-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 2001-2002
doi:10.5923/j.ajmms.20251506.82
Received: May 21, 2025; Accepted: Jun. 13, 2025; Published: Jun. 21, 2025

Advanced pH-Impedance and Manometric Profiling in the Diagnostic Algorithm of Refractory Gastroesophageal Reflux Disease
Khodieva O. I.
Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Khodieva O. I., Bukhara State Medical Institute, Bukhara, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Refractory gastroesophageal reflux disease (GERD) poses a diagnostic and therapeutic challenge despite optimal proton pump inhibitor (PPI) therapy. This article explores the role of esophageal pH-impedance monitoring and high-resolution manometry (HRM) in evaluating pathophysiological mechanisms underlying PPI-resistant GERD. Our findings, based on a cohort of patients with persistent symptoms, emphasize the importance of identifying non-acidic reflux, ineffective esophageal motility, and functional disorders. Accurate interpretation of these functional parameters allows for individualized therapy and avoidance of unnecessary surgical or pharmacologic interventions.
Keywords: Refractory GERD, pH-impedance, Esophageal manometry, Weakly acidic reflux, Motility disorders, PPI resistance
Cite this paper: Khodieva O. I., Advanced pH-Impedance and Manometric Profiling in the Diagnostic Algorithm of Refractory Gastroesophageal Reflux Disease, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 2001-2002. doi: 10.5923/j.ajmms.20251506.82.
1. Introduction
- Gastroesophageal reflux disease (GERD) affects up to 20% of adults in developed countries [1]. While most patients respond well to proton pump inhibitors (PPIs), approximately 30% continue to experience symptoms [2,3]. This condition, termed refractory GERD, warrants further investigation using functional diagnostics to reveal underlying causes such as weakly acidic reflux, non-acid reflux, esophageal hypersensitivity, or motility disorders [4,5].
2. Materials and Methods
- Participants:This prospective study included 60 adult patients (age 18–65) with persistent GERD symptoms despite ≥8 weeks of standard-dose PPI therapy. All participants underwent upper GI endoscopy to exclude erosive esophagitis and structural anomalies.Diagnostic protocol included:• 24-hour pH-impedance monitoring off PPI for 7 days• High-resolution manometry following Chicago Classification v4.0• Symptom-reflux association analysis (SAP, SI)• Reflux episode characterization: acidic, weakly acidic, non-acid• Post-reflux swallow-induced peristaltic wave index (PSPW)• Mean nocturnal baseline impedance (MNBI)Exclusion criteria:Previous anti-reflux surgery, esophageal strictures, eosinophilic esophagitis, major psychiatric comorbidities.
3. Results
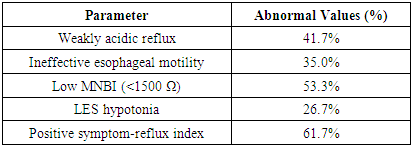
- • Acidic reflux was present in 31.7% of patients, while non-acidic reflux predominated in 41.7%.• 28.3% of patients demonstrated normal acid exposure, but abnormal symptom association (suggestive of reflux hypersensitivity).• MNBI was significantly lower (<1500 Ω) in patients with confirmed reflux vs functional heartburn (p<0.01).• HRM revealed ineffective esophageal motility in 35% and fragmented peristalsis in 18.3%.• LES hypotonia was detected in 26.7% of cases, associated with higher DeMeester scores.• PSPW index was significantly lower in patients with delayed reflux clearance.
|
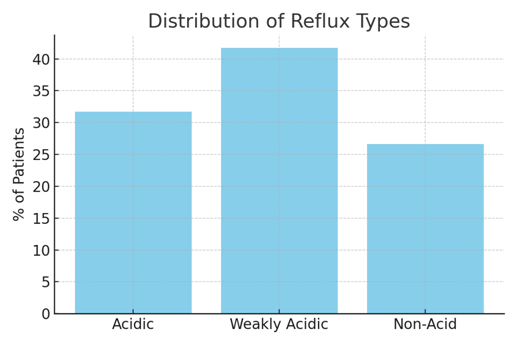 | Figure 1. Distribution of Reflux Types by Impedance-pH Monitoring |
4. Discussion
- Our study confirms the multifactorial nature of refractory GERD. While acid suppression remains central to therapy, nearly half of patients suffer from non-acid reflux, which goes undetected with conventional pH monitoring alone. MII-pH and HRM provide deeper insight, especially in identifying weak peristalsis and abnormal clearance mechanisms. The MNBI and PSPW indices emerged as valuable predictors of mucosal integrity and esophageal function.Based on functional phenotyping, patients can be reclassified for targeted therapy: neuromodulators in hypersensitivity, prokinetics in motility disorders, or consideration of anti-reflux surgery in confirmed pathological reflux with LES incompetence.
5. Conclusions
- pH-impedance monitoring and high-resolution manometry are indispensable tools in the modern management of refractory GERD. Their integration into diagnostic algorithms allows accurate classification of patients and supports individualized treatment plans beyond acid suppression.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML