-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1999-2000
doi:10.5923/j.ajmms.20251506.81
Received: May 22, 2025; Accepted: Jun. 13, 2025; Published: Jun. 21, 2025

Clinical Characteristics of Cardiomyopathy Progression in Type 2 Diabetes Mellitus Patients Residing in Hot Climate Regions
F. A. Ikramova
Bukhara State Medical University, Bukhara, Uzbekistan
Correspondence to: F. A. Ikramova, Bukhara State Medical University, Bukhara, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Cardiomyopathy in patients with type 2 diabetes mellitus (T2DM) is a major contributor to cardiovascular morbidity and mortality. This study investigates the clinical and pathophysiological features of cardiomyopathy progression in T2DM patients living in hot climatic conditions. Environmental stressors such as chronic heat exposure, dehydration, and altered circadian rhythms may exacerbate cardiac dysfunction and accelerate disease progression. The study analyzes a cohort of diabetic patients from the Bukhara region, assessing biochemical, echocardiographic, and clinical parameters over a 12-month period. Results suggest that elevated ambient temperatures correlate with increased myocardial stiffness, diastolic dysfunction, and autonomic imbalance. The findings underscore the need for region-specific guidelines in managing cardiovascular complications in diabetic patients.
Keywords: Type 2 diabetes mellitus, Cardiomyopathy, Hot climate, Diastolic dysfunction, Myocardial remodeling, Environmental stress
Cite this paper: F. A. Ikramova, Clinical Characteristics of Cardiomyopathy Progression in Type 2 Diabetes Mellitus Patients Residing in Hot Climate Regions, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1999-2000. doi: 10.5923/j.ajmms.20251506.81.
1. Introduction
- Type 2 diabetes mellitus (T2DM) is globally recognized as a metabolic disorder with extensive cardiovascular implications. One of the less overt yet critically important complications is diabetic cardiomyopathy (DCM), characterized by structural and functional changes in the myocardium independent of hypertension and coronary artery disease [1,2]. In regions with hot climates, such as Central Asia and parts of the Middle East and Africa, environmental factors may significantly influence the course and severity of DCM [3].Chronic heat exposure can induce dehydration, oxidative stress, and sympathetic nervous system overactivation, all of which may negatively affect cardiac metabolism and electrophysiology [4]. Moreover, changes in physical activity patterns, medication pharmacokinetics, and glycemic variability in response to climatic extremes further complicate disease management [5,6]. Despite the increasing prevalence of T2DM in these regions, limited data exists regarding the interplay between climate and cardiac pathology. This study aims to elucidate the unique clinical characteristics of cardiomyopathy progression in T2DM patients residing in hot climate zones [7,8].
2. Materials and Methods
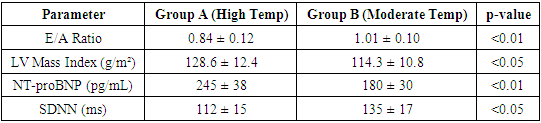
- This observational study included 120 patients aged 40–65 with confirmed T2DM and echocardiographic signs of early-stage cardiomyopathy, residing in the Bukhara region of Uzbekistan. The cohort was followed for 12 months. Exclusion criteria included uncontrolled hypertension, ischemic heart disease, and congenital heart defects.Parameters assessed included:• HbA1c, fasting glucose, lipid profile• NT-proBNP and high-sensitivity CRP levels• Echocardiographic evaluation (EF, E/A ratio, LV mass index, global longitudinal strain)• Heart rate variability (HRV) and 24-hour Holter monitoring• Ambient temperature and humidity recordings during the study periodPatients were divided into two subgroups based on seasonal temperature exposure: Group A (summer peak months >38°C average), and Group B (moderate months <30°C average).
3. Results
- Patients exposed to sustained high temperatures (Group A) demonstrated a statistically significant decline in diastolic function (E/A ratio 0.84±0.12 vs. 1.01±0.10 in Group B; p<0.01), increased LV mass index, and elevated NT-proBNP levels. HRV analysis indicated pronounced autonomic dysfunction in Group A, with reduced SDNN and RMSSD values.The prevalence of subclinical arrhythmias and episodes of nocturnal hypertension was higher in Group A. Furthermore, self-reported symptoms such as fatigue, palpitations, and dyspnea on exertion were more frequent during heatwave periods. Multivariate analysis identified ambient temperature, NT-proBNP, and HRV indices as independent predictors of myocardial functional decline.
|
4. Discussion
- The study highlights the amplifying effect of hot climatic conditions on cardiomyopathy progression in diabetic patients. Heat-induced vasodilation, fluid-electrolyte imbalance, and increased myocardial oxygen demand may exacerbate pre-existing metabolic and structural cardiac abnormalities. These findings advocate for tailored clinical approaches including adjusted medication schedules, hydration strategies, and cardiac monitoring during summer months.
5. Conclusions
- Cardiomyopathy in T2DM patients shows distinct clinical deterioration under hot climate exposure. Healthcare providers in arid and tropical regions must adopt climate-aware cardiovascular management strategies to mitigate disease burden in diabetic populations.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML