-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2216-2218
doi:10.5923/j.ajmms.20251507.26
Received: Jun. 6, 2025; Accepted: Jul. 1, 2025; Published: Jul. 11, 2025

Clinical-Diagnostic Parallels and Prevention of Tubal Pregnancy: Immunological and Morphological Aspects from a Regional Cohort Study in Uzbekistan
Sayora Mukimjanovna Nazarova1, Dilfuzakhon Zakirjanovna Mamarasulova2
1Andijan Branch of Republican Emergency Medical Care Center, Andijan, Uzbekistan
2Doctor of Medical Sciences, Professor, Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Sayora Mukimjanovna Nazarova, Andijan Branch of Republican Emergency Medical Care Center, Andijan, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Tubal pregnancy (TP), a severe form of ectopic pregnancy, remains a pressing issue in reproductive health, contributing significantly to maternal morbidity and infertility. Objective: To enhance the early diagnosis and prevention of TP through analysis of immunological, clinical, and morphological data from women in the Andijan region. A comparative study of 323 women, including 40 with ruptured tubal pregnancy and 40 with normal early pregnancy (≤12 weeks). β-hCG, IL-10, IL-33, VEGF levels were assessed, along with histomorphological analysis of fallopian tubes and risk factor screening. TP was linked to high inflammation markers, prior pelvic inflammatory disease, and abnormal cytokine profiles. VEGF and IL-33 levels were significantly higher in TP cases. A new diagnostic algorithm incorporating biomarkers and imaging improved early detection. Vitamin-mineral complex (Elevit) used in preconception care improved immune regulation. Cytokines such as VEGF, IL-10, and IL-33, combined with imaging and history-taking, form the basis of an effective early detection and prevention strategy for TP.
Keywords: Ectopic pregnancy, Tubal pregnancy, Fallopian tube, IL-33, IL-10, TNF-α, VEGF, Cytokines, Early diagnosis, Prevention, Andijan, Uzbekistan
Cite this paper: Sayora Mukimjanovna Nazarova, Dilfuzakhon Zakirjanovna Mamarasulova, Clinical-Diagnostic Parallels and Prevention of Tubal Pregnancy: Immunological and Morphological Aspects from a Regional Cohort Study in Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2216-2218. doi: 10.5923/j.ajmms.20251507.26.
1. Introduction
- Tubal pregnancy (TP), the most common form of ectopic pregnancy, represents a significant threat to maternal health due to its high risk of rupture and internal bleeding. It accounts for over 90% of all ectopic pregnancies and remains one of the leading causes of pregnancy-related morbidity and mortality in the first trimester [1]. Despite technological progress in imaging and laboratory diagnostics, delayed recognition of TP is still common, especially in low-resource settings [3].The etiology of TP is multifactorial, involving tubal epithelial damage, chronic inflammation, and disrupted embryonic transport [4]. Recent evidence emphasizes the role of immunological dysregulation and inflammatory cytokines in altering the tubal microenvironment, thereby facilitating abnormal implantation [2] [6]. In particular, angiogenic markers such as vascular endothelial growth factor (VEGF) and immune mediators like interleukins IL-10 and IL-33 have been implicated in pathological trophoblast invasion and immune escape mechanisms [7] [8].In Uzbekistan and other parts of Central Asia, access to timely diagnostic and preventive care for TP remains limited, often resulting in late presentation with ruptured ectopic pregnancy and associated complications. Therefore, identifying reliable biomarkers for early diagnosis is essential to reduce preventable maternal harm [2]. Integrating cytokine profiling into clinical workflows offers a promising avenue for enhancing diagnostic precision, especially when combined with imaging and risk assessment.This study aimed to assess the diagnostic value of VEGF, IL-10, and IL-33 in women with TP and to explore the clinical, morphological, and immunological features of ectopic implantation in a regional cohort from Andijan, Uzbekistan.
2. Materials and Methods
- This clinical observational study enrolled 323 women from Andijan region between 2021–2023. Of these, 40 women had confirmed ruptured TP and 40 had healthy intrauterine pregnancies (≤12 weeks). Clinical assessments included ultrasound and MRI imaging. Immunoassays were performed to determine serum levels of VEGF, IL-10, IL-33, and TNF-alpha. Pathological analysis of excised fallopian tubes was also conducted. Statistical analysis used Student’s t-test and ANOVA (p < 0.05).
3. Results and Discussion
- The mean levels of VEGF and IL-33 were significantly higher in the TP group compared to controls (p < 0.01). IL-10 and TNF-alpha were also elevated in TP cases. The diagnostic algorithm integrating biomarker screening with imaging showed higher sensitivity (91%) and specificity (87%) in early TP detection. Morphological analysis revealed severe tubal wall thinning and vascular infiltration in TP cases (Table 1).
|
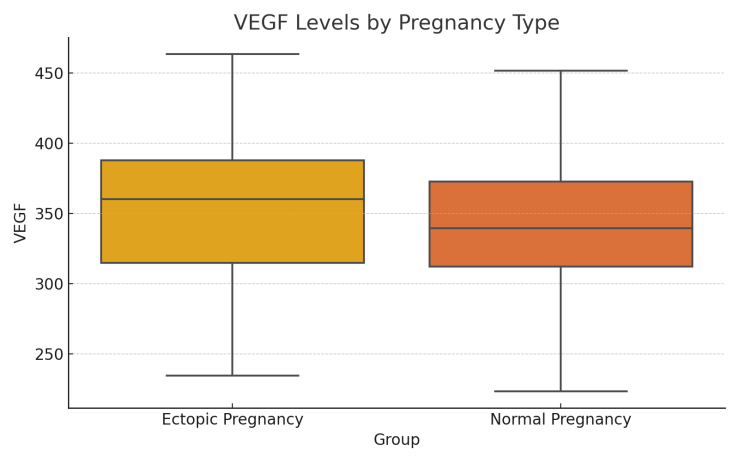 | Figure 1. VEGF levels in ectopic vs normal pregnancy |
 | Figure 2. IL-33 levels in ectopic vs normal pregnancy |
 | Figure 3. IL-10 levels in ectopic vs normal pregnancy |
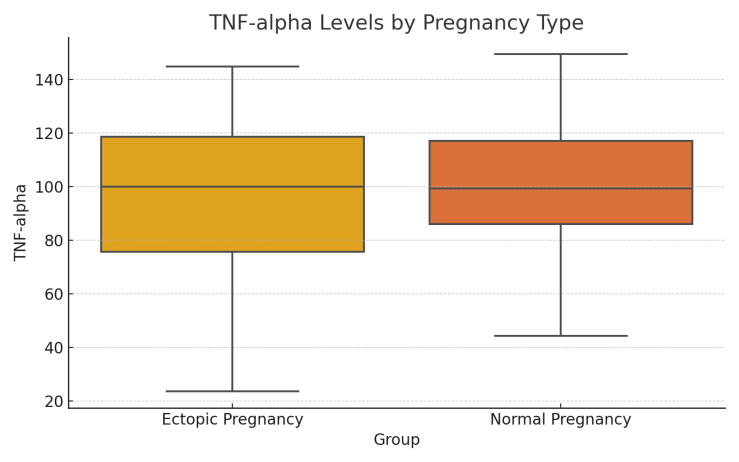 | Figure 4. TNF-alpha levels in ectopic vs normal pregnancy |
4. Conclusions
- The integration of immunological biomarkers, imaging diagnostics, and clinical risk profiling offers a comprehensive approach for early TP diagnosis. Our findings support the role of VEGF, IL-10, and IL-33 as predictive indicators. Future studies should focus on validating these markers in larger multicenter cohorts.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML