-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2358-2363
doi:10.5923/j.ajmms.20251507.57
Received: Jun. 28, 2025; Accepted: Jul. 16, 2025; Published: Jul. 24, 2025

Improved Locked Intramedullary Osteosynthesis for Distal Tibial Fractures
Irismetov M. E., Kamolov B. Kh., Alimov A. P.
Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Ministry of Health of the Republic of Uzbekistan (Tashkent)
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Surgical treatment of fractures of the lower third of the tibia is considered difficult due to the anatomical and biomechanical features. Locked intramedullary osteosynthesis with rods (LIOS), extramedullary osteosynthesis LCP (Locking Compression Plate), and transosseous osteosynthesis (Ilizarov apparatus and rod apparatus) are widely used for the surgical treatment of these fractures. However, due to some shortcomings of the traditional LIOS method, complications such as non-union of bones, breakage of metal structures and deformations are often observed. In this study, the condition of bones and joints in the postoperative period after the application of the improved LIOS technique using the AOFAS (American Orthopaedic Foot and Ankle Society) scale was analysed. Materials and Methods: The study was conducted at the Republican Specialised Scientific and Practical Medical Centre for Traumatology and Orthopedics in 2020–2022 and included 35 patients who underwent LIOS surgery. The patients were divided into two groups: the study group (n=18) - patients who were treated using the improved LIOS technique, and the control group (n=17) - patients who underwent traditional LIOS. The postoperative functional state of the bones was assessed using the AOFAS scale, and such indicators as pain, functional state, and degree of deformation were analysed. Results: In patients who used the improved LIOS method, the pain level according to the AOFAS scale was 32.9 (±3.4), while in the control group it was 29.1 (±4.9) (p=0.0008). The functional state in the control group was 33.9 (±2.4), and in the group with the improved LIOS technique - 40.8 (±3.64) (p<0.0001). The degree of deformation in the control group was 7.5 (±0.87), in the study group - 9.3 (±0.48) (p<0.00). The total score on the AOFAS scale in the control group was 78.29 (±6.97), in the study group - 85.27 (±6.1), which gave a difference of 6.98 points. Conclusion: The improved LIOS technique has demonstrated its effectiveness in the treatment of distal tibia fractures when assessed according to the AOFAS scale. This approach can contribute to a more rapid restoration of the functional state of bones in the postoperative period and a decrease in the number of postoperative complications, which leads to accelerated rehabilitation of patients.
Keywords: Distal tibia, Improved LIOS, AOFAS scale, Functional status
Cite this paper: Irismetov M. E., Kamolov B. Kh., Alimov A. P., Improved Locked Intramedullary Osteosynthesis for Distal Tibial Fractures, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2358-2363. doi: 10.5923/j.ajmms.20251507.57.
Article Outline
1. Introduction
- Fractures of the distal third of the tibia present considerable clinical challenges due to the unique anatomical and biomechanical characteristics of this region. The surgical management of these fractures often involves Locking intramedullary osteosynthesis (LIOS), which has gained recognition as a principal method of treatment [3,12]. LIOS offers several advantages, including minimal disruption to surrounding soft tissues, early mobilization, and expedited functional recovery. Nevertheless, the distinct anatomical structure and limited vascularity of the distal tibia contribute to a notable risk of postoperative complications. Several authors have reported a high complication rate associated with LIOS in this anatomical zone, with some Western studies indicating an incidence of complications as high as 40% [5]. These findings underscore the need for further evaluation of the efficacy and safety of LIOS in treating distal tibial fractures.Studies have reported that the incidence of postoperative wound infections following LIOS ranges from approximately 5% to 15%, depending on factors such as surgical technique, adherence to sterilisation protocols, and individual patient characteristics. For instance, Zhang et al. (2019) observed a 12% infection rate among 85 patients who underwent LIOS, attributing the elevated risk primarily to delays in surgical intervention [15]. These findings highlight the importance of timely surgery and strict intraoperative hygiene in minimising postoperative complications.Nonunion and Delayed Union. Nonunion and delayed union are recognised as common complications following the treatment of distal femoral fractures. According to a meta-analysis conducted by Müller et al., the incidence of nonunion in distal femoral fractures managed with the LIOS was reported to be 8.4% [9]. These complications are multifactorial in origin and are primarily attributed to inadequate mechanical stability at the fracture site, compromised bone quality often due to osteoporosis or other metabolic bone disorders and suboptimal patient compliance with postoperative rehabilitation protocols.Mechanical Failure and Postoperative Complications Associated with LIOS. Mechanical failure of the LIOS components represents a significant postoperative concern. Improper placement of LIOS elements or excessive biomechanical loading has been identified as a primary cause of structural failure, with an incidence reported at approximately 6% of cases [8]. Emphasis has been placed on the necessity of precise intraoperative positioning of the implant to mitigate such risks. Moreover, LIOS implants, particularly when used in distal femoral fractures, have been associated with increased soft tissue irritation due to the design and positioning of hardware components.Implant malposition or displacement has been documented in up to 10% of cases, occasionally necessitating surgical revision or implant removal [2,13]. Angular deformities and irregular fracture alignments remain a challenge, with retrospective analyses revealing that approximately 15% of patients developed clinically significant mechanical instability, frequently attributed to intraoperative technical errors. Gupta et al. also highlight that chronic osteomyelitis poses a serious risk, especially in the context of open fractures, with an incidence of 4% in one study—primarily associated with delayed surgical intervention [1,4].Chronic postoperative pain is another prevalent complication, with persistent pain beyond six months reported in 18% of patients, some of whom required revision surgery for symptomatic relief [1,14]. Although rare, neurovascular injury remains a serious adverse event. O'Brien et al. reported transient peroneal nerve palsy in 2 out of 50 patients, both resolving spontaneously within three months [10]. Additionally, a longitudinal study conducted by Kwan demonstrated a 9% rate of reoperation due to postoperative complications, including implant failure, infection, or progressive bone loss [7].Challenges and Optimisation of LIOS in Distal Tibial Fractures. Locking intramedullary nail osteosynthesis (LIOS) represents a promising, minimally invasive technique for the treatment of distal third tibial fractures. This method is associated with accelerated bone healing and reduced soft tissue disruption. Nevertheless, several postoperative complications remain prevalent, including infection, nonunion, mechanical failure, and malalignment. These challenges underscore the need for continued refinement of LIOS technique, implant design enhancements, and comprehensive preoperative risk stratification.A notable biomechanical limitation of traditional LIOS is its performance in cases involving a short distal fracture segment. Under physiologic loading, particularly during early weight-bearing, the substantial mechanical stress transmitted from the proximal tibial segment may result in instability of the distal fragment, thereby predisposing to malalignment or fixation failure [11]. This instability arises from the unequal distribution of mechanical forces across the fracture site.Postoperative immobilisation is commonly employed in these cases to enhance fracture stability and prevent early complications. However, prolonged immobilisation can lead to restricted ankle joint mobility and transient hypotrophy of the periarticular soft tissues. Following one month of immobilisation, patients often experience delayed functional recovery and a protracted rehabilitation period.Conversely, premature mobilisation without adequate stabilisation may result in varus or valgus deformities of the tibia. The short distal fragment and its anatomical proximity to the tibiotalar joint render it particularly vulnerable to axial misalignment and mechanical overload, leading to severe pain and compromised rehabilitation outcomes. Early weight-bearing can further exacerbate these issues by generating discordant forces along the bone-metal axis, increasing the risk of ankle joint arthrosis, pseudarthrosis, or improper fracture union.Given these risks, the development of personalised rehabilitation and immobilisation protocols is essential. Tailoring postoperative care to the individual patient's fracture characteristics, bone quality, and overall health status can significantly improve clinical outcomes and minimise the incidence of LIOS-related complications.Objective: To evaluate the impact of an optimised surgical approach to the LIOS (Locking Intramedullary Osteosynthesis) procedure—specifically tailored to the anatomical characteristics of the fracture site—on postoperative complications, rehabilitation duration, and the functional integrity of the tibial bone in fractures involving the distal third of the tibia.
2. Materials and Methods
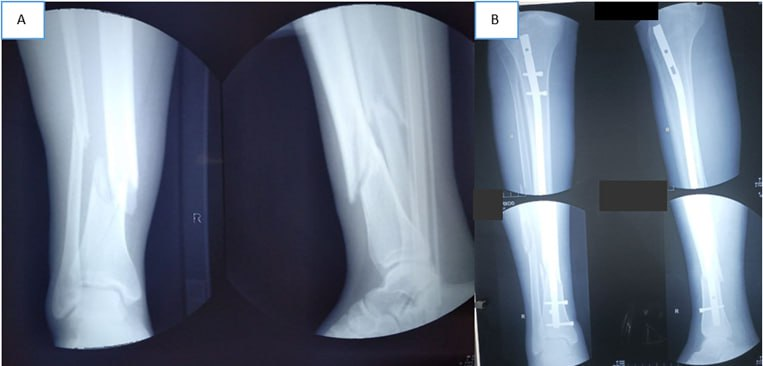
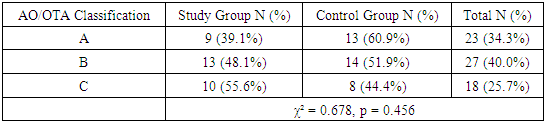
- This study was conducted at the Republican Specialised Scientific and Practical Medical Centre for Traumatology and Orthopaedics and involved a total of 67 patients who underwent LIOS for distal femoral fractures between 2020 and 2023. Patients' data were analysed using a case-control design.The study group consisted of 32 patients who underwent LIOS using an improved surgical technique tailored to the characteristics of the fracture site. Among them, 17 (53.1%) were female and 15 (46.9%) were male.The control group included 35 patients treated using the traditional LIOS method, comprising 18 (51.4%) male and 17 (48.6%) female patients.Outcomes were compared between the two groups in terms of postoperative complications, rehabilitation duration, and functional bone integrity. Statistical Analysis:Data analysis was performed using Microsoft Excel 2019 (Microsoft Corp., USA) and JMP 18 Pro (SAS Institute Inc., USA). The normality of data distribution was confirmed as normal, and group comparisons were conducted using the Chi-squared test for categorical variables and the independent samples T-test for continuous variables. Statistical significance was defined as a p-value less than 0.05.Improved LIOS TechniqueTo address the limitations and complications observed with the conventional LIOS method, a modified surgical approach was developed and implemented by specialists at our institute. The improved technique involves osteosynthesis using a locking intramedullary rod with enhancements designed to better stabilise fracture fragments, reinforce the hip joint, and prevent angular deformities.After standard insertion and fixation of the intramedullary rod, the proximal and distal bone fragments are aligned and temporarily stabilised under real-time guidance using an electron-optical converter (C-arm fluoroscopy) (Figure 1-A). To further enhance fixation of the distal fragment—especially in cases with short distal segments—two additional percutaneous channels are created on the lateral cortex of the distal femur using a drill guide. Through these channels, position screws with a diameter of 3.5 mm and a length of 4.0–6.5 cm are inserted outside the rod, securing the bone from lateral aspects (Figure 1-B).
 | Figure 1. Schematic representation of the improved LIOS (Locking Intramedullary Osteosynthesis) technique |
 | Figure 3. The patient is 48 years old, male. Diagnosis: Closed comminuted fracture of the lower third of the left tibia and upper and lower thirds of the fibula. Improved LIOS procedure performed |
3. Results of the Study
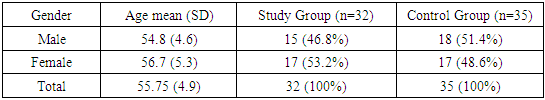
- As shown in Table 1, males comprised 46.5% (n=15) of the study group and 51.4% of the control group. The mean age was 56.7 ± 5.3 years for female patients and 54.8 ± 4.6 years for male patients. Statistical analysis revealed no significant differences between the study and control groups in terms of age and gender distribution (χ² = 0.0756, P = 0.678), indicating that the groups were comparable at baseline.Fractures were categorized based on the AO/OTA classification system. Type B fractures were the most commonly observed, accounting for 40% (n=27) of the total patient population. Among these, 48.1% (n=13) were in the study group (Table 1).
|
|
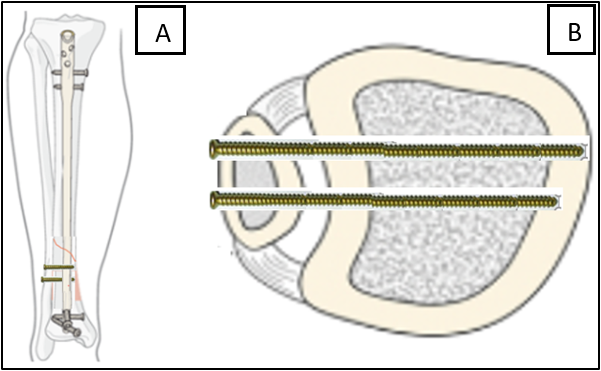
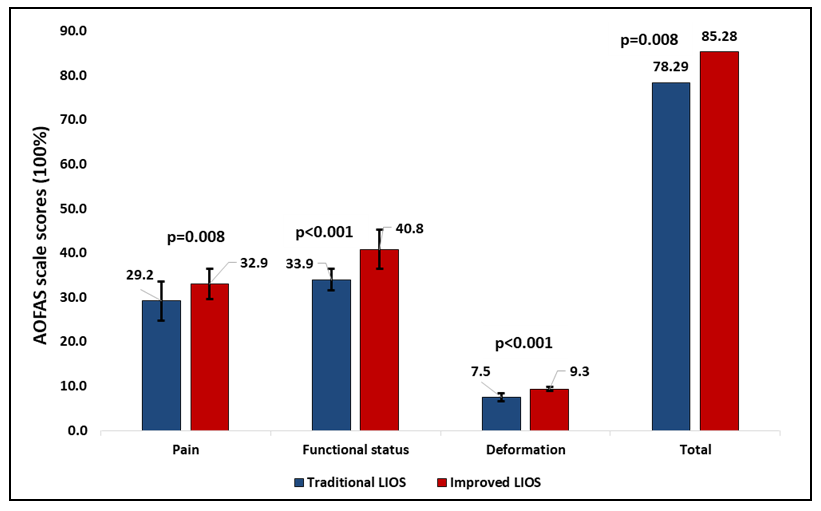 | Figure 4. Evaluation of postoperative treatment outcomes of improved and traditional LIOS procedures using the AOFAS (American Orthopaedic Foot and Ankle Society) scale |
4. Discussion
- The surgical management of distal tibial fractures remains challenging due to the limited soft tissue coverage, subcutaneous location, and high mechanical stress on the lower third of the tibia. Traditional locked intramedullary osteosynthesis (LIOS) has been widely utilised due to its biomechanical advantages and minimally invasive approach. However, studies have reported complications such as non-union, malalignment, and implant failure with conventional techniques [17].In this study, the improved LIOS technique showed significantly better outcomes compared to the traditional approach. Patients treated with the modified technique experienced lower pain levels, improved joint function, and reduced deformity, as measured by the AOFAS scale. These findings align with reports suggesting that refinements in surgical technique, including better alignment, enhanced fixation stability, and early mobilization, contribute to improved outcomes [19].The statistically significant improvement in total AOFAS scores in the improved LIOS group (85.27 ± 6.1 vs. 78.29 ± 6.97; p < 0.05) supports the clinical efficacy of the enhanced method. Similar results have been observed in comparative studies where newer osteosynthesis techniques led to superior functional scores and lower complication rates [18].Despite the positive results, the study has limitations, including a relatively small sample size and a short follow-up period. Further large-scale randomized controlled trials are needed to confirm these findings and evaluate long-term outcomes. Additionally, comparative studies with other fixation methods such as locking compression plates (LCP) and external fixators like the Ilizarov apparatus could provide a more comprehensive understanding of the optimal treatment approach for distal tibial fractures [16].In conclusion, the improved LIOS technique demonstrates clear benefits in managing distal tibial fractures, offering enhanced functional recovery, fewer complications, and potentially faster rehabilitation. These findings support its broader application in orthopedic trauma care.
5. Conclusions
- The application of the improved LIOS procedure in the treatment of complex fractures of the distal femur offers several notable clinical advantages. This technique is minimally invasive, eliminates the need for postoperative immobilization, and facilitates early mobilization and rehabilitation. It is also suitable for cases requiring dynamization during the healing process.Importantly, patients undergoing the improved procedure experienced a significant reduction in postoperative pain, contributing to greater comfort and faster functional recovery. Furthermore, the technique enhances load distribution in the lower limb, thereby reducing the risk of malalignment and deformities, particularly in cases with a short distal fragment.Collectively, these benefits contribute to improved clinical outcomes and underscore the value of the improved LIOS method in modern orthopedic surgical practice.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML