Bekmurodovna Malika Ruzimurod qizi1, Daminov Feruz Asadullaevich2
1Student of the Faculty of Medicine, Samarkand State Medical University, Samarkand, Uzbekistan
2Doctor of Medical Sciences, Associate Professor, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Burn injuries in elderly patients are often accompanied by profound metabolic disturbances and a high risk of complications. This study aimed to evaluate the clinical effectiveness of specialized nutritional support—via parenteral and enteral routes—in patients aged 60 to 80 years with second- and third-degree thermal injuries. Patients were divided into groups based on age, burn severity, and type of nutritional regimen received. Laboratory parameters—including protein metabolism, inflammatory status, and metabolic indicators—along with clinical outcomes were assessed. The analysis showed that targeted nutritional support significantly accelerated recovery and helped reduce the incidence of complications.
Keywords:
Burns, Elderly patients, Nutritional support, Protein metabolism, Laboratory parameters, Clinical effectiveness
Cite this paper: Bekmurodovna Malika Ruzimurod qizi, Daminov Feruz Asadullaevich, The Role of Nutritional Support in Burn Injuries Among Elderly Patients: Metabolic Aspects and Clinical Effectiveness, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2309-2311. doi: 10.5923/j.ajmms.20251507.47.
1. Introduction
Elderly burn patients represent a special category with a high risk of mortality, metabolic disturbances, and complications. Aging is accompanied by reduced physiological reserves, altered immune responses, and decreased stress tolerance. Nutritional support, as a component of comprehensive therapy, becomes especially important in the treatment of such patients. The present study focuses on evaluating the metabolic and clinical effects of specialized nutrition in elderly patients with burn injuries.Aim of the Study: To assess the metabolic aspects and clinical effectiveness of specialized nutritional support in elderly patients (aged 60–80 years) with second- and third-degree burns.
2. Materials and Methods
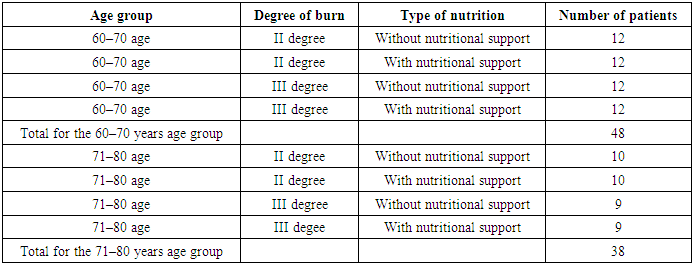
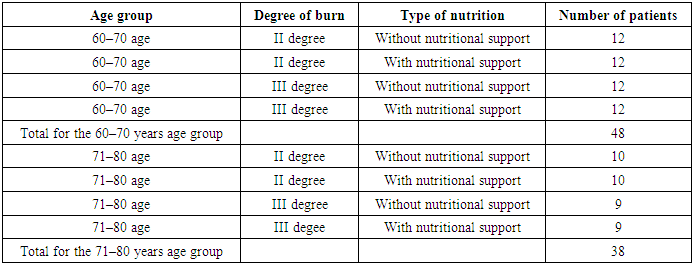
The study included patients admitted to the Department of Combustiology at the Samarkand Branch of the Republican Scientific Center for Emergency Medical Care from August 1, 2024, to February 20, 2025. A total of 86 patients aged 60 to 80 years with second- and third-degree burns were enrolled. Patients were divided into two age groups: 60–70 years (n=48) and 71–80 years (n=38). Within each age group, patients were further stratified based on burn severity and type of nutritional support: standard nutrition and specialized nutritional support (Table 1).Table 1. Stratification Structure
 |
| |
|
Laboratory and Clinical Assessments: All patients underwent the following laboratory tests: complete blood count (hemoglobin, leukocytes, ESR), urinalysis, and blood biochemistry including total protein, albumin, prealbumin, glucose, urea, creatinine, electrolytes (Na⁺, K⁺, Cl⁻, Ca²⁺), and C-reactive protein (CRP).Clinical indicators included: length of hospitalization, frequency of infectious complications, wound healing dynamics, and the need for surgical intervention.
3. Study Results
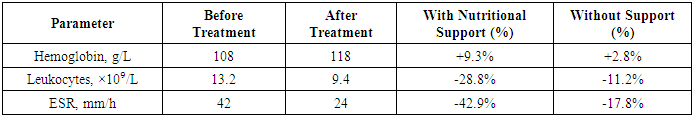
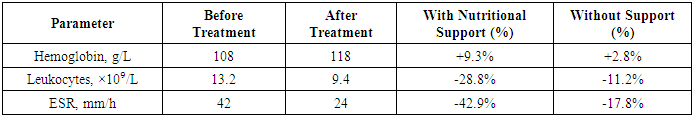
The complete blood count showed the following outcomes. Hemoglobin levels increased by 9.3% in the group receiving nutritional support, indicating recovery of hematopoiesis and correction of anemia. In the control group, the increase was minimal. Leukocyte counts significantly decreased in patients receiving nutritional support, reflecting a reduced inflammatory response. ESR also showed a marked decrease, especially in the nutritional support group (from 42 to 24 mm/h), confirming the anti-inflammatory effect (Table 2).Table 2
 |
| |
|
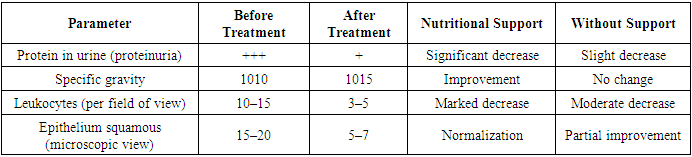
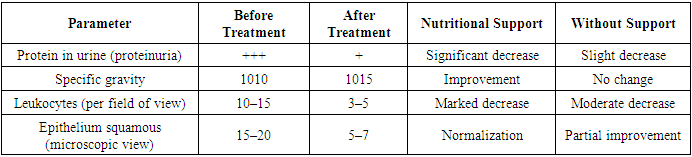
Urinalysis Findings: The following changes were observed in the general urinalysis. A reduction in proteinuria and normalization of the cellular composition of the urinary sediment were noted in the group receiving nutritional support. An increase in urine specific gravity was observed, which may indicate the restoration of the kidneys' concentrating ability. A decrease in leukocytes and epithelial cells suggests regression of the inflammatory process in the urinary system (Table 3).Table 3
 |
| |
|
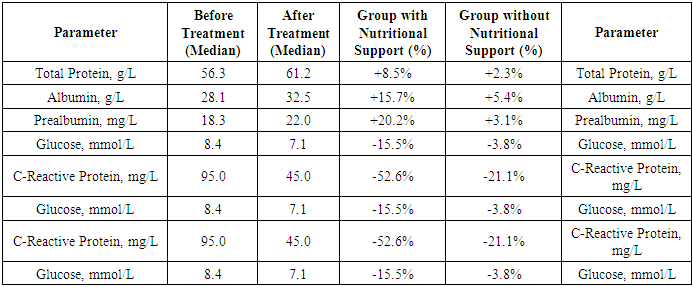
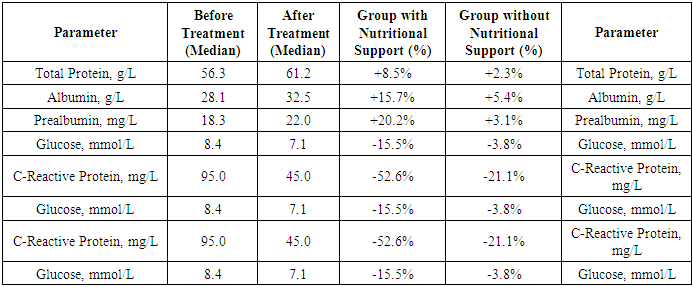
Biochemical Analysis Findings: The biochemical analysis revealed the following changes. In the group receiving nutritional support, a more pronounced increase in total protein levels was observed (+8.5%), indicating better recovery of protein metabolism. In the control group, the increase was only 2.3%.Albumin: A significant increase in albumin levels was noted in the nutritional support group (+15.7%) compared to the control group (+5.4%), confirming an improvement in protein status among patients receiving specialized nutrition.Prealbumin, a sensitive marker of nutritional status, showed a marked improvement in the nutritional support group (+20.2%), whereas the control group exhibited only a modest increase (+3.1%).Glucose: A 15.5% decrease in glucose levels in the nutritional support group may indicate normalization of metabolic processes, while the control group showed a decrease of only 3.8%. This may be associated with reduced physiological stress and improved metabolic regulation.CRP: A significant reduction in C-reactive protein (CRP) levels was observed in the nutritional support group (−52.6%), confirming the anti-inflammatory effect of nutritional intervention. In the control group, the reduction was −21.1%.Lactate: A decrease in lactate levels in the nutritional support group (−31.6%) also indicated improved tissue respiration and metabolic adaptation. In the group without nutritional support, the reduction was minimal (−5.2%).Creatinine and Urea: A slight decrease in creatinine and urea levels was seen in the nutritional support group, possibly reflecting improved kidney function and reduced catabolism (Table 4).Table 4. Laboratory tests in patients with burns in different groups
 |
| |
|
Patients receiving nutritional support showed significantly better results in most biochemical parameters, indicating the positive impact of specialized nutrition on metabolism and recovery. The main improvements were observed in protein, albumin, and prealbumin levels, reflecting normalization of protein metabolism and restoration of nutritional reserves. Additionally, a significant reduction in CRP and lactate levels indicated decreased inflammation and improved metabolic status of the patients.
4. Discussion
The results confirm the important role of nutritional support in the treatment of elderly burn patients. Protein-energy deficiency exacerbates the course of burn disease, intensifies catabolism, and worsens outcomes. Nutritional intervention helps stabilize metabolism, accelerates tissue regeneration, and reduces the risk of complications. It is also important to consider age-related metabolic characteristics and tailor nutrition to individual needs.
5. Conclusions
The results of this study convincingly demonstrate that nutritional support plays a key role in correcting metabolic disturbances in elderly patients with second- and third-degree burns. Patients receiving specialized nutrition showed significant improvement in protein metabolism markers (total protein, albumin, prealbumin), reduction in inflammatory markers (CRP, leukocytes, ESR), and normalization of glycemic and renal profiles. Clinically, this was accompanied by faster wound healing, reduced complication rates, and overall improvement in patient condition. Thus, incorporating nutritional support into the comprehensive treatment of burn disease in elderly patients should be considered not as an auxiliary measure but as a necessary therapeutic component that enhances inpatient care effectiveness and improves prognosis.
References
| [1] | Arutyunov AG, Martynov AI. Klinicheskoe pitanie v reanimatologii i intensivnoi terapii [Clinical nutrition in resuscitation and intensive care]. Moscow: GEOTAR-Media; 2021. 288 p. Russian. |
| [2] | Barinova IA. Pitательная podderzhka pri ozhogovoi bolezni [Nutritional support in burn disease]. Voprosy pitaniya. 2020; 89(4): 52-59. Russian. |
| [3] | Berezhnoy VV, Kuzmin SA. Pitanie v khirurgii i intensivnoi terapii [Nutrition in surgery and intensive care]. St Petersburg: SpetsLit; 2019. 336 p. Russian. |
| [4] | Vishnyakova EA. Osobennosti metabolizma pri ozhogovoi travme u pozhilykh patsientov [Metabolic features in burn trauma in elderly patients]. Vestnik khirurgii. 2021; (3): 15-21. Russian. |
| [5] | Gromova OA, Kuznetsova OA. Biokhimiya vospaleniya i metabolizma pri ozhogakh [Biochemistry of inflammation and metabolism in burns]. Moscow: MEDpress-inform; 2020. 240 p. Russian. |
| [6] | Zhukov VY. Nutritivnaya podderzhka v gerontologii [Nutritional support in gerontology]. Geriatriya. 2020; (2): 38-45. Russian. |
| [7] | Ivanov DA, Soloviev VV. Rol belkovogo pitaniya v vosstanovlenii patsientov s ozhogami [Role of protein nutrition in recovery of burn patients]. Plasticheskaya khirurgiya i kosmetologiya. 2022; (1): 20-25. Russian. |
| [8] | Kalinin AP. Sovremennye podkhody k metabolicheskoi podderzhke pri tyazhelykh travmakh [Modern approaches to metabolic support in severe trauma]. Moscow: Meditsina; 2020. 192 p. Russian. |
| [9] | Klimanov IA, Shprah VV. Klinicheskoe pitanie u patsientov pozhilogo vozrasta [Clinical nutrition in elderly patients]. St Petersburg: Elbrus; 2021. 214 p. Russian. |
| [10] | Kopanev YA. Gipermetabolizm pri ozhogakh: patogenez i korrektsiya [Hypermetabolism in burns: pathogenesis and correction]. Ozhogovaya bolezn. 2020; (4): 10-16. Russian. |
| [11] | Kurashvili AE. Nutritivnaya podderzhka v intensivnoi terapii [Nutritional support in intensive care]. Moscow: Litterra; 2022. 306 p. Russian. |
| [12] | Levin BA. Pitanie pri kriticheskikh sostoyaniyakh [Nutrition in critical conditions]. Moscow: Praktika; 2019. 250 p. Russian. |
| [13] | Petrova MA. Preal’bumin kak marker nutritivnogo statusa [Prealbumin as a marker of nutritional status]. Klinicheskaya laboratornaya diagnostika. 2021; (6): 32-36. Russian. |
| [14] | Sidorov AY. Pitательная podderzhka v gerontologicheskoi praktike [Nutritional support in gerontological practice]. Novosibirsk: SibMedIzdat; 2021. 180 p. Russian. |
| [15] | Trofimov SN. Otsenka laboratornykh pokazatelei pri ozhogakh [Assessment of laboratory parameters in burns]. Laboratornaya meditsina. 2022; (3): 17-22. Russian. |
| [16] | Yarovaya NI. Sravnitel’nyi analiz enteral’nogo i parenteral’nogo pitaniya u pozhilykh [Comparative analysis of enteral and parenteral nutrition in the elderly]. Vrach. 2020; (8): 41-44. Russian. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML