-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2316-2321
doi:10.5923/j.ajmms.20251507.49
Received: Jun. 29, 2025; Accepted: Jul. 17, 2025; Published: Jul. 19, 2025

Efficacy of Posterior Pericardiotomy in the Prevention of Postoperative Atrial Fibrillation in Patients Undergoing Off-Pump Coronary Artery Bypass (OPCAB)
Ogabek O. Zhabbarov1, Guzal U. Mullabaeva2, Islam M. Sharipov3, Xurshid G. Fozilov4
1Junior Researcher of Mini-invasive Cardiosurgery Department of Republican Specialized Scientific and Practical Medical Center of Cardiology, Tashkent, Uzbekistan
2Scientific Director of Mini-invasive Cardiosurgery Department of Republican Specialized Scientific and Practical Medical Center of Cardiology, Tashkent, Uzbekistan
3Head of Mini-invasive Cardiosurgery Department of Republican Specialized Scientific and Practical Medical Center of Cardiology, Tashkent, Uzbekistan
4Director of Republican Specialized Scientific and Practical Medical Center of Cardiology, Tashkent, Uzbekistan
Correspondence to: Xurshid G. Fozilov, Director of Republican Specialized Scientific and Practical Medical Center of Cardiology, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

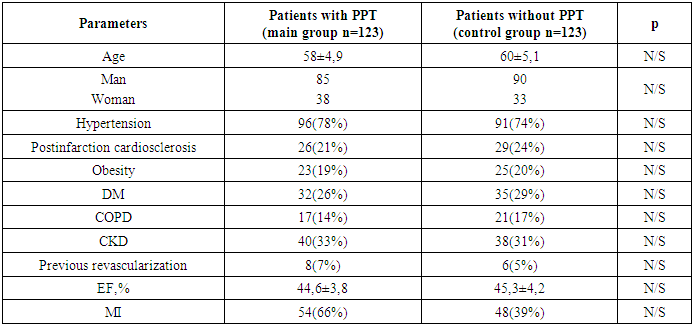
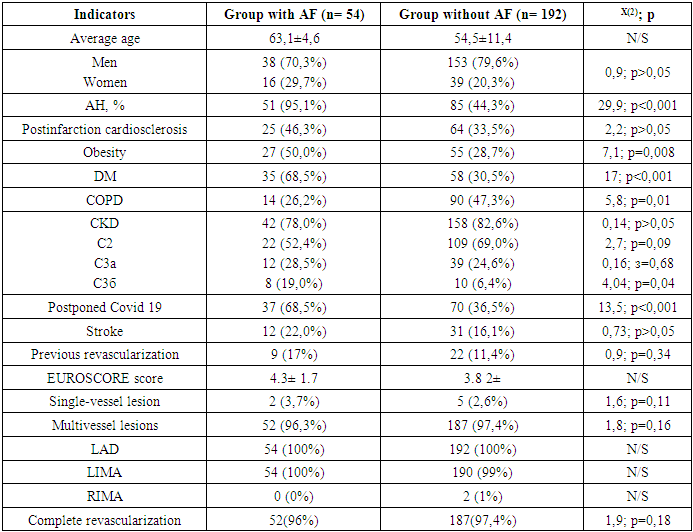
Background: Postoperative atrial fibrillation is a common postoperative complication of cardiac surgery. Its incidence ranges from 30 to 40% after off-pump coronary artery bypass. Although it is a benign problem and well tolerated, it can be life threatening with significant morbidity and mortality. The aim of the study: to evaluate the effectiveness of the pericardiotomy procedure in reducing the incidence of postoperative AF in patients undergoing off-pump coronary bypass grafting surgery. Materials and methods: 246 patients with CHD and indications for coronary artery bypass (OPCAB) were included in the study. The mean age of the patients was 58.6±17.2 years, 55 women and 191 men. By randomization method all patients were divided into 2 groups depending on the addition of posterior pericardiotomy (PPT) to the operation: Group I - 123 patients who underwent PPT, Group II (control group) - 123 patients without addition of PPT to coronary artery bypass surgery. Results: According to the results of the monitoring 54 patients developed POAF after CABG, which amounted to 22.0% of the total number of patients. According to the monitoring data POAF developed in 16(13%) patients of group I and in 38(31%) patients of group II (p<0,05). Analysis of clinical and anamnestic parameters revealed the following. In the studied groups the patients did not differ by age and gender (Table 1). Hypertension (HD) was more frequently registered in the group with POAF and amounted to 95.1% versus 44.3% in the group without POAF (χ2=29.9; p<0.001). Also, patients in the POAF group were frequently obese than in the group without POAF (χ2=7.1; p=0.008). Diabetes mellitus (DM) was also significantly more frequent in patients with POAF, 68.5% vs. 30.5% (χ2=17; p<0.001). (Table 2). Conclusion: Postoperative atrial fibrillation after coronary bypass gafting, according to our results, was observed in 54 (22%) patients. In the first group, 16 (13%) patients developed POAF and in the second group, 38 (31%) patients developed POAF. These data show the frequency of POAF development on the control group is 22 (18%) more than the main group. It is shown that POAF is a poly etiologic disease in its development contributes to many factors, as well as the process of fibrosis in the myocardium, which was confirmed by the highest incidence of postoperative atrial fibrillation in patients with AH, DM, obesity.
Keywords: OPCAB-Off-Pump Coronary Artery Bypass, POAF-Postoperative Atrial Fibrillation, HM ECG-Holter monitoring, DM-Diabetes Mellitus, CKD-Chronic kidney disease, COPD-Chronic obstructive pulmonary disease, DM-Diabetes Mellitus, PVCs-Premature ventricular contractions, SVES-Supraventricular extrasystole, MIDCABG-Minimally invasive aortocoronary bypass surgery, ECMO-Extracorporeal Membrane Oxygenation, IABP-Intra-aortic balloon counterpulsation
Cite this paper: Ogabek O. Zhabbarov, Guzal U. Mullabaeva, Islam M. Sharipov, Xurshid G. Fozilov, Efficacy of Posterior Pericardiotomy in the Prevention of Postoperative Atrial Fibrillation in Patients Undergoing Off-Pump Coronary Artery Bypass (OPCAB), American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2316-2321. doi: 10.5923/j.ajmms.20251507.49.
Article Outline
1. Introduction
- Postoperative atrial fibrillation is a common postoperative complication of cardiac surgery, occurring in 17-47% of patients. Its incidence ranges from 30 to 40% after coronary bypass grafting (CABG), after valve replacement or plasty this rate increases to 50% after combined procedures. It usually occurs within 1-5 days after surgery, with peak incidence on the second postoperative day [2]. Although it is a benign problem and well tolerated, it can be life threatening with significant morbidity and mortality. In recent years, the use of such a simple interoperative method as posterior pericardiotomy for the prevention of POAF and cardiac tamponade has been actively discussed. But the wide application of this surgical method in patients with coronary artery pathology, in whom coronary bypass grafting on the working heart (OPCAB) is planned, does not have a sufficient database. It is considered relevant to study the effect of this surgical method on the course of early and midterm periods after CABG [7].
2. Materials and Methods
- This prospective single-center study was conducted at the Republican Specialized Scientific and Practical Medical Center of Cardiology (Tashkent, Uzbekistan). This study was conducted in the period 2022-2025, by completely randomized and blinded selection of patients. The study of the effect of intraoperative posterior pericardiotomy on the incidence of postoperative AF included 246 patients with CHD and indications for CABG. The mean age of the patients was 58.6±17.2 years, 55 women and 191 men. Inclusion criteria: Patients prepared for elective surgery for coronary bypass surgery on the working heart (OPCAB) and written informed consent of the patient to participate in the study. By randomization method, all patients were divided into 2 groups depending on the addition of posterior pericardiotomy (PPT) to surgery: group I - 123 patients who underwent PPT, group II (control) - 123 patients without addition of PPT to coronary bypass grafting surgery.Exclusion criteria: Performance of MIDCABG or MICS CABG, marked adhesions in the pericardium and pleural cavity, repeated cardiac interventions, patient refusal to participate in the study, patients older than >80 years of age, LV aneurysm with thrombosis, severe valvular heart disease, presence of severe chronic kidney disease, liver disease, comorbid pathologies in decompensation stage, constant intake of antiarrhythmic drugs due to ventricular and supraventricular cardiac rhythm disturbances, and a history of AF. All patients underwent ECG Holter monitoring (ECG HM) 5 days and 24 hours before the operation. The patients also underwent the following instrumental and laboratory investigations: CBC, coagulogram, markers of inflammatory processes (C-reactive protein, Anti-O-streptolysin, Interleukin-6, Rheumatoid factor), biochemical analyses, NT-proBNP, electrolytes, Echo and chest X-ray.All patients underwent OPCAB surgery. After the operation, all patients were in the intensive care unit, where the heart rhythm was monitored using a recording bedside monitor, and then on the 3rd and 5th day patients underwent HM ECG. If Atrial Fibrillation or Atrial flutter was detected, patients underwent electrical or drug-induced cardioversion. Short-term outcomes were defined as: hospital mortality, stroke, acute renal failure, and re-hospitalization within one month after surgery. At 6-month follow-up, mortality, incidences of acute myocardial infarction and stroke, and repeat revascularization surgery (CABG or PCI) were evaluated [8].Statistical processing of dataStatistical processing was performed using spreadsheets "Microsoft Excel" and software "Static for Windows" v. 7.0. To assess the factors influencing the development of postoperative atrial fibrillation after aorto-coronary bypass surgery on the working heart, binary logistic regression analysis was performed and the Katz method of risk and odds ratio calculation was applied.
3. Results
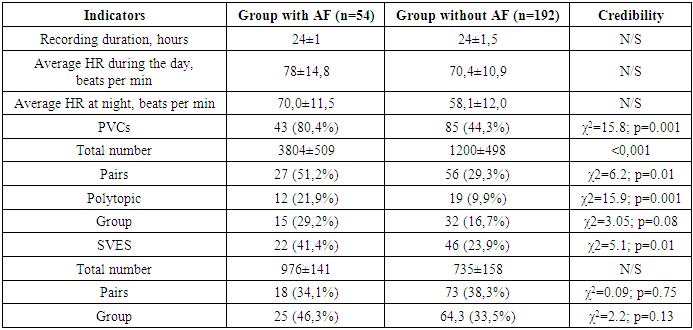
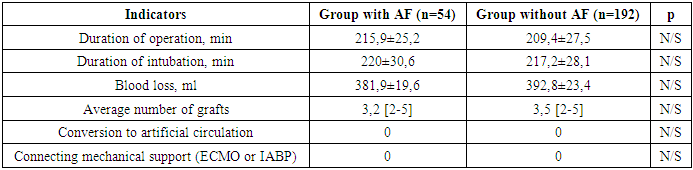
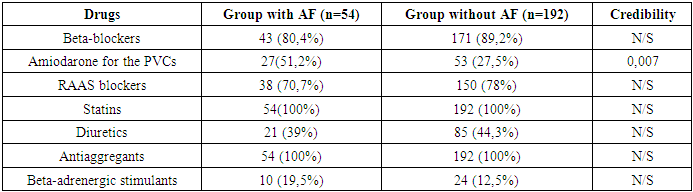
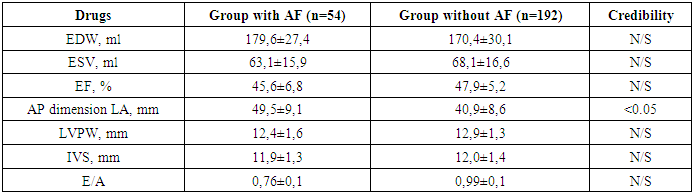
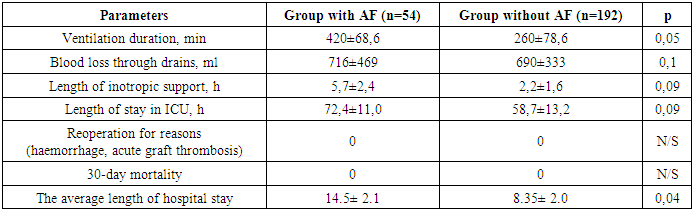
- According to the monitoring data POAF developed in 16(13%) patients of group I and 38(31%) patients of group II (p<0.05). According to the study data POAF developed in 54(22%) patients from the total number of patients. One of the main hypotheses of POAF development is that the fluid accumulated in the oblique pericardial sinus after surgery, in turn, irritates the posterior wall of the left atrium, causing cardiac rhythm disturbances. No established drainage system can evacuate blood from this area. The analysis of clinical and anamnestic parameters revealed the following: in the studied groups the patients did not differ by age and gender (Table 1). When comparing the groups of patients with and without POAF, we obtained the following results: POAF was more often associated with AH - hypertensive patients prevailed in the group with POAF more often than in the group without POAF 95.1% vs. 44.3% (χ2=29.9; p<0.001). Also, patients in the group of patients with POAF were significantly more likely to be overweight than those in the group without POAF (χ2=7.1; p=0.008). Diabetes mellitus (DM) was also significantly more common in patients with POAF, 68.5% vs. 30.5% (χ2=17; p<0.001). Among other comorbid conditions, the presence of COPD was significant in the development of POAF. It was present in 47.3% of patients in the group without POAF, whereas in the group with POAF it was 26.2% (χ2=5.8; p=0.01). When studying the relationship between chronic kidney disease (CKD) and the risk of POAF, we found that patients with stage 3b CKD predominated in the group with POAF - 19.0% vs. 6.4% (χ2=4.04; p=0.04). Given that many patients had Covid19, we also studied its incidence in the compared groups and found an association between coronavirus infection and the incidence of POAF (χ2=13.5; p<0.001) (Table 2).
|
|
|
|
|
|
|
4. Discussion
- Despite the high prevalence of POAF, there is no consensus on the causes and mechanisms of its development. But, as it is known, there are many causes and mechanisms, and researchers agree on this [9]. It is believed that in each individual case the cause of POAF can be different factors that lead to structural and electrophysiological changes, creating favorable conditions for the initiation and maintenance of atrial fibrillation (AF) [10]. In order to identify the causes of POAF, we selected 246 patients and conducted a prospective study. It was shown that POAF significantly more often developed among male patients, who more often had a history of arterial hypertension, obesity, chronic bronchitis, diabetes mellitus. The groups also differed significantly more often by the frequency of coronary viral infection [12]. In addition, POAF was significantly more frequently observed in the group of patients with chronic kidney disease [11]. Evaluation of the efficacy of posterior pericardiotomy in the prevention of POAF gave a positive result. This method can be used to prevent POFP in a group of patients at high risk of POAF. Our data coincide with the opinion of other researchers (Tao Xiong; Hosam Fawzy). In our opinion, in this category of patients the processes of systemic inflammation and fibrosis are excessively activated. When studying the relationship between cardiac rhythm disturbances and the frequency of POAF, we found that the group with AF was significantly more often affected by PVCs and SVES, which once again confirms the theory of initial myocardial inhomogeneity. Thus, 51.2% of patients and POAF group took amiodarone preoperatively. The study of the peculiarities of intraoperative management of patients with POAF did not reveal any significant differences between the compared groups. When analyzing hemodynamic parameters, we found significant differences in the size of the left atrium. Thus, in the group with POAF, the size of the left atrium was 49.5 mm, whereas in the group without POAF it was 40.5 mm (p<0.05). Also in the early postoperative period in the group with POAF there was noted a prolongation of the duration of ventilation and inotropic cardiac support, but in this group also noted a longer resuscitation period of rehabilitation than the second group without POAF. Thus, our study demonstrated the polyetiological of factors in the development of postoperative AF. Such clinical and anamnestic parameters as sex, arterial hypertension, chronic kidney disease, obesity, and diabetes mellitus made a great contribution, which implies nonspecificity of POAF etiology and requires correction of all commonly known cardiovascular risk factors.
5. Conclusions
- Posterior pericardiotomy during coronary artery bypass grafting (OPCAB) surgery is a simple surgical maneuver that allows to significantly reduce the incidence of AF in the postoperative period, thus significantly improving the results of surgical intervention in this group of patients.
ACKNOWLEDGEMENTS
- The authors are grateful to the Republican Specialized Scientific and Practical Medical Center of Cardiology in Tashkent for support and assistance in conducting the study, as well as to colleagues for their valuable comments and recommendations that contributed to the quality of the work.
Funding Source
- This study did not receive external funding.
Authors' Contributions
- Conceptualization: G.U. and O.O.; Methodology: G.U.; Data collection: O.O.; Data analysis and interpretation: G.U. Mullabaeva and O.O. Zhabbarov; Original text writing: O.O.; Editing: G.U.; Visualization: G.U.; Project administration: O.O. All authors are familiar with and agree with the published version of the manuscript.
Ethical Considerations
- This study was reviewed and approved by the Ethics Commission of Republican Specialized Scientific-Practical Medical Center of Cardiology (No. 3/EC/2022). All participants signed written informed consent prior to inclusion in accordance with ethical standards protecting human subjects.
Informed Consent to Publication
- All study participants provided written informed consent for participation in the study and publication of the results.
Data Availability Statement
- Data supporting the results of this study are available from the authors upon reasonable request.
Conflict of Interest
- The authors declare that there is no conflict of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML