-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2253-2257
doi:10.5923/j.ajmms.20251507.35
Received: Jun. 15, 2025; Accepted: Jul. 3, 2025; Published: Jul. 11, 2025

Early vs. Delayed Surgical Treatment of Complicated Congenital Hand Deformities: A Prospective Study
Nigora Nazarova1, Shukhrat Shamukimov2
1Deparment of Traumatology, Orthopedics and MFS, Tashkent Medical Academy, Tashkent, Uzbekistan
2Republican Center for Pediatric Ortopedics, Tashkent, Uzbekistan
Correspondence to: Nigora Nazarova, Deparment of Traumatology, Orthopedics and MFS, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

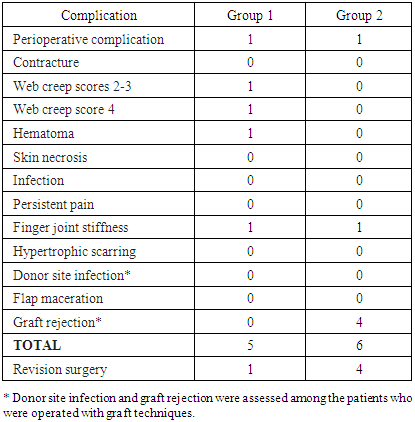
Numerous types of congenital limb differences and anomalies can be surgically corrected. We compared the complexity of surgical interventions and outcomes between early and delayed intervention cases of complex congenital hand deformities. The null hypothesis was that the patient’s age at the time of surgery would not affect the quality of surgical interventions and outcomes. Methods. A prospective single-center study with consecutive cases occurred from May 2012 to May 2022. The study cohort comprised patients presenting for surgical management of isolated and syndrome-affiliated unilateral or bilateral complex forms of congenital hand deformities. They were divided into patients younger than five years (Group 1) and older than five (Group 2). Patients with deformities that involve three or more fingers were included in the study. Results. Altogether, 133 patients (Group 1: n=73, M/F 39/34, mean age 2.8 ± 1.5 years; Group 2: n=60, M/F 32/28, 8.5 ± 3.2 years) were operated and completed follow-up. We operated on 732 fingers on 202 hands in 138 surgeries. Most of the patients had complicated syndactyly, symbrachydactyly, and syndrome-related deformities. Young patients restored their motor and sensory nerve activity during the first six months since surgery, while older patients needed from six to 12 months for complete nerve recovery. One reoperation was needed for a young patient because of web creep, and four reoperations were needed for older patients because of graft rejection. No other significant differences between the two age groups were detected. Conclusion. The timing of surgical treatment of congenital hand deformities is not paramount, and good functional outcomes can be achieved in children of any age.
Keywords: Congenital hand deformities, Pediatrics, Surgery, Symbrachydactyly, Congenital syndromes
Cite this paper: Nigora Nazarova, Shukhrat Shamukimov, Early vs. Delayed Surgical Treatment of Complicated Congenital Hand Deformities: A Prospective Study, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2253-2257. doi: 10.5923/j.ajmms.20251507.35.
Article Outline
1. Introduction
- Congenital hand deformities represent one of the most challenging problems in pediatric orthopedics and cause significant functional, cosmetic, and psychological impairments for patients. In the 1960s-70s, it was agreed that the optimal timing for surgical corrections is between one and two years of age [1]. The issue of choosing the age of patients to start surgical treatment remains controversial, although there are numerous supporters of early interventions. The first two years of life are paramount for developing cerebral cortex patterns of hand use. When surgery is delayed, these patterns will need to be retrained, and the outcome may not be satisfactory [2]. The emerging literature reports that the optimal age for a child to undergo surgical intervention is from three months to two years. The reality is not similarly straightforward [3]. Slevin et al. investigated the timing of surgical release in syndactyly cases in the USA. The mean age of syndactyly release was 3.6 years, but 27.1% of patients underwent release after the age of five years [4]. Other publications reported the age ranges of the operated patients as from 2 months to 3.8 years, 2 to 4 years, 2,5 to 7,3 years, or the average age of 12 years. A review on camptodactyly reported that children of any age from two months to 18 years were operated [5]. Kurebayashi et al. reported that children with syndactyly operated on younger than one year had worse postoperative outcomes than those operated on older than one year. Patients’ age under two years old was considered as a contraindication for syndactyly treatment with external fixation frames [6]. The concept of our research was developed in 2012 while observing children of any age admitted to our institution because of congenital hand deformities. The management of commonly encountered conditions, such as clinodactyly, thumb hypoplasia, and simple syndactyly, was scrupulously described. The authors concentrated on more complex anomalies. We aimed to compare the complexity of surgical interventions and the outcomes between early intervention and delayed intervention cases of complicated hand deformities. The null hypothesis was that the age of patients at the time of surgery would not affect the quality of surgical interventions and outcomes.
2. Materials and Methods
2.1. Study Design and Setting
- To address the research purpose, the investigators designed and implemented a prospective single-center study with a consecutive collection of cases following the STROBE guidelines. The study protocol and written informed consent conformed to the ethical guidelines of the 1975/2013 Helsinki Declaration and were approved by the Institutional Review Board. The study period was set from May 2012 to May 2022 for recruitment, exposure, and data collection. It was terminated in June 2023 when study groups reached the calculated sample size, and all participants had at least a 12-month follow-up period. The patients were referred to the specialized Republican Center for Pediatric Orthopedics by secondary care practitioners who diagnosed complex forms of congenital hand deformities. Some patients were referred for reoperations after previously performed unsuccessful interventions or because of recurrence. Two surgeons experienced in pediatric hand surgery operated on these patients at this tertiary referral hospital with fully functioning surgical units and proper imaging facilities.
2.2. Participants and Study Size
- The study cohort comprised all patients presenting for evaluation and management of isolated and syndrome-affiliated unilateral or bilateral complex forms of congenital hand deformities. The patients who were admitted and operated on at the age younger than five years comprised Group 1. The 5 to 18-year-old patients were assigned to Group 2. A standard sample size 75 calculation for a single-center study determined that a minimum of 60 subjects per group with a total of 120 subjects were required for the difference between Group 1 and Group 2 values to be statistically significant when α = 0.05, the power of the study set at 80% (null hypothesis as equivalence design, α=0.05; β=0.20). The study was terminated when Group 2 reached 60 cases with a proper follow-up period. Inclusion criterion: patients should have isolated or syndrome-affiliated unilateral or bilateral hand deformities that involve three or more fingers. Single-finger clinodactyly, camptodactyly, thumb hypoplasia, six-digit polydactyly, and simple syndactyly cases were excluded. We also excluded cases with the above hand-and-wrist deformities such as phocomelia.
2.3. Presurgical Evaluation
- Proper selection of patients for surgical intervention was the second step after the inclusion/exclusion criteria were met. We considered contraindications for surgical intervention that might include poor health conditions because of a congenital syndrome, within-hand arteriovenous or nerve malformations that might require a multicenter approach, and risk for postsurgical complications and/or recurrence. Patients with multiple syndrome-related malformations were evaluated by a multidisciplinary team. We documented active and passive range of motion of upper extremity joints, bimanual reach towards an object, the palmar grasp, grip strength, pinch strength, abilities and disabilities in manipulating an object with the fingers and with the palm of the hand according to the “Hand Function in Children with Congenital Disorders” guidelines of 2014. A pincer grasp with the tip of the thumb and index finger was checked if the deformity permits. We also used the Manual Ability Classification System (MACS; from 1 – good to 5 – totally inadequate). ABILHANDS-Kids function scale was not used because some items (e.g., “sharpening pencil”) were inapplicable for young patients. A surface EMG investigation was used to assess the functions of the nerves and extrinsic and intrinsic muscle groups and to rule out or detect compression neuropathies. The Wrinkle test was used to check the nerve integrity of the hand by assessing the nervous response to an environmental stimulus in young children who cannot follow instructions. To investigate vascularization, the possible hand skin temperature asymmetry was checked by infrared thermometry and assessed against the healthy hand or against the normative database for bilateral deformities. Arteriography was used for cases with suspected blood circulation abnormalities to rule out postsurgical risk of jeopardizing distal circulation. X-ray investigation was used to understand positions, aphalangia, and deformities of the hand bones, assess a patient’s bone age against his/her chronological age, and detect cases with advanced and delayed skeletal development with the help of the hand-and-wrist radiographic atlas for digital bone age estimation. An evaluation of the amount of available skin helped to choose between graft and graftless surgical techniques.
2.4. Surgical Techniques
- We followed well-established techniques for hand, pediatric plastic, and congenital hand defects surgery. They included general anesthesia, a pneumatic tourniquet, drawing of palmar incision pattern, Cronin zigzag incisions, Buck-Gramcko techniques for the thumb and combined finger malformations, skin and subcutaneous tissue flap lobes, and postsurgical analgesics. For multiple-digit malformations, the thumb was released first, followed by the border fingers. A distal revascularization was used to replace the possible arterial deficit if a case so required. In cases when the digital nerve bifurcated distal to the newly constructed web space, microdissection was used to separate it. We used both graft and graftless surgical techniques. A full-thickness skin graft was harvested from various sites according to the age and condition of a patient. We used autodermal grafts harvested from the thigh, the lateral third of the inguinal crease of the groin area, and the inner shoulder area. In uncircumcised boys, we used foreskin to create proper web spaces. In acrosyndactyly, the index finger was released first. After that, the release of the fifth finger was achieved, which was followed by the release of the central two fingers. We used over compensating the webspace approach to prevent possible web creep. We used one-stage or two stage surgical corrections individualizing the management of the deformities.
2.5. Follow-up and Outcome Evaluation
- We evaluated patients during the dressing change twice a week during the first three to four postsurgical weeks. X-ray, EMG, and infrared thermometry studies were carried out on the third postsurgical day to detect the bone positions and possible nerve and blood supply inadequacies. They were repeated during the six and 12-months follow-ups to assess the recovery process. The subsequent follow-ups were scheduled three, six, and 12 postsurgical months and further in six month periods, checking functional outcomes, physiotherapy and training results, and possible recurrence. For older patients, we examined the grip and in-hand manipulation skills such as writing and drawing or buttoning and tying shoes for two-hand activities. Scaring was evaluated using the modified Vancouver scar scale with 0 (good) to 13 (inadequate) score scale evaluation criteria for scar pigmentation, vascularity, pliability, and height. Web creep was assessed using a 5-point scale system from 0 for normal web space to 4 for total web creep to the proximal interphalangeal joint. We estimated scores 0 to 1 as effective treatment, 2 to 3 as partially inadequate treatment, and 4 as no benefit achieved and reoperation required.
2.6. Bias
- To avoid selection bias, both study groups consisted of consecutive cases. While we had fewer late-release cases than early-release cases, the data collection period ended when Group 2 reached the desirable sample size. Therefore, Groups 1 and 2 had an unequal number of cases, but both reached the calculated sample size. To avoid report bias, all cases, starting from 2012, were reported in the charts and a study database form in a similar way indicating all variables to be used for further analysis.
2.7. Analysis
- The groups of patients were formed according to their age, which served as a primary predictor variable. A Chi-Square test was used to analyze demographic data and time-related variables. We used one-way ANOVA to compare the differences between the groups in the follow-up outcomes and the postsurgical complication rate (Fisher’s exact test) (SPSS ver. 19.0). Statistical significance was considered at the p≤0.05 level.
3. Results
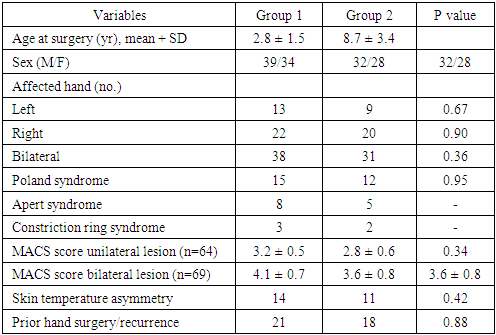
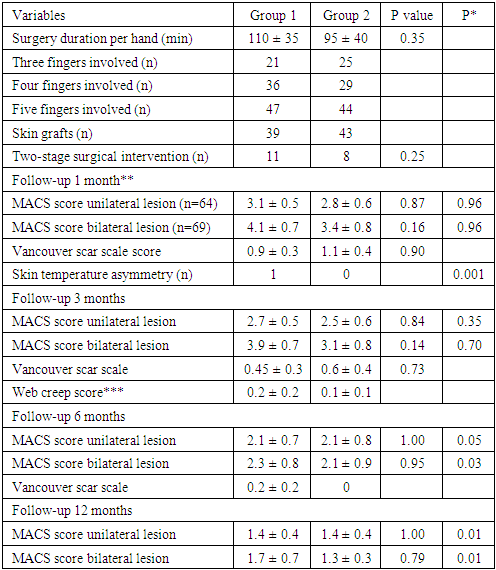
- A total of 536 potentially eligible patients were examined for eligibility; 133 patients (Group 1: n=73, M 39, F 34, mean age 2.8 ± 1.5 years; Group 2: n=60, M 32, F 28, mean age 8.5 ± 3.2 years) were confirmed eligible and included in the study, were operated, completed follow-up, and were analyzed (Table 1). The remaining 403 patients were excluded following the exclusion criteria, surgery contraindication, or lost in follow-up. Most of the patients had complicated syndactyly, symbrachydactyly, and syndrome-related deformities.
|
|
4. Discussion
- We compared the complexity of surgical interventions and the outcomes between early intervention and delayed intervention cases of various isolated or syndrome-affiliated unilateral or bilateral complicated congenital hand deformities. Besides a speedy nerve recovery in young children and graft rejection cases in the group of older patients, all other variables did not show statistically significant differences. Therefore, our null hypothesis that the age of patients at the time of surgery does not affect the quality of surgical interventions and outcomes is mainly confirmed. Complicated hand deformities have a functional, cosmetic, and psychosocial impact. A constant improvement in surgical approaches, including microsurgical techniques, within this area of pediatric surgery has been traced during the last 20 years. It made the question of the timing of surgery less acute. Surgeons operate on children with hand deformities of any age with comparable results. The question of why some parents do not apply for surgical treatment of their children at an early stage remains. In some our cases, physicians evaluated an infant’s condition as “untreatable” and reevaluated as “treatable” in ten or more years. Some parents self-evaluated the child’s condition as untreatable until convinced otherwise. Some delayed cases were operated on when the general health conditions of patients improved. We noted a fear of complicated surgical intervention, religious sentiments, and financial considerations. Our observations support results of Corder et al., who mentioned parents’ fear of surgical correction and congenital cardiac anomalies as factors which delayed surgical interventions.It is beyond the aim of this research, but we would like to share some other observations. While we performed a presurgical assessment of vascularization in the affected hand and used arteriography in some cases, we confirm Wong et al. observation that presurgical assumptions and trans-surgical findings in hand vascularization do not always correlate. We support Solia’s et al. conclusion that the nerve supply of the hand is characterized by numerous variations. Web creep remains a challenging postsurgical complication. We found that the foreskin is perhaps the best graft for proper web formation for uncircumcised boys. The bone age estimation as delayed, normal, or advanced against the chronological age was helpful for surgery planning, decision-making, and assessing functional outcomes. The hand-wrist film method was helpful to estimate skeletal maturity. The nature of interventions necessary to correct certain specific hand deformities remains debatable. Customized methods remain the surgical choice because all variations of hand differences are possible.
5. Conclusions
- The timing of surgical treatment of congenital hand deformities is not paramount. Good functional outcomes can be achieved in children of any age, assuming that the surgical intervention will be followed by proper rehabilitation, physiotherapy, and training activities.
References
| [1] | Goldfarb CA, Ezaki M, Wall LB, et al. The Oberg-Manske-Tonkin (OMT) Classification of Congenital Upper Extremities: Update for 2020. J Hand Surg Am. 2020; 45(6): 542-547. doi: 10.1016/j.jhsa.2020.01.002. |
| [2] | Wall LB, McCombe D, Goldfarb CA, et al. The Oberg, Manske, and Tonkin Classification of Congenital Upper Limb Anomalies: A Consensus Decision-Making Study for Difficult or Unclassifiable Cases. J Hand Surg Am. 2022: S0363-5023(22)00423-3. doi: 10.1016/j.jhsa.2022.07.007. |
| [3] | Chan CCH, McGee P, Hooper G, Lam WL. Re-examining the nomenclature of congenital failure of formation in the upper limb: a historical perspective. J Hand Surg Eur Vol. 2023 Mar 16:17531934231160400. doi: 10.1177/17531934231160400. |
| [4] | Shah A, Bohn DC, Van Heest AE, Hu CH. Congenital Upper-Limb Differences: A 6-Year Literature Review. J Bone Joint Surg Am. 2023; 105(19): 1537-1549. doi: 10.2106/JBJS.22.01323. |
| [5] | Pino PA, Zlotolow DA, Kozin SH. What ̒s New in Congenital Hand Surgery. J Pediatr Orthop. 2020; 40(8): e753-e760. doi: 10.1097/BPO.0000000000001629. |
| [6] | Solia E, Panagouli E, Angelis S, et al. Variations of Ulnar Nerve in the Forearm and Hand: A Review of the Literature and Clinical Significance. J Long Term Eff Med Implants. 2022; 32(1): 45-59. doi: 10.1615/JLongTermEffMedImplants.2021039908. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML