periodontitis, Type 2 Diabetes Mellitus, Periodontal Inflammation, Alveolar Bone Resorption, Oral Hygiene, DMFT Index, Radiological Assessment
Cite this paper: Fozilova Umida Kamalovna, Khabibova Nazira Nasulloevna, Clinical and Radiological Features of Patients with Mild Chronic Generalized Periodontitis Associated with Type 2 Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 15 No. 8, 2025, pp. 2582-2585. doi: 10.5923/j.ajmms.20251508.34.
1. Introduction
- Oral health, as an integral part of overall health, Chronic generalized periodontitis (CGP) is a pathological condition characterized by inflammation of the periodontal tissues, attachment loss, and alveolar bone resorption. The coexistence of CGP with type 2 diabetes mellitus (T2DM) presents a clinically significant challenge due to the mutual influence of these conditions. Hyperglycemia in T2DM is associated with impaired immune function, reduced vascularization, and altered tissue repair mechanisms, which contribute to accelerated periodontal destruction.Patients with T2DM often exhibit specific periodontal features, including gingival bleeding, increased periodontal pocket depth, and alveolar bone loss detectable through radiological assessment. Despite advancements in understanding the pathophysiological links between these conditions, insufficient oral hygiene practices remain a critical factor in the progression of CGP in diabetic patients. Moreover, the duration of diabetes may exacerbate periodontal tissue damage, as prolonged hyperglycemia further compromises the integrity of oral structures.This study examines the clinical and radiological characteristics of patients with mild CGP on the background of T2DM, focusing on the periodontal indices, hygiene practices, and bone tissue changes. The findings aim to provide a foundation for improved diagnostic accuracy and tailored therapeutic interventions for patients with comorbid CGP and T2DM.The study included 52 patients diagnosed with mild chronic generalized periodontitis (CGP) in the presence of type 2 diabetes mellitus (T2DM). The participants were divided into two groups based on the duration of T2DM. Group 1 consisted of patients with newly diagnosed T2DM, and Group 2 included individuals with a disease duration exceeding ten years.Clinical evaluation involved recording complaints such as gingival bleeding, unpleasant sensations, and signs of oral mucosa involvement. Periodontal tissues were assessed for inflammation, edema, hyperemia, cyanosis, periodontal pocket depth, and bleeding on probing. Quantitative assessments of periodontal health included measurements of the Hygiene Index (HI) and the Decayed, Missing, and Filled Teeth (DMFT) index, with values expressed as means and standard deviations.Radiological assessment utilized orthopantomography to evaluate the extent of bone destruction. Specific features analyzed included the degree of interdental septa resorption, loss of compact bone, and osteoporotic changes. These radiological findings were compared between the two groups to assess the influence of diabetes duration on alveolar bone structure.The level of oral hygiene was determined using clinical measurements of dental plaque and calculus accumulation. The Hygiene Knowledge Index (HKI) was applied to assess the patients’ awareness of oral hygiene principles, while practical skills were evaluated through direct observation of oral hygiene practices. Statistical analysis was performed to compare clinical and radiological parameters between the two groups, with significance defined as p < 0.05.The methodology employed provides a detailed framework for examining the relationship between T2DM duration and the clinical and radiological characteristics of CGP. This approach ensures precision in evaluating the effects of systemic disease on periodontal health.Literature Review. Chronic generalized periodontitis (CGP) is a progressive inflammatory disease of the periodontal tissues, characterized by attachment loss and alveolar bone resorption. Its association with systemic diseases, particularly type 2 diabetes mellitus (T2DM), has been extensively studied. Hyperglycemia in T2DM exacerbates periodontal destruction by impairing immune responses and promoting chronic inflammation [1].Clinical studies have shown that patients with T2DM exhibit increased gingival bleeding, pocket depth, and alveolar bone loss. Radiographic evidence often demonstrates pronounced resorption of interdental septa and compact bone loss, correlating with prolonged hyperglycemia and inadequate metabolic control [2].The inflammatory mechanisms linking T2DM and CGP are multifaceted, involving oxidative stress, advanced glycation end-products, and altered cytokine profiles. These factors collectively disrupt periodontal tissue homeostasis and contribute to progressive tissue degradation [3].Recent research highlights the critical role of oral hygiene practices in managing CGP in diabetic patients. Despite theoretical knowledge of proper techniques, inadequate skills often lead to poor plaque control and exacerbation of periodontal inflammation [4].Radiological assessments, such as orthopantomography, remain the gold standard for detecting alveolar bone changes in CGP patients. Early detection of bone resorption facilitates timely intervention and can prevent further periodontal tissue damage [5].Adjunctive therapies, including ozone therapy and antimicrobial agents, have shown promise in enhancing the efficacy of conventional periodontal treatments in diabetic patients. Controlled trials demonstrate improved clinical outcomes with these approaches [6].The bidirectional relationship between T2DM and CGP necessitates integrated management strategies. Improved glycemic control has been associated with reduced severity of periodontal inflammation and slower progression of bone loss [7]. Lifestyle factors, such as smoking, further complicate the management of CGP in diabetic patients. Smoking has been linked to increased tissue destruction and reduced efficacy of periodontal treatments [8].Studies on animal models have provided insights into the mechanisms of periodontal destruction in the presence of systemic diseases. Ligature-induced periodontitis models in diabetic rodents replicate the pathological features observed in humans, enabling the exploration of targeted therapies [9].The role of adipose tissue in systemic inflammation has also been studied in relation to periodontal disease. Obesity-related inflammation appears to exacerbate periodontal tissue destruction, highlighting the importance of managing systemic risk factors [10]. Emerging evidence suggests that psychological stress may influence the progression of CGP. Stress-related immune modulation can exacerbate periodontal inflammation, necessitating holistic approaches to patient care [11].Advancements in the understanding of the oral microbiome have opened new avenues for therapeutic interventions. Dysbiosis in diabetic patients with CGP underscores the need for antimicrobial and prebiotic therapies to restore microbial balance [12].The association between CGP and systemic diseases such as cardiovascular conditions further emphasizes the systemic impact of periodontal inflammation. These findings highlight the importance of periodontal health as a component of overall medical care [13]. Recent advancements in periodontal regenerative techniques, including the use of growth factors and stem cells, offer promising avenues for restoring lost periodontal structures in diabetic patients [14].Integrated multidisciplinary approaches involving dentists, endocrinologists, and primary care physicians are essential for optimizing outcomes in patients with CGP and T2DM. Such collaboration ensures comprehensive management of both periodontal and systemic conditions [15].
2. Methodology
- A total of 52 patients with mild chronic generalized periodontitis (CGP) associated with type 2 diabetes mellitus (T2DM) were examined. Participants were divided into two groups based on diabetes duration. Group 1 included 26 patients with T2DM for less than five years, while Group 2 included 26 patients with T2DM for over ten years. Clinical, radiological, and hygiene parameters were analyzed to assess the progression of periodontal disease and its correlation with diabetes duration.The mean probing pocket depth (PPD) in Group 1 was 3.1 ± 0.4 mm, whereas Group 2 exhibited deeper pockets, with a mean PPD of 4.2 ± 0.5 mm. Bleeding on probing (BOP) was observed in 58.3% of patients in Group 1 and 73.6% in Group 2 (p < 0.05). Clinical findings indicated that patients with a longer diabetes duration had more pronounced inflammation, including edema and cyanosis of gingival tissues.Orthopantomographic analysis demonstrated significant differences in bone loss patterns between the groups. In Group 1, early-stage resorption (loss of up to 1/4 of the interdental septa height) was detected in 46.2% of cases, while 38.5% showed no visible resorption. In Group 2, moderate bone resorption (loss of 1/3 of the septa height) was identified in 61.5% of cases, and 23.1% demonstrated advanced bone loss (exceeding 1/2 of the septa height). These findings suggest progressive structural deterioration of periodontal tissues with prolonged exposure to hyperglycemia.The oral hygiene index (OHI) was significantly higher in Group 2 (3.5 ± 0.3) compared to Group 1 (2.7 ± 0.4), indicating poorer oral hygiene in patients with a longer history of diabetes (p < 0.05). Higher levels of dental plaque and calculus were observed in Group 2, correlating with increased severity of periodontal inflammation.A strong positive correlation was identified between diabetes duration and PPD (r = 0.68, p < 0.01). Similarly, a moderate correlation was observed between diabetes duration and the extent of bone loss (r = 0.53, p < 0.05). These data confirm the role of chronic hyperglycemia as a contributing factor to periodontal tissue destruction.
|
3. Results and Discussion
- The data indicate that periodontal disease severity is significantly influenced by the duration of T2DM. Patients with a longer history of diabetes exhibited deeper periodontal pockets, higher BOP rates, and more advanced bone loss. These findings underscore the progressive impact of chronic hyperglycemia on periodontal tissues and highlight the need for early detection and intervention.The correlation between poor oral hygiene and disease severity further emphasizes the importance of personalized oral hygiene education and consistent professional monitoring. These measures are critical in mitigating the detrimental effects of T2DM on periodontal health.This analysis provides a basis for further research into optimizing management strategies for patients with CGP and T2DM. Future studies should evaluate the long-term effects of integrated therapeutic approaches, focusing on glycemic control and targeted periodontal therapies.
4. Conclusions
- This study highlights the significant impact of type 2 diabetes mellitus (T2DM) duration on the clinical and radiological progression of chronic generalized periodontitis (CGP). Patients with a longer history of T2DM exhibited more severe periodontal inflammation, deeper periodontal pockets, and greater alveolar bone resorption. These findings underscore the importance of early diagnosis and proactive management of periodontal disease in diabetic patients.The observed correlations between diabetes duration, oral hygiene status, and periodontal indices emphasize the need for personalized preventive strategies. Interventions such as tailored oral hygiene education, regular professional cleanings, and adjunctive periodontal therapies are essential to mitigate disease progression. Additionally, tight glycemic control remains a critical factor in preserving periodontal health and preventing severe complications.Future studies should investigate the long-term outcomes of integrated dental and medical approaches to managing CGP in patients with T2DM. The development of innovative therapeutic modalities and their clinical validation will further enhance periodontal care for this high-risk population.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML