-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2250-2252
doi:10.5923/j.ajmms.20251507.34
Received: May 26, 2025; Accepted: Jun. 19, 2025; Published: Jul. 11, 2025

Changes in the Hemostasis System During the Recovery Period of Children from COVID-19
Turdikul A. Bobomuratov1, Mokhira A. Bakirova2
1Professor, Head of the Department, Tashkent Medical Academy, Tashkent, Uzbekistan
2Department of Propaedeutics of Children’s Diseases, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Turdikul A. Bobomuratov, Professor, Head of the Department, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

COVID-19 is an acute respiratory viral infection in children, accompanied by damage to the it can cause various forms of pneumonia, respiratory failure of varying degrees, septicemia and septic shock. In severe forms of the disease, inflammation of the blood vessels and changes in the hemostasis system can endanger the child's life or lead to a deterioration in the quality of life, disability.
Keywords: COVID-19, Children, Hemostasis, Hypercoagulation, Disability
Cite this paper: Turdikul A. Bobomuratov, Mokhira A. Bakirova, Changes in the Hemostasis System During the Recovery Period of Children from COVID-19, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2250-2252. doi: 10.5923/j.ajmms.20251507.34.
Article Outline
1. Introduction
- Viral diseases account for 80% of infectious diseases, according to the World Health Organization (WHO). The appearance of new infectious diseases in the last 10 years and the development of severe autoimmune pathologies, an increase in the number of allergic patients, are leading to a change in the structure of diseases in childhood. Although the new coronavirus infection, which was registered in 2019, was milder in children than in adults, we observe a significant increase in the incidence among children in the following years, the length of the recovery period after an acute course of the disease and the negative impact on children's lives and quality of life with complications observed in various organs and systems [1]. The clinic of the disease manifests itself after 2-4 days after the infection of the virus. The disease is acute, begins with an increase in body malaise, signs of general poisoning, which are not clearly developed. Also, when breathing in children, chest pain, cough, dry whistling wheezes are heard. Coronavirus infection can be complicated by acute pneumonia. Radiographs of the chest reveal foci or interstitial infiltrates. In severe cases, the activity of the respiratory organs worsens, in the second week the disease develops respiratory symptoms, in adults there is a violation of the function of various organs. In severe forms of the disease, injuries to the lower parts of the respiratory tract are observed, symptoms of pneumonia, sepsis, septic shock appear and can cause the patient's death [3,8].According to the recommendation of the staff of the British pediatric service, the сauses of complications of coronavirus in children:- background diseases, i.e. anemia, endocrine diseases, chronic diseases, including various developmental defects, bronchopulmonary dysplasia);- cases of immunodeficiency caused by various causes;- coinfection with respiratory syncytial virus, influenza virus and other pathogens.Complications of COVID-19 are more common in people with chronic non-infectious disease. The risk group includes people with bronchial asthma, diseases of the endocrine system, i.e. diabetes mellitus, nutritional disorders, as well as those taking a number of drugs: antibiotics, cytostatics, glucocorticoids [9]. Severe inflammation develops in the severe course of COVID-19 and disorders in the management of the immune system arise. The in a general blood test, the formed elements of the blood, such as monocytes and lymphocytes, are reduced. Тhe ratio of types of T-lymphocytes is disrupted.In some patients with a rapid course of the disease, a "cytokine storm" develops due to increased production of interleukins. That is, the body will not be able to regulate the inflammatory process. The body's immune cells are produced in large quantities and affect internal organs [6]. After exposure to coronavirus, tissues attract protective blood cells such as monocytes, lymphocytes, and neutrophils. In this process, Th1 and Th17 produce inflammatory and proinflammatory cytokines, as well as chemokines [8]. Thus vicious circle appears and, in addition to causing "cytokine storm", enhances its development, as well as a severe inflammatory process. This condition leads to multiple organ dysfunction syndrome and severe consequences [9,10]. А postmortem examination revealed a large number of CCR6+, Th17, and increased activity of cytotoxic T-lymphocytes (CD)+ and NK-lymphocytes (CD16)+ in the affected organs [11]. Аn increase in the number of cytotoxic cells does not indicate their normal functioning. The developing lymphopenia is associated with fatigue of cytotoxic lymphocytes under the influence of coronavirus. Macrophages in the se can be damaged by SARS-CoV-2 and, in turn, lead to the development of lymphopenia.Simultaneously, mononuclear cells in peripheral blood stimulate the production of IL6/Il8, attract neutrophils to tissues, and induce an uncontrollable inflammatory response of the body [9]. According to the data presented in the literature, COVID-19 infection in children is more damaging to the nasal cavity, larynx in comparison with lung tissue.Тhe initial period of coronavirus is from two to fourteen days, on average, 5-7 days, and even during this period, patients transmit the disease to those around them, even after the complete disappearance of clinical signs of the disease, for 7-17 days the patient is dangerous for those around him, that is, the disease is contagious [12].The purpose of the examination: to prevent complications observed after COVID-19 and disability among children.
2. Examination Material and Methods
- For the examination, 82 children were selected who had COVID-19 in severe form, were treated in Tashkent City, children's infectious Diseases Hospital No. 3.3 months after leaving the hospital from children, clinical symptoms were collected on a survey basis and a clinical examination (skin color, skin dressing condition, muscle tone and trophic, active and passive movements in the joints, breathing and pulse number, arterial blood pressure) was carried out, as well as their lobarator indicators (general blood analysis, blood biochemical analysis, coagulogram) were examined.
3. Personal Examination
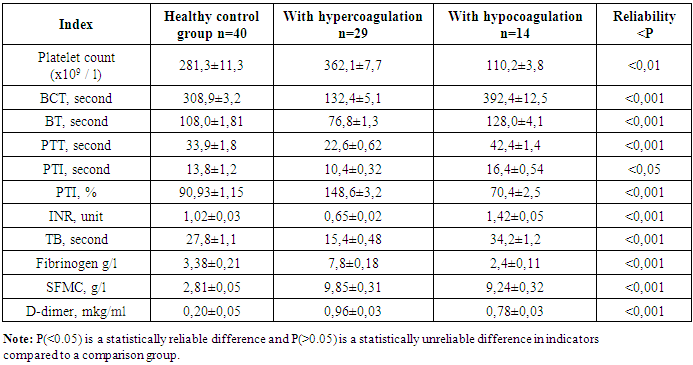
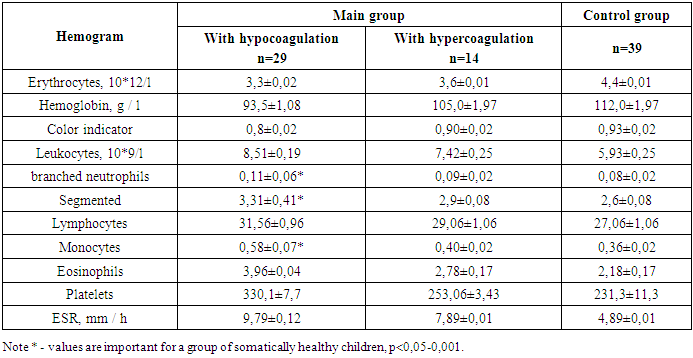
- A comparative analysis of the indicators of the blood clotting system in controlled children during the recovery period made it possible to identify a number of changes in relation to healthy children, which in turn manifest themselves in the form of hypercoagulation and hypocoagulation. We isolated patients undergoing hypercoagulation and hypocoagulation changes in the hemostasis system.
|
|
4. Conclusions
- In children's practice, a special place is occupied by a violation of the hemostasis system, which occurs as a result of a violation of the balance of the body's internal environment as a result of the influence of various exogenous and endogenous factors.Impaired hemostasis balance in the body of morphofunctionally immature children has a negative effect on their overall health. Deep changes observed in the hemostasis system of oganism cause clinical manifestations of hemorrhagic syndrome.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML