-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2322-2327
doi:10.5923/j.ajmms.20251507.50
Received: Apr. 28, 2025; Accepted: May 22, 2025; Published: Jul. 23, 2025

Our Method of Surgical Treatment of Patellar Chondromalacia
Irismetov M. E.1, Shamshimetov D. F.2, Irismetov D. M.2, Tadjinazarov M. B.2, Rustamov F. R.2
1Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Tashkent, Uzbekistan
2Sport Travma, Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Tashkent, Uzbekistan
Correspondence to: Irismetov D. M., Sport Travma, Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Patellofemoral pain syndrome is one of the most frequent symptom complexes encountered in the reception of traumatologists, neurologists, rehabilitation specialists, medical physical culture specialists, and sports medicine specialists. With the development of Ortho biology, interest in regenerative medicine increases. Subchondral use of PRP therapy in chondromalacia of the patella is completely unexplored. We conducted arthroscopic diagnosis and treatment of 159 patients between 2020 and 2024, of whom 113 (71.1%) were women and 46 (28.9%) were men. The average age of patients was 50.4±7.3 years. The patients were divided into two groups. First control group, 86 (54.1%) patients, second main group consisted of 73 patients (45.9%), all patients underwent lavage and knee joint debridement, mobilized the lateral edge of the patella, and released the outer retainer. To stabilize, the ablation of the weighted part of the knee joint surface was performed. The same operation and subchondral plasma lifting were performed in the main group. Before surgery, 1, 3, 6, and 12 months after surgery, the knee joint was assessed using the IKDC and VAS scales. Patients were subjected to radiography, ultrasound, knee joint MRI before surgery, and controlled knee joint MRI after surgery. The patients of the main group showed good results in the near term according to the ICDS scale (78,4±5,2-80,3±6,5). In the long term, very good results were obtained (88.5±8.5). In this case, similar results were also noted on the VAS scale (1.5±0.1-1.0±0.18). The lavage and debridement of the entire joint and especially the outer fascia, as well as the mobilization of the lateral edge of the patella and the release of the outer retainer, ensure the mobile and free movement of the patella, thereby reducing inflammatory changes.
Keywords: Patellar chondromalacia, Patellofemoral pain syndrome, Platelet-Rich Plasma
Cite this paper: Irismetov M. E., Shamshimetov D. F., Irismetov D. M., Tadjinazarov M. B., Rustamov F. R., Our Method of Surgical Treatment of Patellar Chondromalacia, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2322-2327. doi: 10.5923/j.ajmms.20251507.50.
1. Introduction
- The patella is the largest sesamoid bone in the body, and its articular surface is covered with thick cartilage. The patella engages with the femoral groove at approximately 10-15 degrees of flexion and remains engaged throughout the entire range of knee flexion [1].Articular cartilage is a highly specialized connective tissue with biophysical properties that enable it to withstand high compressive loads. The biochemical properties and structure of the macromolecular components of the cartilage matrix, along with their interaction with water molecules, are key factors determining the shock-absorbing properties of the tissue [2,3].Chondromalacia is a disease of the hyaline cartilage that covers the articular surfaces of bones. It leads to softening and subsequent rupture, cracking, and erosion of the hyaline cartilage. Most often, it affects the mechanism of knee joint extension and, accordingly, is often called chondromalacia patellae, patellofemoral syndrome, or "runner's knee." The lower surface of the patella is covered with hyaline cartilage, which articulates with the femoral groove covered with hyaline cartilage (trochlear groove). Post-traumatic injuries, microtraumas, wear and tear, and iatrogenic drug injections can lead to the development of chondromalacia [4].Women are more susceptible to this condition than men, which is attributed to the increased Q-angle in women. Apparently, there are no hormonal causes for this disease. Chondromalacia is more common in active young people who engage in running, or in workers who increase the load on the patellofemoral joint by frequently climbing stairs and/or kneeling [5].Treatment of patients with chondromalacia patellae is a complex task, as there is no single universally accepted form of treatment that would be considered the standard of care. Treatment should be based on the results of a medical examination. It may include patellar braces, physiotherapy to strengthen the quadriceps femoris muscle, orthopedic insoles that reduce foot pronation, and non-steroidal anti-inflammatory drugs. Sometimes, platelet-rich plasma (PRP) therapy is recommended, but this is not a standard of care. It has not been proven that PRP therapy consistently improves patients' condition. Similarly, some authors recommend prolotherapy, but it is not a standard treatment and has not proven its effectiveness [4].Despite the existence of several effective surgical methods, the patient's age and severity of the condition should be taken into account when selecting the most appropriate approach. Each method has its own advantages, indications, and limitations. Available techniques include patellar excision, cartilage removal, drilling, tibial tuberosity osteotomy, tibial tuberosity anteversion and elevation, partial or complete patellectomy, proximal soft tissue repair, and distal patellar bone repair. The most effective and straightforward procedure that avoids fibrosis and dysfunction of the quadriceps femoris muscle is medial realignment of the patellar tendon with lateral release and tensioning of the medial portion of the quadriceps femoris muscle [8].Patella replacement. The McKeever prosthesis initially showed positive long-term effects in cases of severe patellar chondromalacia with progressive patellofemoral osteoarthritis; however, this procedure was abandoned due to numerous complications, such as patellar tendon damage, secondary patellar fracture, avascular necrosis, patellofemoral joint instability, and prosthesis loosening [9,15].Cellular therapy. [16,17]. The first report of autologous chondrocyte implantation for the treatment of cartilage defects in knee osteoarthritis was published in 1994 [18]. Over the past two decades, cellular therapy for osteoarthritis has become one of the established treatment methods. Many experts consider chondromalacia patellae to be a mesenchymal disorder; therefore, cellular therapy may have a positive therapeutic effect. New treatment approaches include autologous chondrocyte transplantation and mesenchymal stem cell injections.For many years, arthroscopic mechanical debridement has demonstrated successful symptom relief by removing damaged and unstable cartilage to create a stable edge [19]. However, mechanical shavers can also have a "tearing" effect on the cartilage, posing a significant risk of iatrogenic damage to adjacent healthy cartilage and subsequent progression of the lesion [21,22]. Radiofrequency (RF) knee arthroplasty (ablation) has been proposed as a safe method to address the drawbacks associated with mechanical shaver use [21]. Previous studies have shown that using radiofrequency ablation can make the cartilage surface smoother, limit damage to surrounding healthy cartilage, and potentially reduce the frequency of iatrogenic injuries, in addition to shortening operation time and reducing intra-articular bleeding, which are its main advantages [22]. With the advent of radiofrequency energy for chondroplasty, both monopolar and bipolar systems have been incorporated into instrument development [23]. It has been demonstrated that bipolar radiofrequency systems can penetrate 78-92% deeper than monopolar frequency systems [24]. During radiofrequency procedures, surgeons generally fear chondrotoxic thermal damage, postoperative chondrolysis, and osteonecrosis of the adjacent subchondral bone [21,22,25].Previous studies have evaluated the effects of bipolar and monopolar radiofrequency devices in vitro, although reports on in vivo effects and clinical outcomes are still relatively scarce [24]. The authors suggested that radiofrequency ablation leads to improved clinical outcomes with low rates of complications and repeat surgeries [26].Objective. To improve the results of surgical treatment methods for grade II-III chondromalacia of the patella by optimizing and enhancing arthroscopic chondroplasty. To improve the results of surgical methods of treatment of II-III degree of chondromalacia of the patella by optimizing and improving arthroscopic chondroplasty.
2. Materials and Methods
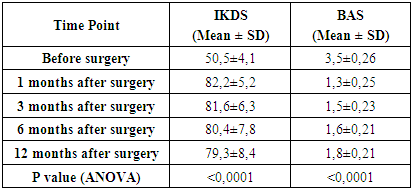
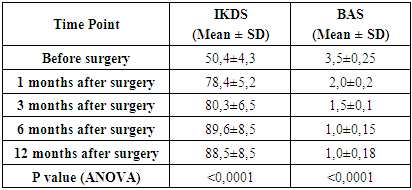
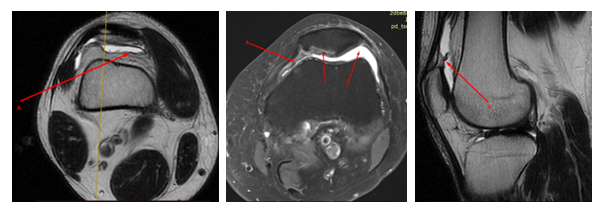
- In the Department of Sports Trauma at the Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, we conducted arthroscopic diagnosis and treatment of 159 patients between 2020 and 2024, of whom 113 (71.1%) were women and 46 (28.9%) were men. Among the patients, 46 were under 18 years old, 17 were 19 to 30 years old, 14 were 31 to 40 years old, 30 were 41 to 50 years old, and 52 were 51 to 60 years old. The patients were divided into two groups. In the first control group, 86 (54.1%) patients underwent lavage and debridement of the knee joint, mobilization of the lateral edge of the patella, and release of the external retainer. In order to stabilize, the hanging part of the articular surface of the patella was ablated.The second main group consisted of 73 patients (45.9%) who had unfavorable results of conservative treatment and grade I-II-III chondromalacia. They performed lavage and debridement of the knee joint, mobilization of the lateral edge of the patella, and release of the external retainer. In order to stabilize, the hanging part of the articular surface of the patella was ablated. Subchondral plasm lifting was also performed.The main complaints of most patients were aching or colicky pain in the knee joint, which intensified with physical exertion and changes in weather, as well as difficulty walking on uneven surfaces and stairs. The pains were sometimes diffuse, without clear localization.Patients underwent radiography in three projections: frontal, sagittal, and axial. Ultrasound of the knee joint was performed using linear or convex transducers with a frequency of 5 to 10 MHz, while the leg was bent at the knee to 50°-60°-90°, with the transducer positioned over the joint space. Magnetic resonance imaging of the knee joint was also performed with 3 mm slices and a 1.5 Tesla magnetic field. MRI results were obtained in 3 planes: axial, coronal, and sagittal, and included T1 and T2 sequences, which identified grade II-III chondromalacia patellae (Fig. 1) and pathological patellar plicas (Fig. 2).
 | Figure 1. A, B - MRI image of grade II-III chondromalacia foci in the patella |
 | Figure 2. A, B - MRI image of the pathological patellar fold |
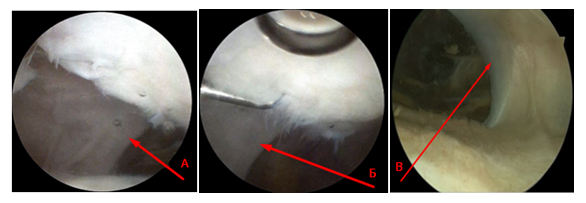 | Figure 3. A, B, C - Arthroscopic view of pathological folds of the patella |
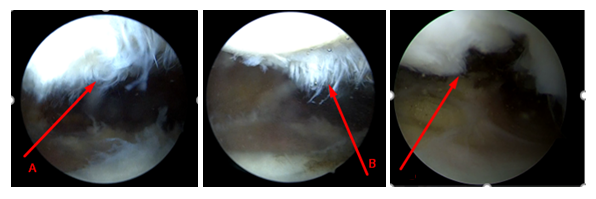 | Figure 4. А, B, C – Arthroscopic view of patellar chondromalacia |
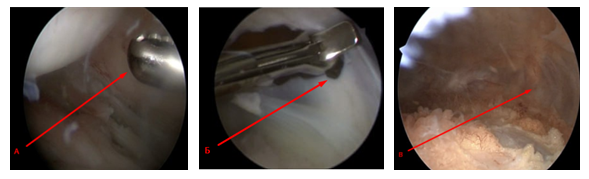 | Figure 5. A, B, C - Arthroscopic view of the lateral facet debridement and release of the lateral patellar retinaculum |
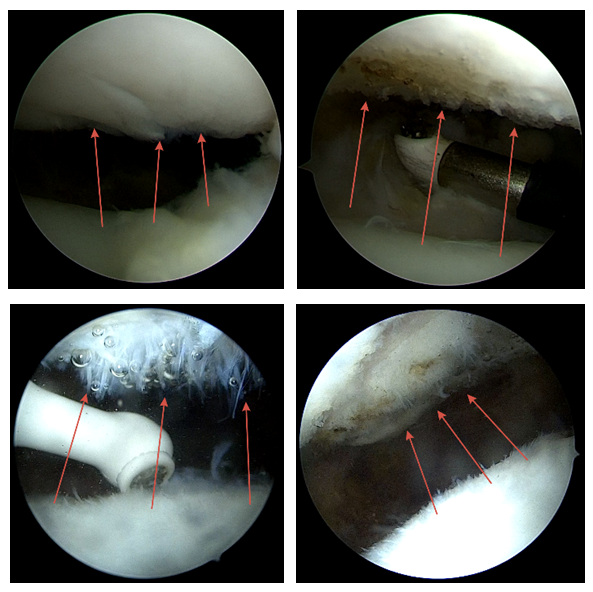 | Figure 6. A, B, C, D - Arthroscopic view of the ablation of the suspended portion of the patellar articular surface |
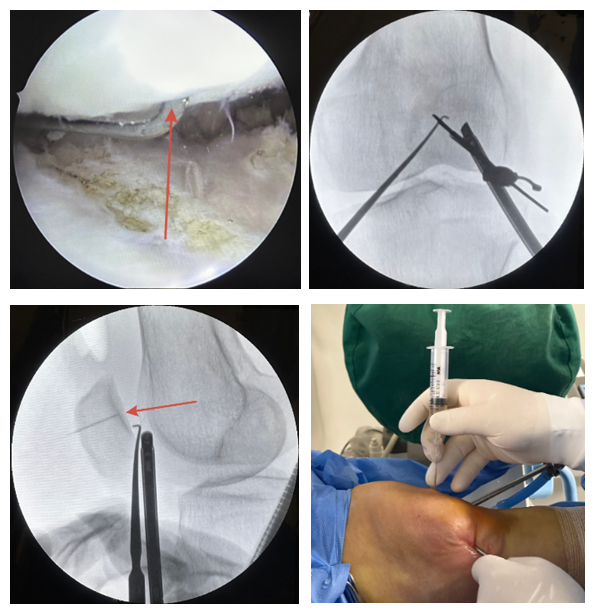 | Figure 7. Image of subchondral plasma lifting of the patella |
3. Results and Discussion
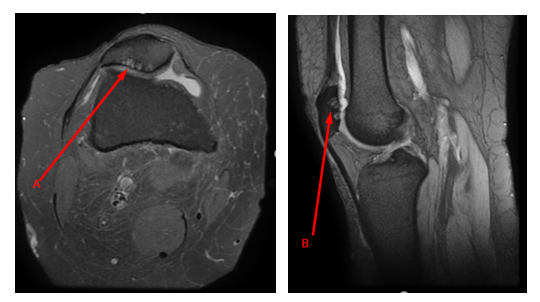
- Our proposed method of chondroplasty for the articular surface of the patella includes the elimination of cartilage defects. The method demonstrated successful symptom relief by stabilizing the damaged and unstable cartilage with the formation of a stable edge. Radiofrequency ablation makes the cartilage surface smoother, limits damage to surrounding healthy cartilage, and potentially reduces the frequency of iatrogenic injuries. Additionally, it shortens operation time and reduces intra-articular bleeding, which are its main advantages.All patients underwent early postoperative rehabilitation measures according to a prescribed scheme following chondroplasty of the articular surface of the patella. The average duration of the rehabilitation process was 2-3 months. The average time to return to sports activities was 3-4 months.At 1-, 3-, 6-, and 12-months post-surgery, the knee joint was evaluated using the IKDC and VAS scales (Table 1,2).
|
|
4. Conclusions
- Our proposed method of chondroplasty of the patellar articular surface using a low-frequency ablator demonstrated advantages in reducing pain syndrome by stabilizing the damaged and unstable cartilage, forming a stable edge and a smoother cartilage surface.Despite the obtained results and the proven effectiveness and safety of subchondral PRP administration in treating grade II-III patellar chondromalacia, we consider it necessary to conduct further research to study this pathology.Our performed lavage and debridement of the entire joint, especially the lateral facet, as well as mobilization of the lateral patellar edge and release of the lateral retinaculum, ensured mobile and free movement of the patellar articular surface, thereby reducing inflammatory changes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML