Shonazarov Iskandar Shonazarovich, Rakhmonov Firdavs Salomatovich
Samarkand State Medical University, Samarkand, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Gastroduodenal ulcers constitute a significant gastrointestinal disorder, affecting a large segment of the population and often leading to serious complications, including bleeding. This bleeding can result from erosion of blood vessels due to ulcer formation, necessitating prompt medical intervention. Historically, the management of gastroduodenal ulcer bleeding has involved various surgical strategies, ranging from ulcer resection to less invasive techniques such as cauterization. Recent advancements in surgical techniques, coupled with improved understanding of the pathophysiology of ulcers, have contributed to enhanced patient outcomes. These improvements not only aim to control bleeding effectively but also to minimize complications, reduce recovery times, and optimize overall surgical care for patients suffering from this debilitating condition. As we delve into current methodologies and future directions in surgical treatment, it becomes essential to evaluate both established practices and innovative approaches that promise to advance the field further.
Keywords:
Gastroduodenal ulcer, Bleeding, Surgical treatment, Ulcer resection, Cauterization, Minimally invasive surgery, Patient outcomes
Cite this paper: Shonazarov Iskandar Shonazarovich, Rakhmonov Firdavs Salomatovich, Improvement of Surgical Treatment of Gastroduodenal Ulcer Bleeding, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 2019-2024. doi: 10.5923/j.ajmms.20251506.87.
1. Introduction
Gastroduodenal bleeding is one of the complex clinical problems in abdominal surgery, associated with high mortality rates and requiring urgent hospitalization. Among the sources of gastroduodenal bleeding, stomach and duodenal ulcers account for 71.2%. In 75-80% of patients, bleeding stops on its own, while in 20-25% of cases, bleeding is active during the initial endoscopic examination. Over the past 50 years, the overall mortality rate has remained at around 10% [1,6].One of the complex issues in emergency surgery remains the choice of treatment tactics for patients with gastroduodenal ulcer bleeding. Despite the progress of medical science and clinical practice, and the more than century-long history of discussions on this issue, the problem of treatment tactics for patients with gastroduodenal ulcer bleeding remains one of the most pressing problems in modern emergency surgery [2,7].The current stage of surgical treatment for peptic ulcer disease should be considered a time when organ-preserving operations with vagotomy have paramount importance in the treatment of gastroduodenal ulcers [3,8]. Many surgeons are moving away from radical interventions, establishing a trend towards organ-preserving procedures. New technologies allow for the application of minimally traumatic variants of these operations. The methodology and technique of organ-preserving operations continue to be improved [4,9].Thus, the widespread introduction of modern endoscopic techniques into clinical practice, which allow for the cessation of bleeding, as well as the use of minimally invasive surgeries, has led to changes in the treatment tactics for patients with bleeding gastroduodenal ulcers and a differentiated determination of indications for surgical intervention [5,10].Research objective. To develop a method for stopping ulcerative gastroduodenal bleeding using hybrid technologies by laparoscopic suturing of bleeding ulcers with endoscopic navigation.
2. Materials and Research Methods
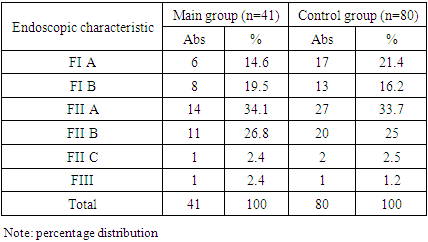
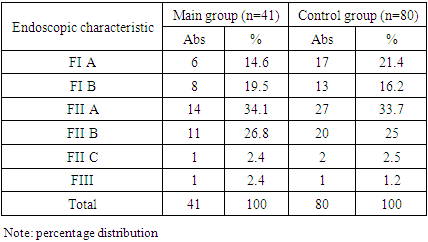
This work is based on the experience of the clinic covering a 5-year period (2020-2024) at the Department of Surgical Diseases and Endoscopy of the Faculty of Postgraduate Education at Samara State Medical University, based in the Samarkand branch of the Republican Scientific Center for Emergency Medical Care. The study included 121 patients with gastroduodenal ulcer bleeding.The studied group of patients was divided into two groups: - the comparison group consisted of 80 patients; - the main group consisted of 41 patients, differing in approaches to the management and treatment of patients with gastroduodenal ulcer bleeding. In the overall group, the age of patients ranged from 19 to 79 years, with 10 patients (8.3%) being older than 60 years. There were 89 (73.5%) men and 32 (26.5%) women. In the overall group, all variants of peptic ulcer were observed: duodenal ulcer disease (DUD), gastric ulcer disease (GUD) of types 1, 2, and 3 according to Johnson's classification. Among the sources of bleeding, duodenal bulb ulcers predominated in 65 (53.6%) patients.The size of ulcers was determined by their area, calculated based on visual data. In 71 (58.6%) patients, the size of ulcers ranged from 5 mm to 10 mm, 21 (17.4%) patients had ulcers from 10-15 mm, and 9 (7.4%) patients had ulcers larger than 15 mm.In 36 (29.6%) patients, concomitant pathology was identified. It should be emphasized that in some cases, the same patient had more than one comorbidity.In 121 patients with gastroduodenal bleeding, all patients reported melena during history taking, with the presence of "coffee ground" vomitus in 79 (65.3%) patients. Vomiting with blood clots was observed in 42 (34.7%) patients. All patients with gastroduodenal ulcer bleeding underwent urgent fibroesophagogastroduodenoscopy (FEGDS). According to endoscopy data, the source of bleeding was identified in 118 (97.5%) cases.The majority of patients were hospitalized with grade II blood loss, accounting for 73 (63%) cases. Grade I blood loss was observed in 21 (17.4%) patients, while grade III blood loss was seen in 25 (20.6%) patients. Only 2 (1.6%) patients experienced grade IV blood loss.During endoscopy, we assessed bleeding activity according to the J.A. Forrest (1974) classification.According to endoscopy data, the source of bleeding was identified in 97.5% of cases. The severity of bleeding was evaluated based on the endoscopic image using the J. A. Forrest (1974) classification.Table 1. Distribution of patients with gastroduodenal ulcer bleeding according to J. Forrest classification
 |
| |
|
As shown in Table 1, in the main group, 14 patients (34.1%) had type I (FI) active bleeding; 26 patients (63.4%) had type II (FII) recent bleeding, and 1 patient (2.4%) had type III (FIII) bleeding. In the control group, type I (FI) was observed in 30 patients (37.5%), type II (FII) in 49 patients (61.2%), and type III (FIII) in 1 patient (1.2%) (p=0.002).When studying the frequency of bleeding by ulcer location in the main group, bleeding occurred in: the body of the stomach - 5 cases (12.2%), the cardiac region of the stomach - 2 cases (4.9%), the pyloric-antral region of the stomach - 9 cases (21.9%), and the duodenum - 25 cases (60.9%).In the control group, bleeding occurred in 8 (10%) cases in the body of the stomach, in 4 (5%) cases in the cardiac part of the stomach, in 28 (35%) cases in the pyloric-antral part of the stomach, and in 40 (50%) cases in the bulb of the duodenum.When studying the frequency of bleeding by ulcer size, as can be seen from the table, in the main group ulcers with a diameter of up to 5 mm were observed in 10 (24.4%) cases, from 5 to 10 mm in 23 (56.1%) cases, from 10 to 15 mm in 6 (14.6%) cases, and more than 15 mm in 2 (4.9%) cases. In the control group, ulcers with a diameter of up to 5 mm were observed in 10 (12.5%) cases, from 5 to 10 mm in 48 (60%) cases, from 10 to 15 mm in 15 (18.7%) cases, and more than 15 mm in 7 (8.7%) cases.We studied the recurrence of bleeding based on the size of the ulcerative defect during a retrospective study in the control group. Recurrence of bleeding with an ulcer size of up to 5 mm was observed in 1 (1.3%) patient, from 5 to 10 mm in 13 (16.3%) cases, from 10 to 15 mm in 9 (11.3%) patients, and more than 15 mm in 3 (3.8%) cases.
3. Results and Discussion
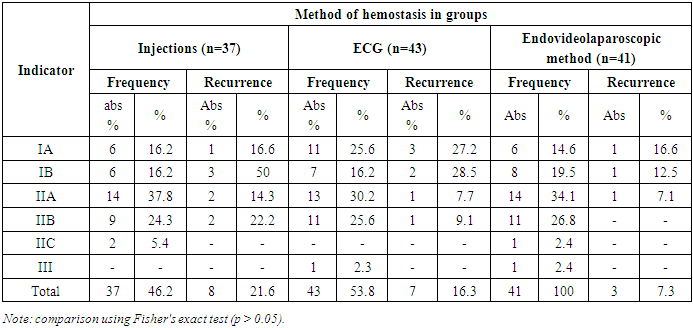
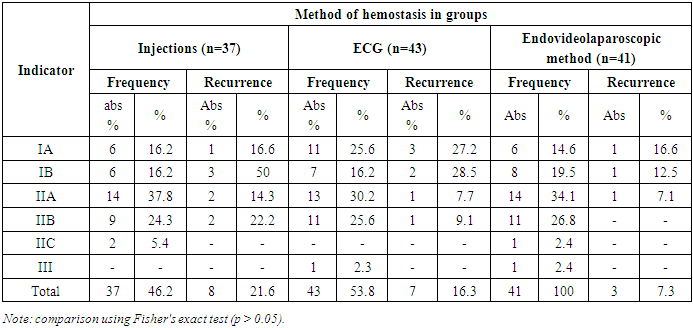
Treatment tactics for patients in the control group were determined after confirming ongoing bleeding during FGDS, and in 80 cases, various options for endohemostasis were used. In 37 patients, vasoconstricting (adrenaline solution in 1:10000 dilution) and denaturing agents (70% ethyl alcohol) were injected into and around the ulcer tissue. In 43 cases, electrocoagulation of bleeding vessels in the ulcer niche and/or tissues along the perimeter of the defect was used. For therapeutic measures in the main group, the developed hybrid endovideolaparoscopic method of endohemostasis was applied.During the operation, while inserting trocars after preliminary gastric lavage, instead of a gastric tube, the endoscopist inserted an endoscope into the stomach or duodenum to visualize the source of bleeding (Figure 1). The surgeon and endoscopist worked in combination (Fig. 2).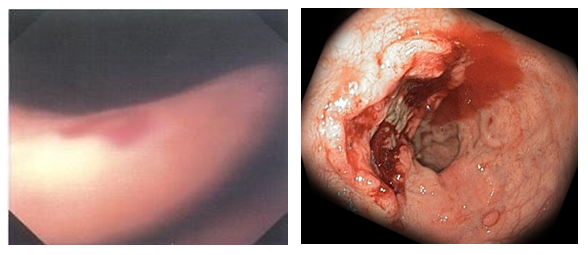 | Figure 1. Standard laparoscopic view during diaphanoscopy (a) and gastroscopic view (b) of a gastric ulcer complicated by bleeding |
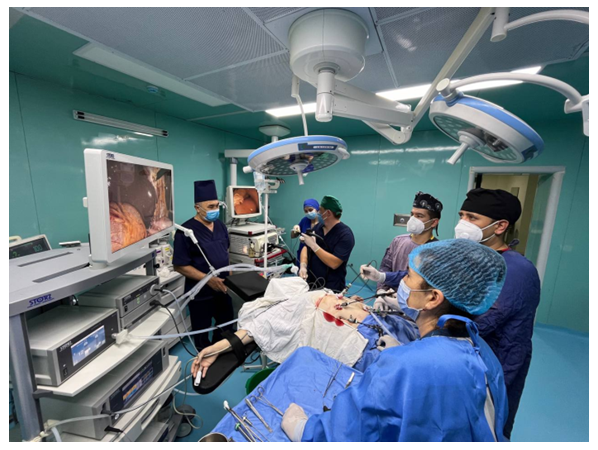 | Figure 2. Positioning of the surgical and endoscopic team |
We have developed a methodology at our clinic for determining the source of bleeding during combined hybrid endolaparoscopic interventions.In this method, the bleeding point is visualized using the illumination from the endoscope light (diaphanoscopy). The simultaneous work of the surgeon and endoscopist ensures visualization of the bleeding source throughout the entire surgical intervention.The developed methodology allowed the surgeon to accurately locate the bleeding source without opening the hollow organ. After identifying the source of bleeding, transserosal suturing of the bleeding vessel was performed, or it was ligated using clips.In 25 (60.9%) patients of the main group, the bleeding ulcer was located in the anterior or anterolateral bulbar part of the duodenum. Transserosa suturing of the branches was performed on: a. gastrica dextra, a. gastroduodenalis, a. gastroomentalis dextra. In 6 cases, the artery trunk itself was ligated, and in 2 cases, due to uncertainty about stopping the bleeding because of adhesions, laparoscopic excision of the bleeding ulcer was performed.In 5 (12.2%) patients, the ulcers were localized in the body of the stomach: transserosa suturing of branches was performed on: a. gastrica dextra, a. gastrica sinistra, a. gastroomentalis dextra, a. gastroomentalis sinistra, a. gastricae breves, a. lienalis. In 9 (21.9%) patients, the ulcers were located in the pyloroantral zone. Transserosa suturing of the branches was performed on: a. gastrica dextra, a. gastroomentalis dextra. In 2 (4.9%) patients, the ulcers were localized in the cardiac region of the stomach. Transserosa suturing of branches was performed on: a. gastrica sinistra, a. gastricae breves, r. esophagus.We studied the frequency of bleeding recurrence, the frequency of forced operations, and mortality, which is the most significant indicator affecting treatment outcomes.Statistical analysis of the results from both groups revealed a significant difference in the degree of relapse development (p = 0.012421, Pearson's method). In the control group, two variants of endoscopic bleeding control were used, and the number of relapses after hemostasis was statistically higher in FIA and FIB compared to the FIIA and FIIB group (p = 0.0103, Fisher's exact test). The frequency of recurrence in active bleeding FIA was 4 out of 17 patients (23.5%), in the FIB group - 5 out of 13 patients (38.4%), and using Fisher's exact test, no statistically significant difference was found (p<0.05).Regarding the number of relapses, when comparing the injection method with ECG, a statistically significantly higher number of relapses was observed with the use of the injection method and electrocoagulation (p = 0.0112, Fisher's exact test) compared to the use of the hybrid endovideolaparoscopic method, favoring the latter.The frequency of recurrence in cases of bleeding that had already occurred (FII) after applying the injection method was 4 out of 23 patients (17.4%), while for coagulation endohemostasis it was 2 out of 24 patients (8.35%) (p > 0.05) (Table 2).Table 2. Frequency of recurrence of ulcerative gastroduodenal bleeding depending on the hemostasis method and intensity of bleeding (according to J. Forrest)
 |
| |
|
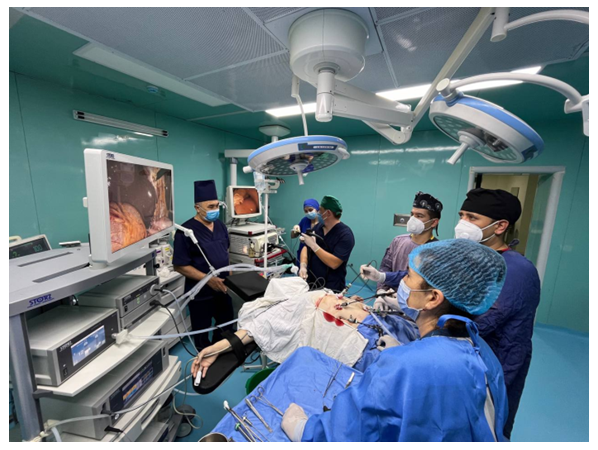
When comparing the variants of the endoscopic method with the combined hybrid endovideolaporoscopic method of stopping bleeding in the FIA and FIB groups, a statistically significant difference (p < 0.05) was revealed in favor of the latter (p = 0.0138, Fisher's exact test).After the above analysis, it can be concluded that the use of a combined endolaparoscopic method for stopping ongoing and arrested bleeding is more effective and statistically significant compared to the two options of endoscopic hemostasis (p < 0.05).When analyzing the results in the main group for Forrest Ia - Ib, 2 patients (4.8%) required forced surgery due to ineffective primary endohemostasis. In 2 patients, it was impossible to stop bleeding subserosally due to scar deformation in the surgical intervention zone. Two of them underwent gastric resection and one had suturing of the bleeding ulcer; all patients recovered.Analysis of the results in the control group for Forrest Ia - Ib showed that surgical activity was 8 (26.6%), with gastric resection performed in 5 cases and suturing of bleeding vessels in 3 cases. One patient (3.3%) had a fatal outcome due to peritonitis caused by anastomotic suture failure (Fig. 3).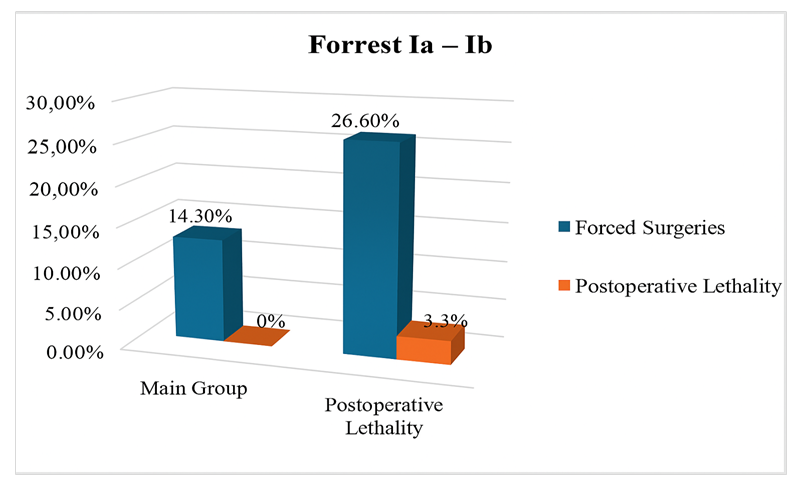 | Figure 3. Frequency of forced surgeries and mortality in Forrest Ia - Ib |
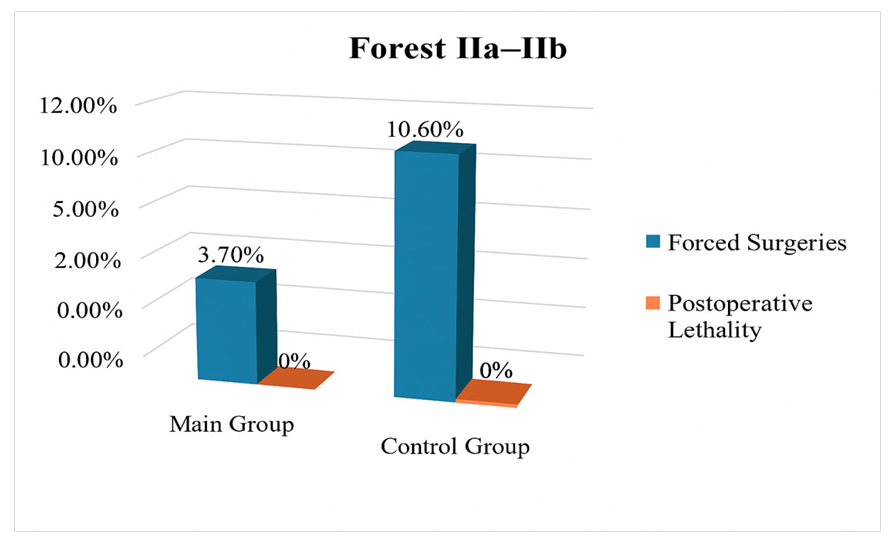
When analyzing the results in the main group and the control group for Forrest IIa-IIb, postoperative activity was observed in 1 patient where no source of hemorrhage was found. However, during the operation, undertaken due to clinical signs of ongoing bleeding, a duodenal ulcer on the posterior wall was detected, necessitating emergency surgery. In the control group, recurrence of bleeding was observed in 5 (10.6%) cases in patients who underwent gastric resection. Postoperative mortality was not observed in either group (Fig. 4).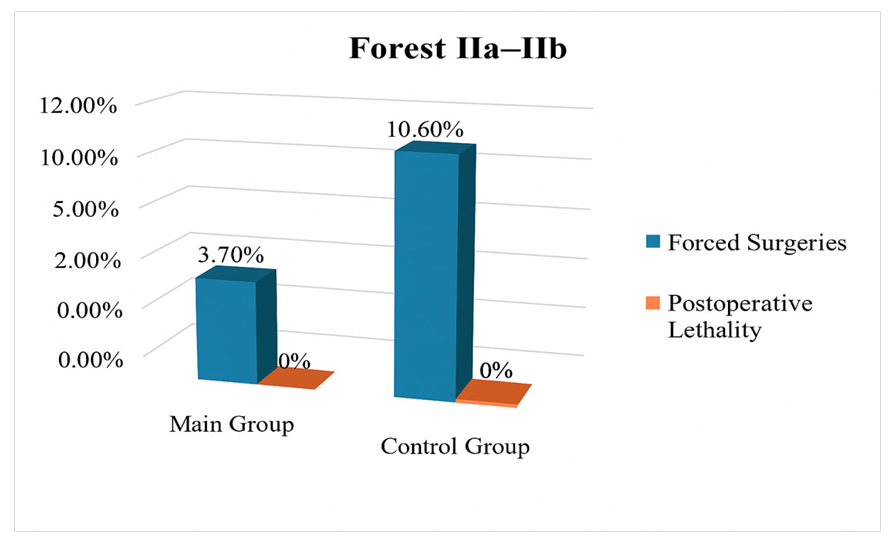 | Figure 4. Frequency of forced surgeries and mortality in Forrest IIa - IIb |
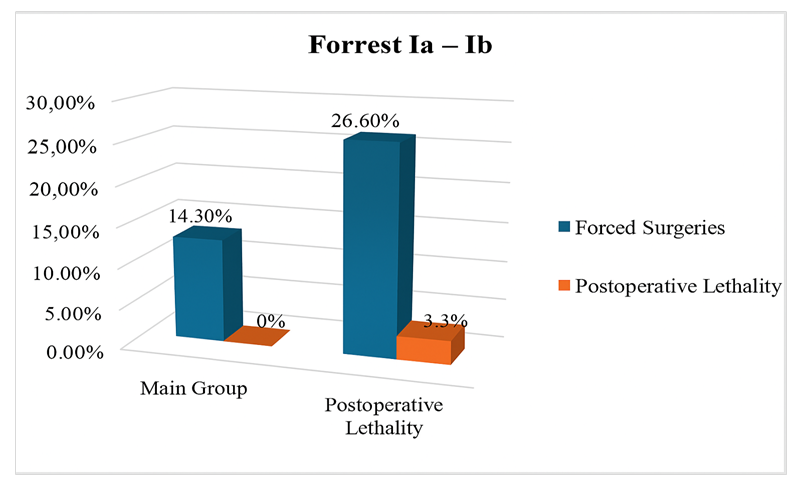
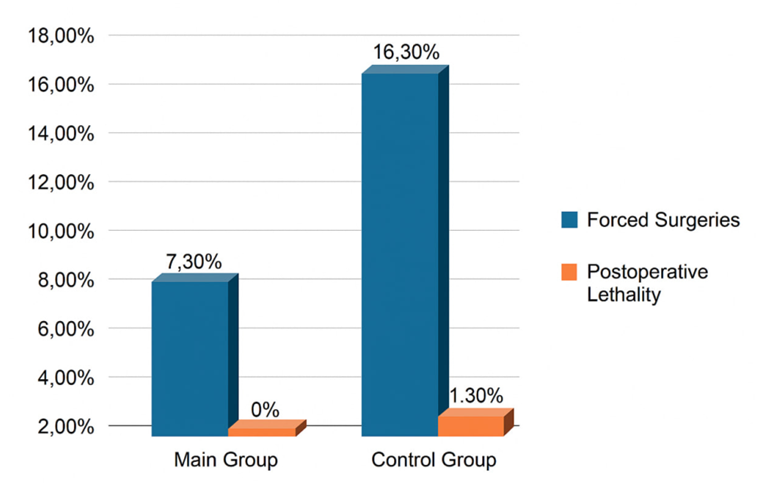
In total, the frequency of forced surgeries in the main group was 3 (7.3%) without fatal cases, while in the control group, surgical activity was 13 (16.33%), with 1 fatal outcome (Fig. 5).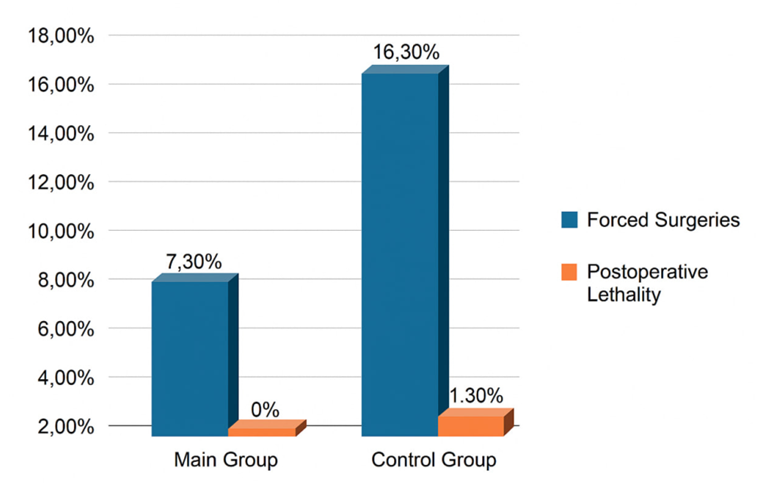 | Figure 5. Overall frequency of forced surgeries and mortality |
Thus, the hybrid endolaparoscopic method we developed showed greater effectiveness compared to other endohemostasis methods. The frequency of forced operations using this method is 7.3% versus 16.3% for injection and electrocoagulation endoscopic methods, and the mortality rate is 0% versus 1.3% for these methods. This allows us to recommend it for stopping gastroduodenal bleeding in clinical practice.
4. Conclusions
1. The most significant factors influencing the development of gastroduodenal ulcer bleeding are: - long history and episodes of bleeding (r=0.44); age and concomitant diseases (r=0.37); - size (r=0.22) and localization of the ulcer (r=0.21); - H. pylori infection (r=0.25). Predicting the risk of hemorrhage recurrence using the improved J. Rockall scale showed 95% specificity and 98.8% sensitivity.2. For patients with a high risk of bleeding according to the J. Rockall risk scale, priority is given to hybrid surgical interventions with laparoscopic suturing of bleeding ulcers using endoscopic navigation and monitoring of hemostasis effectiveness.3. Optimization of tactical and technical aspects of surgical treatment of gastroduodenal ulcer bleeding using hybrid laparoscopic and endoscopic technologies made it possible to reduce the frequency of forced operations in Forrest Ia-Ib from 26.6% to 14.3%, and in Forrest IIa-IIb from 10.6% to 3.7%.4. The developed and clinically implemented high-tech method of hemostasis - laparoscopic suturing of bleeding ulcers with endoscopic navigation - made it possible to reduce the recurrence rate of bleeding from 21.6% with endoscopic injection and 16.3% with endoscopic coagulation to 7.3% with the proposed method, and to eliminate mortality (1.3% in the comparison group).
References
| [1] | Dostalik J. Laparoscopic gastric resection with natural orifice specimen extraction for postulcer pyloric stenosis / J. Dostalik, P. Gunkova, I. Gunka // Wideochir Inne Tech Maloinwazyjne. – 2014. – Vol. 9(2). – P. 282-5. |
| [2] | El Ouali S. Timing of rebleeding in high-risk peptic ulcer bleeding after successful hemostasis: a systematicreview / S.El Ouali, A.Barkun, M. Martel // Can J Gastroenterol Hepatol. – 2014. – Vol. 28(10). – P. 543-8. |
| [3] | Abraham N. S. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin: population based cohort study. / Abraham NS. and [et al.] // BMJ. - 2015. - V. - 350. - P. 1857-1861. |
| [4] | Agreus L. Value of the “Test & Treat” Strategy for Uninvestigated Dyspepsia at Low Prevalence Rates of Helicobacter pylori in the Population. Helicobacter / L. Agreus, N.J. Talley, M. Jones // - 2016. V. -21. - P. 186–191. |
| [5] | Bager P. Randomised clinical trial: oral vs. intravenous iron after upper gastrointestinal haemorrhage--a placebo-controlled study / P. Bager, J.F. Dahlerup // Aliment Pharmacol Ther. -2014 / - V. 39(2). - P. 176–87. |
| [6] | Beales I.L. Decisions on restarting anticoagulation should be made earlier after rebleeding / I.L. Beales // BMJ. - 2016. - P. 532. |
| [7] | Brooks J. Prevention of upper gastrointestinal haemorrhage: current controversies and clinical guidance / J. Brooks, R. Warburton, I.L. Beales // Ther Adv Chronic Dis. – 2013. -V. -4(5). - P. 206–22. |
| [8] | Chan EW. Prevention of Dabigatran-Related Gastrointestinal Bleeding With Gastroprotective Agents: A Population-Based Study / E.W. Chan and [et al] // Gastroenterology. – 2015. -V. - 149(3). - P. 586–95. |
| [9] | Chan FK. Similar Efficacy of Proton-Pump Inhibitors vs H2-Receptor Antagonists in Reducing Risk of Upper Gastrointestinal Bleeding or Ulcers in High-Risk Users of Low-Dose Aspirin / F.K. Chan and [et al.] // Gastroenterology. -2017. - V. - 152(1). - P. 105–110. |
| [10] | Chan SM. of the Over-The-Scope Clip for treatment of refractory upper gastrointestinal bleeding: a case series/ S.M. Chan and [et al.] // Endoscopy. – 2014. - V. - 46(5). - P. 428–31. |
| [11] | Changela K. Hemostatic powder spray: a new method for managing gastrointestinal bleeding. / K Changela, H. Papafragkakis // Therap Adv Gastroenterol. -2015. -V. -8(3). - P. 125–35. |
| [12] | Timerbulatov Sh.V., Timerbulatov M.V., Sagitov R.B., Timerbulatov V.M., Gafarova A.R. Ulcerative gastroduodenal bleeding: current state of the problem // Medical Bulletin of Bashkortostan. - 2020. - T. 15, No. 2. - P. 85–96. |
| [13] | Romantsov M.N., Cherednikov E.F., Bondarenko A.A., Yakushev F.K. New technologies of endoscopic hemostasis in the treatment protocol for patients with gastroduodenal bleeding // Bulletin of experimental and clinical surgery. - 2020. - T. 13, No. 2. - P. 78–84. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML