-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2349-2354
doi:10.5923/j.ajmms.20251507.55
Received: Jun. 23, 2025; Accepted: Jul. 16, 2025; Published: Jul. 24, 2025

Examination of the Eustachian Tube Using Video Endoscopy and Acoustic Impendance
Nigora Makhkamova1, Nilufar Usmanova1, Murodullo Zaynutdinov2
1Department of Otorhinolaryngology Tashkent State Medical University, Uzbekistan
2Department of Maxillofacial Diseases and Traumatology Tashkent State Medical University, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

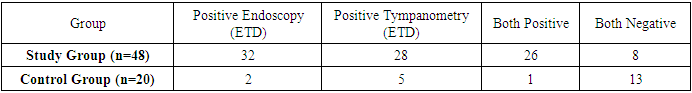
This study evaluated the effectiveness of video endoscopy of the nasal cavity, nasopharynx, and acoustic impedance to diagnose Eustachian tube dysfunction. The study involved children aged 2 to 18 years. The main group consisted of 48 patients diagnosed with otitis media, and the control group consisted of 20 healthy children. Among 48 patients in the main group, endoscopic examination revealed Eustachian tube dysfunction in 32 patients, and acoustic impedance measurement in 28 patients. In the control group, 18 out of 20 patients were identified as healthy, with no ENT pathology based on endoscopy, and 15 based on acoustic impedance measurement. This study emphasizes the importance of combining visualizing and functional diagnostic methods for more accurate and timely diagnosis of Eustachian tube dysfunction, which in turn helps improve treatment outcomes for middle ear diseases such as exudative otitis.
Keywords: Eustachian tube dysfunction, Otitis media, Pediatric endoscopy, Acoustic impedance audiometry, Tympanometry, Nasopharyngeal anatomy
Cite this paper: Nigora Makhkamova, Nilufar Usmanova, Murodullo Zaynutdinov, Examination of the Eustachian Tube Using Video Endoscopy and Acoustic Impendance, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2349-2354. doi: 10.5923/j.ajmms.20251507.55.
1. Introduction
- To date, there are numerous data confirming that auditory tube dysfunction (ATD) is one of the main causes of middle ear diseases and represents a serious health problem. DST is more common in children, covering approximately 4-20% of cases [1,2,6,7]. Among the consequences of DST, one can distinguish otitis media with effusion (OME) and retrusion of the tympanic membrane, which leads to a large number of doctor visits, reaching 2.6 million per year [3,4]. Currently, infectious-inflammatory diseases of the upper respiratory tract occupy a leading position among diseases due to their prevalence [5,9,12,22]. Particularly relevant are inflammations of the nose and nasopharynx, as well as the middle ear, which occupy a significant place in the pathology of ENT organs [8,9,10,11]. According to modern data, there is an increase in the number of combined diseases of the paranasal sinuses and middle ear, as well as an increase in chronic processes. This can be due to several factors, including increased virulence of pathogenic microflora and difficulty in diagnosing complex inflammations when one or another symptom predominates [13,15]. This situation makes recovery difficult and requires thorough therapy. First of all, the damage to the mucous membrane in the case of acute inflammation can be caused by viruses such as rhinovirus, influenza virus, and parainfluenza. Bacterial rhinosinusitis develops as a complication of a viral infection [16,17,18]. Disorders of mucociliary clearance can occur due to changes in the quantity and viscosity of secretions, which is often observed in catarrhal inflammation and hyperproduction of mucus [19,20]. In turn, disorders in the work of mucociliary tracts lead to congestion of discharge in the nasal cavity, paranasal sinuses, and at the mouth of the auditory tube, which reduces the pH level and oxygen content, creating conditions for bacterial growth and the development of rhinosinusitis with concomitant auditory tube dysfunction [21,22].Endoscopy and acoustic impedance imaging (AI) are effective methods for assessing auditory tube dysfunction. Within the framework of our study, children aged 2 to 18 years were examined, in whom auditory tube function was assessed using endoscopy and acoustic impedance measurement. 48 patients diagnosed with otitis media were used as the study cases, and 20 healthy ears were included in the control group. To assess the function of the auditory tube in both groups, endoscopy and acoustic impedance measurement were performed. The sensitivity and specificity of these methods were assessed in the main and control groups. Of the 48 patients who underwent both tests, 32 were diagnosed with auditory tube dysfunction based on endoscopy results, and 28 were diagnosed with acoustic impedance measurement. In the control group, out of 20 patients, 18 ears were recognized as healthy based on endoscopy results, and 15 - based on acoustic impedance measurement.The inability to diagnose chronic otitis media in a timely manner remains a significant healthcare problem in several countries, as it is the primary cause of hearing loss. The etiology of middle ear diseases is multifactorial, however, the disruption of mechanical function and mucociliary dysfunction of the auditory tube are among the main factors in the development of these diseases.The purpose of this study was to determine the effectiveness of videoendoscopy for visualizing the auditory canal opening in patients with auditory canal dysfunction, as well as to conduct acoustic impedance measurement.
2. Materials and Methods
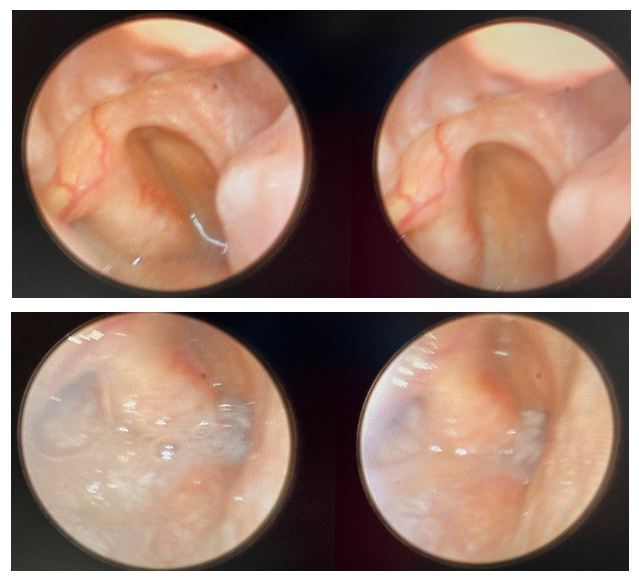
- This prospective study was conducted in the ENT department of the Tashkent State Dental Institute. A total of 68 children (2–18 years) were examined: 48 with otitis media (96 ears) and 20 healthy controls (40 ears). Patients with prior ear surgery, chronic mesotympanitis, or severe nasopharyngeal anomalies were excluded.Rigid endoscopy (2.7 mm and 4 mm, 0° scope, Chamed CU-5000) was used to evaluate nasal and nasopharyngeal anatomy, including the Eustachian tube orifice. To assess the condition of the nasal cavity, mucous membrane, and the nature of the discharge present, the examination was conducted twice - immediately upon patient arrival, assessing the presence of swelling, general nasal breathing, the presence of discharge and the condition of the mucous membrane, its smoothness or tuberosity, whiteness and blueness, i.e., signs of an allergic component; then, a blood vessel-constricting preparation, in particular, nazivin 0.025% (can be used from 1 year to 6 years, 2-3 drops in each nasal cavity are recommended), was sprayed into the nasal cavity, the patient was left for 7-10 minutes, and then the examination was repeated.Tympanometry assessed middle ear pressure and mobility. Any tympanogram deviating from type A was considered abnormal. Tympanometric criteria:§ Type B: Suggests fluid or blockage§ Type C: Indicates negative middle ear pressure§ Type B/C: Combination or borderline conditionsIndividuals who had previously undergone any ear surgery and had chronic mesotimpanitis were excluded. The study excluded children under 3 years of age, cases of gross nasopharyngeal anomalies, such as congenital malformations, such as a wolf's palate, weakened or severely ill patients, and polypous rhinosinusitis. Ears that fully met the above-mentioned criteria - included and excluded - were selected for the study. Then, both groups were examined using video endoscopy and acoustic impedance measurement.During endoscopy of the posterior part of the nose, patients were asked to perform a series of throats at the time of examination, which made it possible to assess the mobility of the tubal roller and the degree of opening of the auditory tube entrance, the presence of mucopurulent pathways in the area of the mouth, which also contribute to the obstruction of the lumen.
3. Results
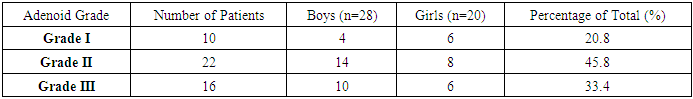
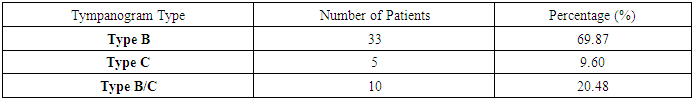
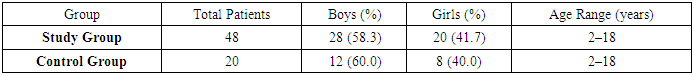
- A total of 68 patients were included in the study, with 48 patients in the main and 20 patients in the control groups. Patients in the main and control groups were comparable in age and gender. The age of patients in both groups ranged from 2 to 18 years. There, 28 (58.3%) boys and 20 (41.6%) girls were in the observation group, while 12 (60%) boys and 8 (40%) girls were in the control group.Endoscopy of the nasal cavity showed that the size of 1st-degree adenoid vegetations was observed in 10 patients, including 4 boys and 6 girls. The prevalence of 2nd-degree adenoid vegetations was higher, amounting to 50% in boys and 45.9% in girls. The occurrence of 3rd-degree adenoid vegetations was also significant, accounting for 41.3% in the boys' group and 37.8% in the girls' group. These indicators confirm a direct correlation between the size of adenoid vegetations and auditory tube obstruction. The B-type tympanometry indicators constituted 69.87% of all patients, the C-type tympanometry indicators - 9.6%, and the B-C-type indicators - 20.48%.Of the 48 patients in the study group who underwent both tests, 32 had ST dysfunction according to the endoscopic picture and 28 - according to acoustic impedance measurement. Among the 20 patients in the control group, 18 were identified as healthy patients without LOR organ pathology by endoscopy, and 15 by acoustic impedance measurement.Children are more vulnerable to middle ear pathology than adults. This is mainly due to the fact that ET dysfunction is a common disease in children. ET in children has several differences compared to adults. In children, the tube is generally shorter, but with the bone part, it is relatively longer compared to adults. Additionally, ET in children is more horizontal. The inclination of the tube relative to the horizontal level in a newborn is approximately 10°. Moreover, in children, the bone-cartilage connection appears linear. Finally, the submucosa of the tubules in children is characterized by more developed accumulations of lymphoid tissue, which form tubar rollers. The same applies to more pronounced adenoids in children compared to adults.
|
|
|
|
4. Discussion
- The present study highlights the diagnostic significance of combining video endoscopy and acoustic impedance (AI) measurement in evaluating Eustachian tube dysfunction (ETD), particularly in pediatric patients suffering from otitis media. These findings confirm that an integrated approach enhances the accuracy and reliability of identifying ETD compared to the use of a single method.Video endoscopy of the nasal cavity and nasopharynx provided real-time visualization of the anatomical and pathological conditions associated with the pharyngeal orifice of the Eustachian tube. Among the 48 children in the study group, 32 (66.6%) showed signs of ETD using endoscopy, which demonstrates high sensitivity in identifying mucopurulent accumulations, adenoid hypertrophy, and structural obstructions. This aligns with the findings of Chen et al. (2021) and Toivonen & Dean (2021), who reported that in-office endoscopic evaluation is particularly beneficial in children due to the anatomical differences in the Eustachian tube, including its shorter length, more horizontal orientation, and the presence of lymphoid-rich tubal rollers.Meanwhile, acoustic impedance testing, as a non-invasive functional method, detected ETD in 28 patients (58.3%) within the study group. Although slightly less sensitive than endoscopy, AI remains valuable for assessing middle ear compliance and pressure, providing insight into the functional integrity of the Eustachian tube. The prevalence of abnormal tympanograms (types B and C) in this group supports earlier findings that children with otitis media often exhibit negative pressure or effusion in the middle ear (Swarts et al., 2016; Mandel et al., 2016).Importantly, both diagnostic tools revealed concordant positive findings in 26 patients (54.1%), while 8 patients showed negative results in both tests. This overlap emphasizes the complementary nature of these techniques: while endoscopy excels at revealing anatomical obstructions (e.g., adenoids, mucus), AI is instrumental in detecting functional impairments (e.g., poor pressure equalization). In this context, the specificity and sensitivity of each method should not be viewed in isolation, but rather as part of a multimodal assessment strategy.The control group data further reinforce this argument. Only 2 of 20 healthy children exhibited abnormal findings on endoscopy and 5 on AI, suggesting that both tools have high specificity in the absence of middle ear pathology. However, the slight discrepancy between the endoscopic and AI findings in the control group may reflect subclinical or transient ET dysfunction that warrants follow-up, particularly in high-risk populations.A noteworthy finding of the study is the relationship between the degree of adenoid hypertrophy and the presence of ETD. Grade II and III adenoids were prevalent among those with confirmed ET dysfunction, a finding consistent with prior studies (Ma et al., 2020; Juszczak & Loftus, 2020). These vegetations can mechanically obstruct the pharyngeal opening of the tube, especially in children, whose anatomical predisposition—low pharyngeal orifice placement and narrower lumen—amplifies the impact of even modest lymphoid hypertrophy.Furthermore, the study highlights the morphological and developmental characteristics of the Eustachian tube in children that contribute to their susceptibility to dysfunction and middle ear pathologies. These include the linear bone-cartilage junction, rich lymphoid tissue around the tubal opening, and the tube's horizontal alignment in early childhood. Such developmental factors underscore the necessity of age-appropriate diagnostic tools and therapeutic strategies.In clinical practice, the findings advocate for a routine dual-assessment protocol for children presenting with symptoms of otitis media or suspected ETD. Timely identification of dysfunction through this dual approach can facilitate more effective interventions, such as decongestant therapy, adenoidectomy, or myringotomy, and potentially reduce the risk of chronic complications and hearing loss.In conclusion, this study substantiates the importance of integrating anatomical (endoscopic) and physiological (impedance) diagnostics in assessing ETD. Such a combined approach allows for a more nuanced understanding of the disease process and supports evidence-based clinical decision-making in pediatric otolaryngology. Further studies with larger cohorts and longitudinal follow-up are recommended to assess the prognostic value of these diagnostic modalities and their role in monitoring treatment efficacy.
5. Conclusions
- The present study provides strong evidence for the clinical value of combining video endoscopy and acoustic impedance audiometry in diagnosing Eustachian tube dysfunction in children with otitis media. The findings demonstrate that neither method alone offers complete diagnostic coverage; rather, their integration significantly enhances the identification of both anatomical and functional abnormalities. This is especially important in pediatric patients, where early and accurate diagnosis is crucial to prevent chronic complications such as hearing loss, speech delays, and academic difficulties.Video endoscopy revealed pathological changes consistent with ETD in 66.6% of the study group, highlighting its strength in visualizing adenoid hypertrophy, mucosal edema, and structural anomalies at the pharyngeal orifice. These visual findings are essential for evaluating the direct causes of obstruction and for determining the need for surgical interventions like adenoidectomy. The endoscopic examination also allowed for dynamic assessment of Eustachian tube patency through observation of the tubal ridge’s mobility and mucosal condition during voluntary swallowing, providing a functional perspective alongside anatomical insights.Acoustic impedance audiometry identified abnormal tympanograms in 58.3% of the same group, demonstrating its efficacy in detecting negative pressure or effusion in the middle ear cavity, which are indirect but reliable markers of Eustachian tube dysfunction. Although slightly less sensitive than endoscopy in this cohort, tympanometry has the advantage of being non-invasive, easily repeatable, and applicable in outpatient and primary care settings.The comparative analysis of results from the control group—comprising children without clinical ENT pathology—further supports the diagnostic specificity of both methods. The high concordance between negative endoscopy and normal tympanograms in healthy children reinforces their combined utility in ruling out disease, reducing the likelihood of overdiagnosis or unnecessary treatment.A critical contribution of the study lies in its attention to the developmental anatomical differences of the pediatric Eustachian tube. The shorter, more horizontally positioned auditory tube, abundant lymphoid tissue, and immature mucociliary function contribute to a higher risk of obstruction and middle ear pathology in children. These anatomical predispositions not only justify the need for routine assessment in symptomatic patients but also support preventive screening in high-risk groups.Moreover, the correlation between the severity of adenoid hypertrophy and the prevalence of ETD underscores the importance of including endoscopic examination in standard pediatric otolaryngologic evaluations. In many cases, adenoid enlargement, particularly Grades II and III, acts as a mechanical barrier to tube ventilation, reinforcing the necessity for targeted surgical or medical management based on objective diagnostic criteria.The study’s results suggest that dual-modality diagnostics not only improve detection rates but also facilitate earlier and more accurate clinical decisions, leading to more personalized and effective treatment plans. The data emphasize that timely identification of Eustachian tube dysfunction through combined visual and functional methods could reduce the frequency of recurrent otitis media, decrease the need for repeated antibiotic use, and potentially avoid surgical interventions like tympanostomy tube placement in a subset of patients.In conclusion, the integration of video endoscopy and acoustic impedance measurement provides a comprehensive, accurate, and clinically applicable strategy for the diagnosis of Eustachian tube dysfunction in pediatric patients. These tools complement each other by addressing both the structural and functional dimensions of ETD. Their combined use not only enhances diagnostic confidence but also supports more effective management of middle ear diseases, ultimately contributing to improved auditory health, quality of life, and developmental outcomes in children. These findings strongly advocate for their inclusion in standardized diagnostic protocols and warrant further research in larger, multicenter populations to refine their application and assess long-term clinical impact.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML