-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(7): 2195-2198
doi:10.5923/j.ajmms.20251507.22
Received: Jun. 10, 2025; Accepted: Jul. 6, 2025; Published: Jul. 11, 2025

Assessment of Chronic Kidney Disease in Patients with Prediabetes Identified Through Screening
Yusupova Sh. K.1, Chartakov A. K.2
1Doctor of Medical Sciences, Associate Professor, Head of the Department of Hospital Therapy and Endocrinology, Andijan State Medical Institute, Andijan, Uzbekistan
2Assistant, Department of Hospital Therapy and Endocrinology, Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Chartakov A. K., Assistant, Department of Hospital Therapy and Endocrinology, Andijan State Medical Institute, Andijan, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

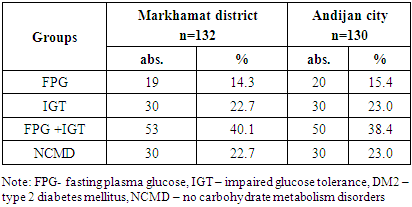
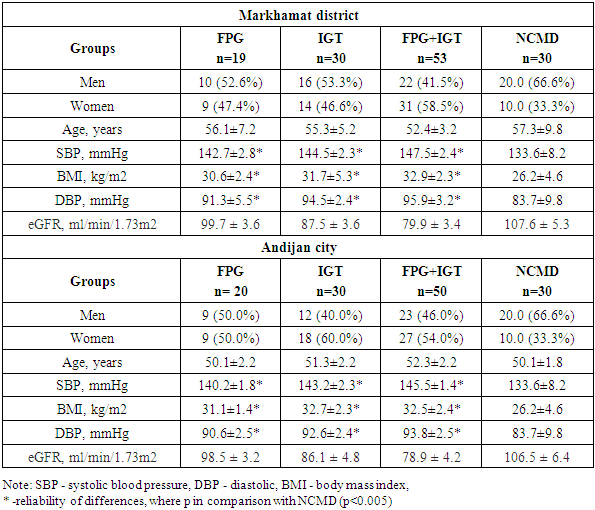
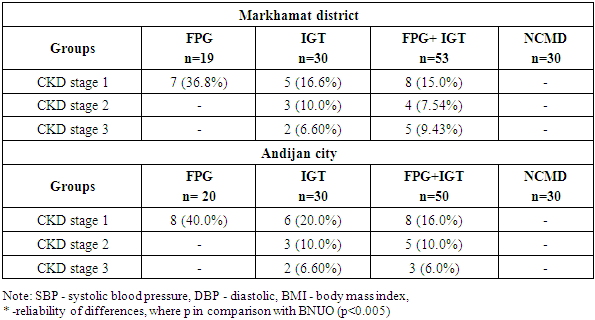
The aim of this study was to investigate the biochemical characteristics of patients with prediabetes and renal dysfunction identified during screening in the city of Andijan and the Markhamat district of the Andijan region. A total of 3,400 individuals from the risk group were examined, with 1,800 residing in the Markhamat district and 1,600 in the city of Andijan. The control group consisted of 20 healthy individuals. A total of 262 patients with prediabetes were identified: 132 from the Markhamat district and 130 from the city of Andijan. General clinical and biochemical methods were employed, including measurement of blood glucose levels, glycated hemoglobin, C-reactive protein, urea, creatinine, lipid profile, cystatin-C, microalbuminuria, and calculation of glomerular filtration rate (eGFR). The results showed that 19 patients in the Markhamat district and 20 patients in the city of Andijan were identified with various forms of prediabetes. In 34.2% of cases, low eGFR and proteinuria were observed among patients with prediabetes. Patients with type 2 diabetes and prediabetes also showed lower eGFR, higher systolic blood pressure, and increased body mass index (BMI) at baseline. The study demonstrated that albuminuria was less pronounced in patients with prediabetes compared to those with type 2 diabetes. These findings highlight the importance of early diagnosis and monitoring of renal function in individuals with prediabetes.
Keywords: Prediabetes, CKD, Assessment, Morbidity and health care, Diabetes mellitus, Chronic kidney disease
Cite this paper: Yusupova Sh. K., Chartakov A. K., Assessment of Chronic Kidney Disease in Patients with Prediabetes Identified Through Screening, American Journal of Medicine and Medical Sciences, Vol. 15 No. 7, 2025, pp. 2195-2198. doi: 10.5923/j.ajmms.20251507.22.
1. Introduction
- Chronic kidney disease (CKD) is becoming increasingly common worldwide, in both developing and developed countries [1] and is associated with a significant burden of mortality, morbidity and health care costs [2]. Diabetes is a growing pandemic [3] and is a major cause of CKD in many countries, contributing to the increase in CKD-related morbidity and mortality [4,5]. For example, in the United States, diabetes accounts for 30 to 40% of CKD [6]. Furthermore, recent data suggest an increased risk of CKD even in non-diabetic glycemic ranges [7,8].Despite our understanding of type 2 diabetes mellitus (T2DM) as an established risk factor for progressive kidney disease and cardiac complications, the prognostic significance of prediabetes in patients with chronic kidney disease (CKD) remains largely unknown, according to the authors [9]. Of the 3701 individuals analyzed, 945 were normoglycemic, 847 had prediabetes, and 1909 had diabetes. The median follow-up was 7.5 years. Prediabetes was not associated with the composite renal outcome (adjusted hazard ratio [aHR], 1.13; 95% confidence interval [CI], 0.96-1.32; P = .14) but was associated with progression of proteinuria (aHR, 1.23; 95% CI, 1.03-1.47; P = .02). The authors concluded thatIn individuals with CKD, prediabetes was not associated with composite renal outcome but was associated with an increased risk of proteinuria progression and adverse cardiovascular outcomes.To study the relationship between diabetes and prediabetes with chronic kidney disease (CKD) taking into account major risk factors such as gender, age, lifestyle, smoking and blood pressure, a study was conducted in Iran in 2024. Between November 17, 2016 and November 22, 2018, 4063 subjects aged 35 to 70 years were enrolled in the first phase of the Bandar-e-Kong Noncommunicable Diseases (BKNCD) cohort study, which is part of the PERSIAN (Prospective Epidemiological Studies in Iran) cohort [10]. According to their data, The prevalence of CKD was 15.3%, with 29.6% in individuals with diabetes and 16.5% in patients with prediabetes. Thus, the prevalence of CKD in patients with type 2 diabetes was higher than in prediabetics and healthy individuals. Older age, dysglycemia (diabetes or prediabetes), hypertension, and the use of angiotensin receptor blockers were significantly associated with an increased risk of CKD in adults.The prevalence of albuminuria, decreased renal function, and CKD increased with increasing glycemia (P < 0.001), noted the authors from China. Based on the MDRD study equation, the unadjusted prevalence of CKD was 30.9%, 28.5%, 14.1%, and 9.2% in individuals with diagnosed diabetes, undiagnosed T2DM, prediabetes, and normoglycemia, respectively [11].All of the above formed the basis for this study.The aim of the study isto assess chronic kidney disease in patients with prediabetes identified through screening.
2. Material and Methods of Research
- A total of 3,400 risk group individuals were examined, of whom 1,800 were residents of the Markhamat district of the Andijan region and 1,600 were residents of Andijan city. A total of 262 patients with prediabetes were identified: 132 in the Markhamat district and 130 in Andijan city. Inclusion criteria: individuals over 20 years of age suffering from overweight, dyslipidemia or hypertension. Exclusion criteria: type 1 diabetes mellitus, other endocrine diseases, metformin intake, severe autoimmune diseases, vasculitis, oncology. Prediabetes (preDM) is a condition defined as an intermediate state in glucose metabolism that is part of a continuum from normoglycemia to diabetes mellitus (DM). Criteria for identifying patients with preDM are based on changes in glucose levels measured by fasting plasma glucose (FPG), glycosylated hemoglobin (HbA1c), or two-hour post-load plasma glucose (2hBG).According to the design, the study was conducted in two stages.At the first stage, patients were surveyed, including using the Findrisk scale.At the 2nd stage, freshly collected biological material (venous blood) was collected and then promptly delivered to the laboratory for research.The research methods included general clinical approaches, biochemical testing (measurement of blood glucose levels on an empty stomach and two hours after a meal, determination of glycated hemoglobin, C-reactive protein levels, urea, creatinine and lipid profile, Cystatin-C, microalbuminuria, calculation of SCF).Statistical research methods. The overall prevalence of CKD, reduced renal function and albuminuria by glycemic status was calculated. Odds ratios (OR) and 95% confidence intervals (CI) of the independent association between dysglycemia (prediabetes or diabetes) and CKD, adjusted for age, sex, hypertension status, BMI and TG, were estimated using logistic regression models.
3. Research Results
- Table 1 shows the distribution of patients from the Markhamat district and the city of Andijan by clinical groups.
|
|
|
4. Conclusions
- 1. Prediabetes is associated with early-stage kidney damage. This study provides evidence that a significant proportion of patients with prediabetes show early signs of chronic kidney disease (CKD), such as microalbuminuria and a mild reduction in glomerular filtration rate (GFR). These findings underscore the importance of early detection of prediabetes and the need for vigilant monitoring of kidney function at early stages.2. Comorbid cardiometabolic factors exacerbate the risk of CKD in prediabetes. Patients with prediabetes who also present with risk factors such as arterial hypertension, obesity, and dyslipidemia demonstrate more significant alterations in kidney function. This highlights the necessity for a comprehensive clinical evaluation that incorporates all potential risk factors in managing patients with prediabetes.3. Prediabetes should be recognized as a risk factor for CKD, not merely as a precursor to type 2 diabetes. Early-stage kidney damage is already evident in some patients with prediabetes, suggesting that this condition should be regarded as an independent risk factor for CKD, not solely as a stage before the development of type 2 diabetes. Early kidney involvement in prediabetes warrants increased clinical awareness.4. The importance of screening for prediabetes and CKD. Our findings emphasize the need for widespread screening to identify prediabetes and early-stage CKD in high-risk populations, including individuals over 40 years of age, those with excess weight, hypertension, and other metabolic abnormalities. Early identification enables timely intervention and the potential for prevention of disease progression.5. Early prevention and continuous monitoring are critical. Identifying prediabetes and kidney function impairment at an early stage provides an opportunity for early intervention. Monitoring of blood pressure, blood glucose levels, and lifestyle modification are crucial in preventing the progression of CKD and diabetic nephropathy.6. Further research is needed. Longitudinal prospective studies are necessary to more precisely assess the long-term effects of prediabetes on CKD progression. These studies should explore the mechanisms underlying kidney damage in prediabetes and identify the most effective interventions for slowing disease progression.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML