-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1995-1998
doi:10.5923/j.ajmms.20251506.80
Received: May 25, 2025; Accepted: Jun. 16, 2025; Published: Jun. 21, 2025

Modified Treatment and Diagnostic Algorithm for the Prevention of Mediastinitis in Neck Phlegmons
Okhunov A. O.1, Boboev K. Kh.2
1Professor, Doctor of Medical Sciences, Head of the Department of General and Pediatric Surgery-1, Tashkent Medical Academy, Tashkent, Uzbekistan
2Assistant of the Department of General and Pediatric Surgery-1, Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Neck phlegmons are associated with a high risk of developing descending mediastinitis, which determines an unfavorable prognosis of the disease. The aim of the study was to compare the effectiveness of traditional surgical tactics with a modified treatment and diagnostic algorithm aimed at preventing mediastinitis. The study included 92 patients divided into a control group (n=35) and a main group (n=29). In the main group, a risk stratification system was applied based on clinical, laboratory, and imaging data, followed by personalized selection of the extent of surgical intervention and antibacterial therapy. The results demonstrated a significant reduction in the incidence of mediastinitis (3.4% vs. 28.6%; p<0.01), a decrease in the number of reoperations, reduced mortality, and shorter hospitalization duration in the main group. The dynamics of inflammatory markers (C-reactive protein, procalcitonin, lactate) indicated a faster resolution of systemic inflammation. The implementation of the modified algorithm improved the clinical effectiveness of treatment and reduced the risk of severe complications in patients with neck phlegmons.
Keywords: Neck phlegmons, Descending mediastinitis, Prevention, Risk stratification, Surgical tactics
Cite this paper: Okhunov A. O., Boboev K. Kh., Modified Treatment and Diagnostic Algorithm for the Prevention of Mediastinitis in Neck Phlegmons, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1995-1998. doi: 10.5923/j.ajmms.20251506.80.
1. Introduction
- Neck phlegmons represent a severe pathology characterized by the rapid spread of infection through deep fascial spaces, posing a high risk of life-threatening complications. The most dangerous outcome is descending mediastinitis, which, according to literature data, is associated with a mortality rate of up to 60% in cases of delayed intervention [1,2].Despite the accumulated clinical experience in treating neck phlegmons, traditional tactics focused on local abscess incision without active revision of the retropharyngeal, retrofaryngeal, and paratracheal spaces often prove insufficient to prevent the downward spread of infection. The lack of prognostic risk stratification and standardized intervention algorithms leads to high variability in outcomes and frequent complications, particularly in patients with concomitant metabolic disorders [3].Current evidence highlights the need to shift toward proactive treatment strategies for neck phlegmons, based on early assessment of mediastinitis risk, extensive surgical debridement of potentially involved anatomical zones, and the use of active drainage and vacuum therapy methods. In this context, a critical task is the implementation of treatment and diagnostic algorithms that not only predict the likelihood of descending infection spread but also personalize the extent of surgical intervention and the intensity of postoperative monitoring [4,5].The aim of this study was to compare the effectiveness of traditional surgical tactics for treating neck phlegmons with a modified treatment and diagnostic algorithm designed to prevent descending mediastinitis. The evaluation included an analysis of the incidence of complications, the structure of reoperations, the dynamics of clinical and laboratory parameters, the duration of hospitalization, and overall mortality.
2. Materials and Methods
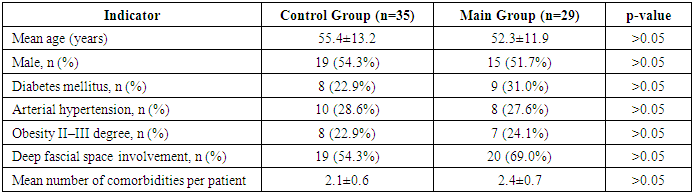
- The study included 92 patients with neck phlegmons of odontogenic etiology treated at the Center for Purulent Surgery and Surgical Complications of Diabetes at the Multidisciplinary Clinic of the Tashkent Medical Academy from 2015 to 2024. Depending on the applied treatment tactics, patients were divided into three groups: control (n=35), comparative (n=28), and main (n=29).The control group consisted of patients with neck phlegmons without signs of descending infection spread, who received traditional treatment involving limited incision of the local abscess and placement of passive drains. The comparative group included patients who developed descending mediastinitis during standard treatment, requiring extensive surgical interventions at the complication stage. The main group comprised patients managed with a developed modified treatment and diagnostic algorithm for the prediction and prevention of mediastinitis, based on early risk stratification and individualized surgical tactics.The diagnostic program for all patients included clinical and laboratory examinations (levels of leukocytes, neutrophils, C-reactive protein, procalcitonin, albumin, lactate), microbiological analysis of purulent discharge, and multispiral computed tomography (MSCT) of the neck and upper mediastinum with intravenous contrast enhancement.The essence of the treatment and diagnostic algorithm was the early stratification of mediastinitis risk based on a comprehensive assessment of clinical, laboratory, and imaging data. After calculating an individual prognostic score, patients in the main group were classified into risk levels: low, moderate, high, and very high, which determined the nature of subsequent therapeutic measures.For patients with low risk, in the absence of signs of deep fascial space involvement and systemic inflammation, standard surgical tactics were applied, including incision of the local purulent focus and placement of passive drains. As the prognostic risk increased, treatment tactics were modified: in patients with moderate risk, extended revision of adjacent fascial spaces was performed, counter-apertures were formed to ensure adequate drainage, and enhanced antibacterial therapy was prescribed.The most radical tactics were applied in patients with high and very high risk. In these cases, revision of the retropharyngeal and retrofaryngeal spaces was mandatory, and in the presence of CT signs of early mediastinal involvement, preventive mediastinotomy was performed. Active drainage was carried out using irrigation-suction systems or negative pressure wound therapy (NPWT), which ensured control over deep inflammatory sites. In the postoperative period, strict monitoring of clinical and laboratory parameters and dynamic CT evaluation were conducted for timely adjustment of treatment tactics.The effectiveness of the proposed algorithm was assessed based on the incidence of mediastinitis, septic complications, the number of reoperations, duration of hospitalization, mortality rate, and clinical-economic efficiency indicators (OMES scale).Statistical data analysis was performed using the Student’s t-test, Mann-Whitney U-test, χ² test, and Fisher’s exact test for qualitative data. The prognostic value of the model was evaluated using ROC analysis with the calculation of the area under the curve (AUC). The statistical significance level was set at p<0.05.Analysis of the baseline characteristics of patients in the control and main groups showed that differences in age, gender, frequency of comorbidities (diabetes mellitus, arterial hypertension, obesity), and signs of deep fascial space involvement did not reach statistical significance (p>0.05). This indicates the comparability of the groups in terms of key demographic and clinical parameters, ensuring the validity of the subsequent comparative analysis of treatment tactics’ effectiveness (Table 1).
|
3. Results
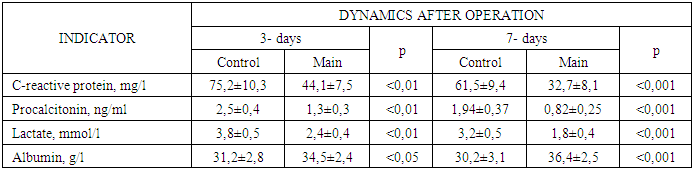
- Analysis of the treatment outcomes in the control and main groups revealed significant differences in the incidence of complications, the structure of reoperations, the duration of hospitalization, and mortality rates, indicating the high effectiveness of the modified treatment and diagnostic algorithm for preventing mediastinitis.Descending mediastinitis was recorded in 1 out of 29 patients (3.4%) in the main group and in 10 out of 35 patients (28.6%) in the control group (p<0.01). The more than eightfold reduction in the incidence of mediastinitis underscores the critical importance of active risk stratification and timely extended intervention in preventing complicated disease progression. The incidence of septic shock was also significantly lower in the main group (3.4%) compared to the control group (11.4%), although these differences did not reach statistical significance (p>0.05).The need for reoperations differed significantly. In the main group, 75.9% of patients required only one surgical intervention, whereas in the control group, only 32.1% of patients avoided reoperations (p<0.01). This reflects the high completeness and radicality of primary interventions when using the proposed algorithm.The average duration of hospitalization in the main group was 17.8±3.5 days, which was statistically significantly shorter compared to the control group, where this indicator reached 27.4±4.1 days (p<0.001). The reduction in hospital stay was associated with both the prevention of mediastinitis and the faster stabilization of patients' conditions.Mortality in the main group was 3.4% (1 case out of 29), while in the control group, it reached 17.1% (6 cases out of 35) (p<0.05), confirming the high clinical effectiveness of the modified treatment and diagnostic approach.Additionally, the main group showed a significant improvement in OMES scale scores, reflecting not only a reduction in complication rates but also an accelerated restoration of patients' social and occupational status.Evaluation of the dynamics of key laboratory indicators of systemic inflammatory response and metabolic status demonstrated significant differences between the control and main groups following treatment (Table 2).
|
4. Discussion
- The obtained results convincingly demonstrate the high effectiveness of the modified treatment and diagnostic algorithm aimed at preventing descending mediastinitis in patients with neck phlegmons of odontogenic etiology. A significant reduction in the incidence of mediastinitis, a decrease in the number of reoperations, a statistically significant reduction in hospitalization duration, and a decrease in mortality reflect the advantages of an individualized approach based on early risk stratification and proactive surgical tactics. The use of the algorithm was associated with a faster resolution of the inflammatory response: levels of C-reactive protein, procalcitonin, and lactate decreased significantly more rapidly, and albumin levels stabilized earlier compared to traditional tactics. These results underscore the critical role of timely intervention and comprehensive postoperative monitoring in preventing severe septic complications.The data from this study align with the findings of international researchers, who emphasize the importance of early active debridement of deep fascial spaces and the use of active drainage systems in reducing the risk of descending mediastinitis [6]. In particular, according to L.F. Wang and co-authors, mediastinitis predominantly develops due to delayed revision of the retrofaryngeal space and the absence of preventive mediastinotomies [1]. The application of the algorithm in our study not only reduced the incidence of complications but also minimized the consequences of systemic inflammatory response, as evidenced by the dynamics of procalcitonin and lactate levels.An important aspect is the confirmation of the high clinical significance of laboratory and imaging prognostic criteria. Elevated levels of C-reactive protein, procalcitonin, hypoalbuminemia, and CT signs of retropharyngeal involvement became integral components of the early risk diagnostic system, which aligns with modern concepts of stratified surgical care [6]. The implementation of this model in clinical practice enables a shift from reactive surgery to proactive control of severe purulent neck infections.
5. Conclusions
- This study was aimed at improving the treatment tactics for neck phlegmons of odontogenic etiology to prevent descending mediastinitis, one of the most severe and life-threatening complications of this pathology. Based on the analysis of clinical, laboratory, microbiological, and imaging data, a modified treatment and diagnostic algorithm was developed and implemented, integrating principles of early prognostic risk stratification and proactive individualized surgical tactics.A comparative evaluation of the effectiveness of the traditional approach and the proposed algorithm demonstrated the compelling advantages of the modified tactics. The implementation of the algorithm significantly reduced the incidence of mediastinitis, decreased the number of reoperations, shortened hospitalization duration, and lowered mortality rates. The dynamics of key laboratory indicators—reduced levels of C-reactive protein, procalcitonin, lactate, and stabilization of albumin—also confirmed a faster resolution of the inflammatory response and restoration of tissue homeostasis in patients treated according to the new model.The development and implementation of the treatment and diagnostic algorithm for preventing descending mediastinitis enabled a shift from reactive to proactive surgical strategies, ensuring not only improved clinical effectiveness but also optimized healthcare resource utilization. The obtained results highlight the high practical value of the stratified approach and justify its application in real clinical practice to reduce disease severity, shorten treatment duration, and improve long-term outcomes in patients with deep neck infections.Ethical Approval: The study was conducted in accordance with the Declaration of Helsinki of the World Medical Association (2013) and was approved by the local ethics committee of the Tashkent Medical Academy. All patients provided informed voluntary consent to participate in the study.Funding: The study was not funded. The authors conducted the work as part of their primary scientific activities.Conflict of Interest: The authors declare no apparent or potential conflicts of interest related to the publication of this article.Author Contributions: All authors made equal contributions to the development of the study concept, data collection, analysis, and interpretation, preparation of the manuscript, and approval of its final version for publication.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML