-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2223-2227
doi:10.5923/j.ajmms.20251507.28
Received: Jun. 11, 2025; Accepted: Jul. 9, 2025; Published: Jul. 11, 2025

The Impact of Diabetes Duration on Cardiac and Vascular Remodeling
Saidakbarova F. T.1, Srojidinova N. Z.2
1Postdoctoral Student, Republican Specialized Scientific and Practical Medical Center of Cardiology Tashkent, Uzbekistan
2MD, Republican Specialized Scientific and Practical Medical Center of Cardiology Tashkent, Uzbekistan
Correspondence to: Saidakbarova F. T., Postdoctoral Student, Republican Specialized Scientific and Practical Medical Center of Cardiology Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

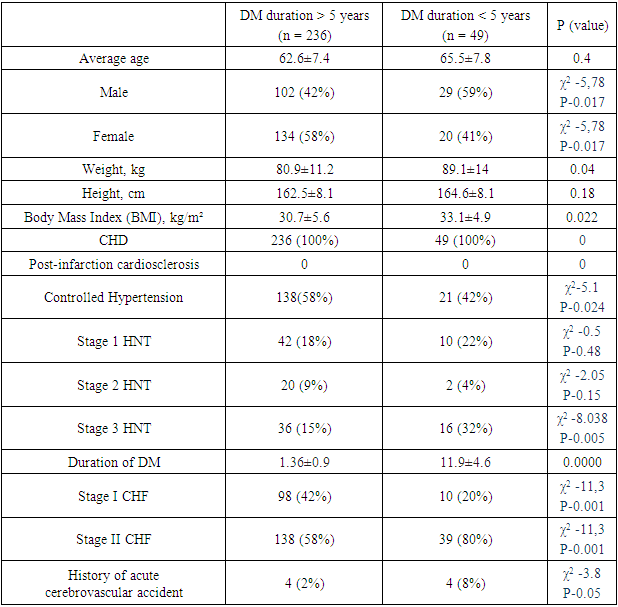
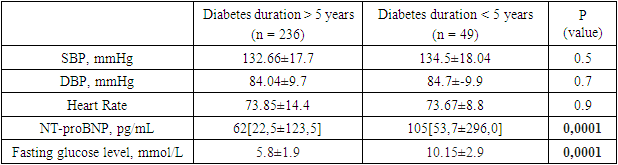
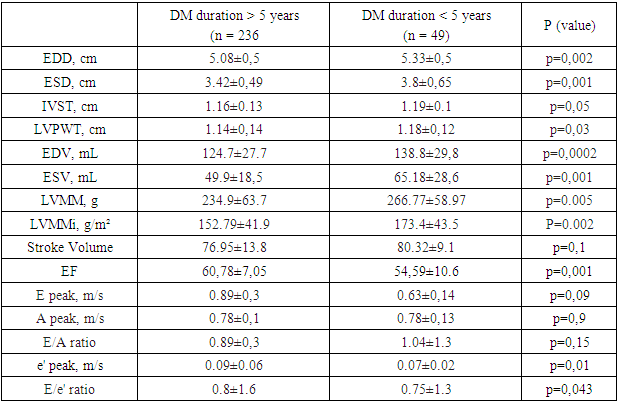
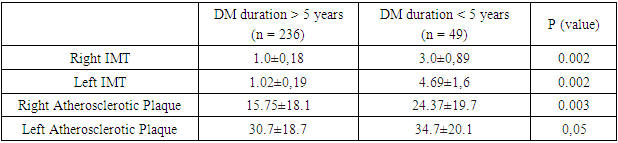
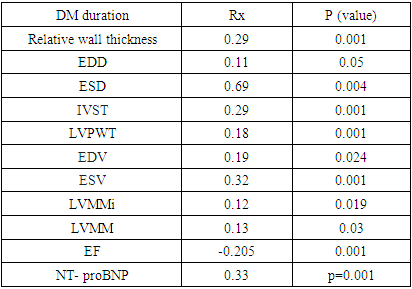
To evaluate the effect of disease duration on cardiac and vascular remodeling in patients with atherosclerotic cardiovascular disease (ASCVD) and type 2 DM. This study included 285 patients aged 35–80 years with HNT and DM who were treated in an inpatient setting. The average age of the patients was 64.11±1.2 years, with 34% male and 66% female. Patients with preserved ejection fraction (LVEF ≥ 50%) were included in this study. Patients were divided into two groups according to the duration of type 2 DM: Group 1 included patients with DM duration of up to 5 years (n=236), and Group 2 included patients with DM duration of more than 5 years (n=49). Statistical analysis was performed using IBM-SPSS 27.0 software package. When comparing the central hemodynamic parameters, it was observed that these measures were larger in Group 2. ESD – 3.42±0.49 cm vs 3.8±0.65 cm, p=0.001; EDD – 5.08±0.5 cm vs 5.33±0.5 cm, p=0.002. EDV – 124.7±27.7 mL vs 138.8±29.8 mL, p=0.0002; ESV – 49.9±18.5 mL vs 65.18±28.6 mL, p=0.001; IVST – 1.16±0.13 cm vs 1.19±0.1 cm, p=0.05; LVPWT – 1.14±0.14 cm vs 1.18±0.12 mm, p=0.03; EF- 60.78±7.05% vs 54.59±10.6%, p=0.001. LVMM (234.9±63.7 g/m2 vs 266.77±58.97 g/m2, p=0.005) and LVMMi (152.79±41.9 g/m2 vs 173.4±43.5 g/m2, p=0.002) were significantly higher in Group 2 than in Group 1. Left ventricular hypertrophy was more common in Group 2 patients (67% vs. 89%, χ2 =4.7, p=0.05).When evaluating peak velocity indicators in both groups, it was found to be non-significantly lower in Group 2: E wave, 0.68±0.15 vs. 0.63±0.14 m/s, p=0.09; A wave, 0.78±0.1 vs. 0.78±0.13 m/s, p=0.9; E/A, 0.89±0.3 vs. 1.04±1.3 m/s, p=0.15. e’ – 0.09±0.06 m/s vs 0.07±0.02 m/s, p=0.01. The E/e’ ratio was found to be significantly lower in Group 2 (0.75 ± 1.3 vs. 0.8 ± 1.6 m/s, p = 0.043).When evaluating the brachiocephalic vessels, the right intima-media thickness (IMT) was 1.0±0.18 vs. 3.0±0.89 mm (p = 0.002), the left IMT was 1.02±0.19 vs. 4.69±1.6 mm (p = 0.002), the right atherosclerotic plaque was 15.75±18.1 vs 24.37±19.7 mm, p=0.003; left Atherosclerotic plaque 30.7±18.7 vs 34.7±20.1 mm, p=0.05. DM is a major clinical problem for treating physicians. It is important to conduct early primary examinations and initiate standard treatment in patients with type 2 DM. This is because not diagnosing the disease for years causes rapid development of severe complications. Prolonging the duration of DM leads to remodeling of the heart and blood vessels.
Keywords: Arterial hypertension, Type 2 diabetes mellitus, NT-proBNP, Cardiac remodeling, Left ventricular diastolic function, Left ventricular systolic function
Cite this paper: Saidakbarova F. T., Srojidinova N. Z., The Impact of Diabetes Duration on Cardiac and Vascular Remodeling, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2223-2227. doi: 10.5923/j.ajmms.20251507.28.
1. Introduction
- According to the World Health Organization, Coronary Heart Disease (CHD) and hypertension (HNT) are the leading causes of death, ranking first among the top ten causes. The risk of developing CHD and HNT in individuals with Diabetes Mellitus (DM) is 3-5 times higher than that in non-diabetic patients [1]. The longer the duration of DM, the greater is the risk. DM is considered an international epidemic. Type 2 DM is the most prevalent form of the disease, accounting for approximately 90% of all cases. The prevalence of DM is rapidly increasing in both developing and developed countries. The prevalence of diabetes among the working-age population increased from 4.7% in 1980 to 8.5% in 2014. Currently, its global average prevalence is estimated to be approximately 11.8% (4.7-13.3%) [2]. Globally, deaths from diabetes are more widespread among women than men, which may be due to the higher cardiovascular risk in women. In our country, the incidence of DM in the population aged 20 to 79 years is 7.5-7.6%, and in the population over 60 years of age, it is 0.74% [1]. CHD and HNT are the main causes of heart failure in patients with DM; however, diabetic cardiomyopathy also plays a key role in its development. The longer the duration of DM, the faster the remodeling of the heart develops, along with the development of macro- and microvascular complications [3].Objective: To evaluate the effect of disease duration on cardiac and vascular remodeling in patients with atherosclerotic cardiovascular disease (ASCVD) and type 2 DM.
2. Materials and Methods
- The study was conducted in the Department of “Cardiometabolic Disorders and Endocrinology” of the Republican Specialized Scientific-Practical Medical Center of Cardiology (RSSPMCC). The study included 285 patients aged 35–80 years with HNT and DM who were treated in an inpatient setting. The average age of the patients was 64.11±1.2 years, with 34% male and 66% female. All patients received commonly prescribed antihypertensive and hypoglycemic medications.The analysis of comorbidities was conducted based on the history of cardiovascular and chronic diseases recorded in the patients' medical records. The presence of comorbidities was determined based on the results of examinations conducted in an inpatient setting. Patients with preserved ejection fraction (LVEF ≥ 50%) were included in this study. Patients were divided into two groups according to the duration of type 2 DM: Group 1 included patients with DM duration of up to 5 years (n=236), and Group 2 included patients with DM duration of more than 5 years (n=49).The structural and functional states of the myocardium and remodeling process were assessed using Doppler echocardiography. Examinations were performed using an ultrasound "ACUSON X 700 PV 2.0" apparatus (SIEMENS, Germany). The examination was performed using the transthoracic method in M and B modes according to the recommendations of the American Society of Echocardiography. According to the recommendations, LVEF is measured based on the disc method (Simpson's method) in biplane (apical 4-chamber and apical 2-chamber) view. Left ventricular end-diastolic (LVEDV) and end-systolic volumes (LVESV) were obtained from the 4- and 2-chamber views. The following structural parameters of the heart were assessed in the EchoCG examination: end-diastolic dimension (EDD), end-systolic dimension (ESD), interventricular septal thickness (IVST), left ventricular posterior wall thickness (LVPWT), left atrial index (LAI), aorta, left ventricular myocardial mass (LVMM), LVMM index (LVMMi), and relative wall thickness (RWT). Left ventricular systolic function was determined using the Simpson method: end-diastolic volume (EDV), end-systolic volume (ESV), left ventricular ejection fraction (LVEF), and stroke volume (SV), which is the difference between EDV and ESV. Myocardial diastolic function was assessed using the following indicators: peak early diastolic filling velocity (E wave), peak late diastolic filling velocity (A wave), and E/A ratio. Ultrasonography of the brachiocephalic vessels was performed using an ultrasound apparatus. NT-pro BNP was measured using an electrochemiluminescence immunoassay (ECLIA; Roche).
|
3. Results
- The two groups were compared for ambulatory Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) values. No differences were found when comparing the SBP and DBP values. When comparing NT-proBNP values, a significantly higher value was obtained in Group 2 (62[22.5±123.5] pg/mL vs. 105[53.7±296.0] pg/mL; (p=0.001). When comparing fasting glucose levels in both groups, it was found that the levels were significantly higher in Group 2 (5.8 ± 1.9 mmol/L vs. 10.15 ± 2.9 mmol/L, p = 0.0001).
|
|
|
|
4. Discussion
- Early diagnosis of HF in patients with type 2 DM at early stages of development, that is, during the period when reversible changes in organs may develop, can reduce the development of cardiovascular complications, disability, and risk of death. This is because the duration of DM directly affects the development of complications of DM. Uncontrolled DM can cause complications that are twice as severe. In DM, initial changes in the heart may begin with left ventricular (LV) diastolic dysfunction. Left ventricular diastolic dysfunction is a sign of early heart damage and can be diagnosed long before clinical signs of the disease develop. Left ventricular diastolic dysfunction is the only functional disorder of the heart that can be detected by echocardiography (EchoCG) [4,7]. According to the recommendations of the European Society of Cardiology, the determination of blood brain natriuretic peptide hormone (BNP) and its NT-pro BNP fraction is important in the diagnosis of CHF [5]. In our study, even though patients with preserved left ventricular EF were included, the amount of NT-pro BNP in the blood was significantly high and correlated with the duration of DM.The development of CHF in patients with type 2 DM is rapid [6]. In all patients with DM included in the study, the presence of two stages of CHF was observed. An increase in the duration of diabetes mellitus was associated with the development of severe heart failure. Therefore, timely diagnosis of LV dysfunction is important in this patient category. The main diagnostic methods are echocardiography (EchoCG) and plasma BNP or NT-pro BNP analysis [8]. This study examined the association between type 2 DM duration and NT-pro BNP levels and structural changes in the heart. Despite the fact that the patients included in the study had preserved EF, we can see that NT-pro BNP was higher in patients with diabetes for more than 5 years. As the duration of DM increases, heart remodeling becomes more pronounced. In addition, the degree of atherosclerotic damage to the brachiocephalic vessels was more pronounced in patients with DM for more than 5 years. It was found that the stronger the heart remodeling, the higher the NT-pro BNP value in the patient. In addition, a direct correlation was observed between the duration of DM and NT-pro BNP values and LV dimensions.
5. Conclusions
- DM is a major clinical problem for treating physicians. It is important to conduct early primary examinations and initiate standard treatment in patients with type 2 DM. This is because not diagnosing the disease for years causes rapid development of severe complications. Prolonging the duration of DM leads to remodeling of the heart and blood vessels.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML