-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 2003-2004
doi:10.5923/j.ajmms.20251506.83
Received: May 28, 2025; Accepted: Jun. 16, 2025; Published: Jun. 21, 2025

Role of Esophageal Ph-Impedance and Manometric Monitoring in the Therapeutic Strategy for Refractory Gerd
Khodieva O. I.
Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Khodieva O. I., Bukhara State Medical Institute, Bukhara, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Refractory gastroesophageal reflux disease (GERD) remains a significant clinical concern, affecting nearly one-third of patients despite standard proton pump inhibitor (PPI) therapy. This paper explores the diagnostic and therapeutic implications of esophageal pH-impedance and manometric monitoring in managing these challenging cases. By characterizing reflux episodes beyond acid exposure and evaluating esophageal motor function, clinicians can identify phenotypes such as weakly acidic reflux, esophageal hypersensitivity, and ineffective esophageal motility. Our findings reinforce the integration of functional testing into routine GERD management to ensure precision-guided therapy.
Keywords: Refractory GERD, pH-impedance, High-resolution manometry, Esophageal motility, Non-acid reflux, Personalized treatment
Cite this paper: Khodieva O. I., Role of Esophageal Ph-Impedance and Manometric Monitoring in the Therapeutic Strategy for Refractory Gerd, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 2003-2004. doi: 10.5923/j.ajmms.20251506.83.
1. Introduction
- GERD is a prevalent disorder that compromises quality of life and predisposes patients to complications such as Barrett's esophagus [1,2]. While PPIs offer symptomatic relief for most, up to 30% of patients continue to suffer from heartburn, regurgitation, or chest pain. Refractory GERD, defined as the persistence of symptoms despite adequate PPI therapy, necessitates deeper diagnostic evaluation. Traditional endoscopy and pH-metry fail to fully capture non-acidic reflux and motor dysfunctions, prompting reliance on advanced diagnostics: esophageal pH-impedance monitoring and high-resolution manometry (HRM) [3,4].These tools not only quantify acid exposure but also detect the frequency, composition, and clearance of reflux episodes, as well as motility disturbances. This article investigates their role in stratifying patients and tailoring treatment strategies [5].
2. Materials and Methods
- A cohort of 72 adult patients (aged 20–65) with persistent GERD symptoms despite double-dose PPI therapy were enrolled from tertiary gastroenterology clinics. Each patient underwent:• 24-hour multichannel intraluminal impedance and pH monitoring (MII-pH) off therapy• High-resolution esophageal manometry per Chicago Classification v4.0• Symptom association probability (SAP) and symptom index (SI) assessment• Clinical interviews and validated symptom scoringOutcomes evaluated included reflux type, total number of reflux episodes, esophageal motility profiles, and correlation with symptom severity.
3. Results
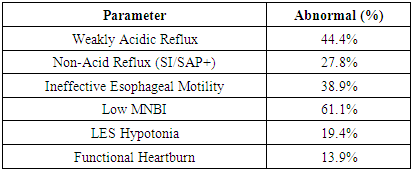
- Out of 72 patients, 52.8% had abnormal pH-impedance parameters, including:
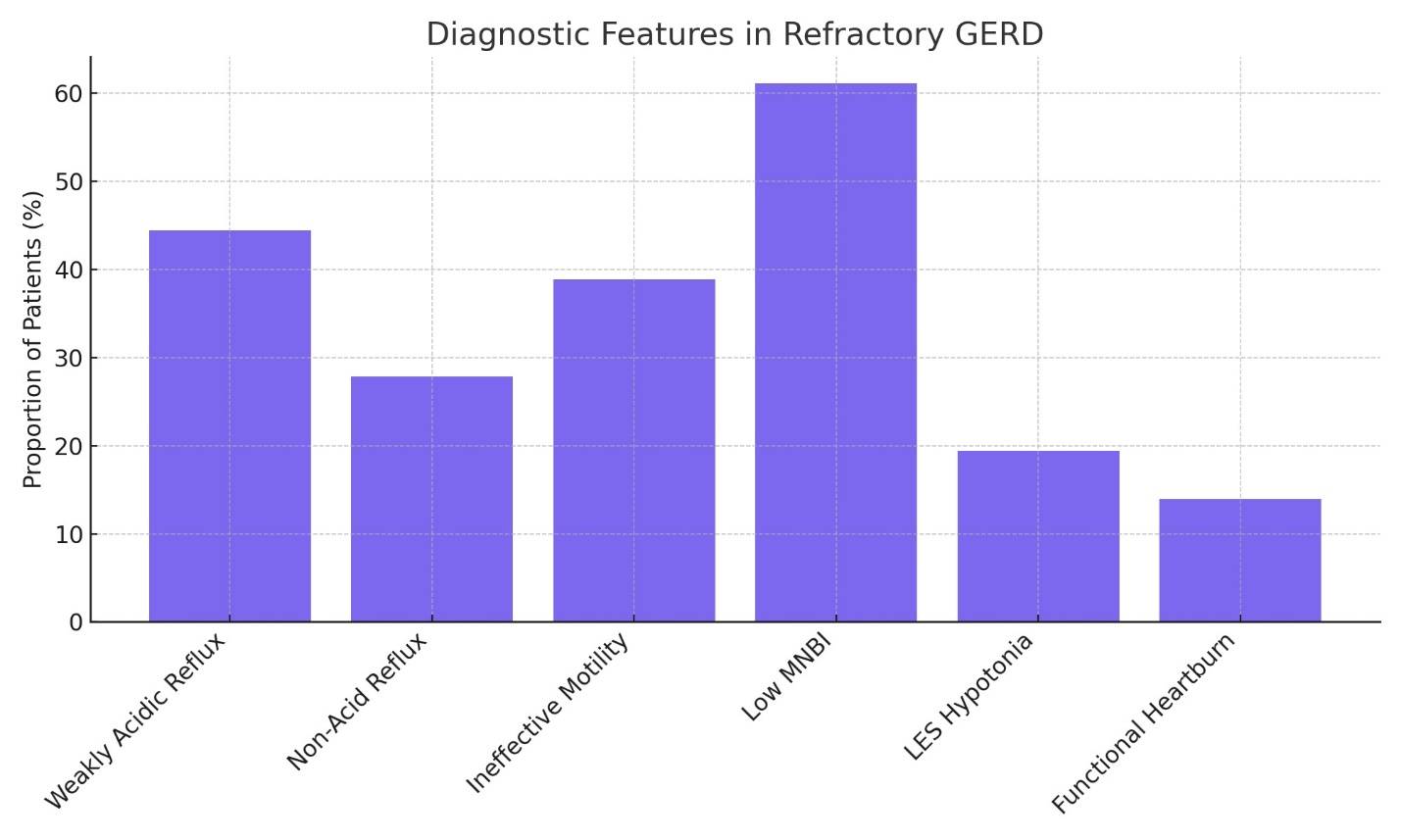 | Figure 1 |
|
4. Discussion
- Our findings illustrate the heterogeneity of refractory GERD and the indispensable role of combined pH-impedance and manometric analysis. Weakly acidic and non-acid reflux often escape detection via standard pH monitoring but can cause significant symptoms. Manometric profiles further delineate subgroups suitable for prokinetics, behavioral therapy, or surgical intervention.Patients with functional heartburn benefit more from neuromodulation than acid suppression. The integration of functional diagnostics not only refines differential diagnosis but enables evidence-based decisions in managing refractory GERD.
5. Conclusions
- Esophageal pH-impedance and manometry are central to the therapeutic strategy for refractory GERD. Their application ensures appropriate targeting of therapy, reduces unnecessary medication use, and improves patient outcomes through individualized care.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML