-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2300-2302
doi:10.5923/j.ajmms.20251507.45
Received: Jun. 5, 2025; Accepted: Jul. 3, 2025; Published: Jul. 19, 2025

Risk Factors for the Development of Febrile Seizures in Children and Their Transition to Febrile Seizures
Gafforova Visola Furkatovna, Xodjiyeva Dilbar Tadjiyevna, Rahmatov Alizot Axtam ogli
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Gafforova Visola Furkatovna, Bukhara State Medical Institute, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Febrile seizures (FS) are the most common type of acute symptomatic seizures in young children. Despite the favorable prognosis in most cases, in some patients they transform into febrile convulsive syndromes, including epilepsy. The purpose of this work is to analyze the risk factors for the development of FS and their transition to afebrile seizures. The genetic, clinical and neurophysiological predictors of an unfavorable course are indicated. An important role in the occurrence of this disease in children is played by perinatal factors, in particular, cerebral hypoxia, developmental abnormalities, genetic determinations, as well as anatomical and physiological features of the child's brain, which, in certain pathological conditions, are prone to high convulsive activity and excitability of the brain, even with the smallest metabolic changes occurring in the child's body.
Keywords: Febrile seizures, Epilepsy, Children, Risk factors, Prognosis, EEG, Neurodevelopment
Cite this paper: Gafforova Visola Furkatovna, Xodjiyeva Dilbar Tadjiyevna, Rahmatov Alizot Axtam ogli, Risk Factors for the Development of Febrile Seizures in Children and Their Transition to Febrile Seizures, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2300-2302. doi: 10.5923/j.ajmms.20251507.45.
Article Outline
1. Introduction
- Febrile seizures (FS) occur in 2-5% of children aged 6 months to 5 years. In the vast majority, they are benign and do not require antiepileptic therapy. However, 2-10% of patients may develop afebrile seizures, including various forms of epilepsy.Early detection of risk factors for the transition of FS to epileptic syndrome makes it possible to optimize monitoring, prognosis and, if necessary, early therapy [5].Epileptic syndrome is one of the most urgent problems of pediatric neurology. The frequency of epilepsy in the population is 0.5-0.75% of the child population, and febrile seizures (FS) - up to 5%. About half of all seizures occur before the age of 15, of which the largest number of seizures occur between the ages of 1 and 9 years. The frequent development of seizures in childhood is explained by the peculiarities of the child's nervous system and the variety of causes that cause them [1,4].Febrile seizures often begin with a sudden increase in temperature, which is associated with hypoxia of the brain. It is known that with an increase in body temperature of only 1°C, the intensity of metabolic processes in the brain increases by 7-10%, and hence the need for oxygen. With a gradual increase in temperature, seizures are much less frequent, as there is time for the necessary increase in cerebral blood flow, which prevents hypoxia [1,3,4,6].An important role in the occurrence of this disease in children is played by perinatal factors, in particular, cerebral hypoxia, developmental abnormalities, genetic determinations, as well as anatomical and physiological features of the child's brain, which, in certain pathological conditions, are prone to high convulsive activity and excitability of the brain, even with the smallest metabolic changes occurring in the child's body [2,5].The aim of this study is to systematize the factors associated with an increased risk of FS transformation into afebrile seizures.
2. Materials and Methods
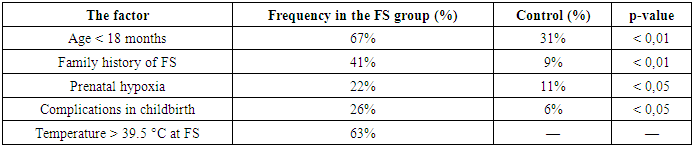
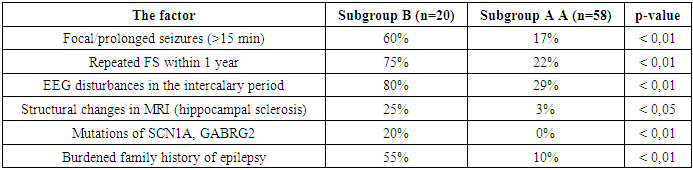
- The analysis was based on data from 78 FS patients (the main group) and 35 healthy children (the control group). Two subgroups are identified among them:• Subgroup A (n=58): children with single/uncomplicated FS, without subsequent transition;• Subgroup B (n=20): children who had afebrile seizures 6-24 months after FS (epilepsy was confirmed in 80% of cases).Methods:• analysis of anamnestic and clinical data;• electroencephalography (EEG) in the intercalary period;• MRI of the brain according to the indications;• Family history;• Genetic screening (including SCN1A and GABRG2).
3. The Results and Their Discussion
- The study examined 78 children under the age of 5 who are in the period of convalescence, i.e. recovery, characterized by the gradual disappearance of FS (up to 5-6 years) and the restoration of normal bodily functions. For several years, children with FS were under supervision, constant monitoring was carried out, recreational activities, periodic checkups, and examinations were carried out.
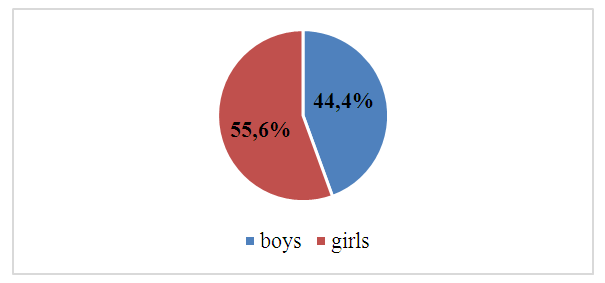 | Figure 1. Analysis of the distribution of children by gender |
|
|
4. Conclusions
- The detection of these signs requires increased monitoring, in-depth examination and, if necessary, early intervention.The analysis of clinical, neurological, neurophysiological, and molecular genetic data made it possible to identify key factors contributing to both the development of febrile seizures in children and their transformation into febrile seizures, including epilepsy.Thus, early identification of risk factors and targeted monitoring of high-risk children makes it possible to timely intervene in a potentially unfavorable scenario of the disease and improve the neurodevelopment and quality of life of patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML