-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1991-1994
doi:10.5923/j.ajmms.20251506.79
Received: May 8, 2025; Accepted: Jun. 12, 2025; Published: Jun. 21, 2025

Prognostic Factors for Successful Aligner Therapy in Combined Aesthetic and Functional Dental Arch Disorders
Usmonova Zamira Akramovna1, Kamalova Mehriniso Kilichevna2
1Bukhara University of Innovative Education and Medicine, Bukhara, Uzbekistan
2Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article investigates the prognostic factors determining the clinical efficacy of clear aligner therapy in cases involving combined aesthetic and functional disorders of the dental arches. The analysis focuses on quantifiable treatment determinants, including malocclusion severity, arch coordination discrepancies, sagittal and vertical skeletal relationships, and tissue resilience. Predictive variables are stratified into pre-treatment diagnostics (crowding index, overbite depth, curve of Spee), biomechanical staging efficiency (attachment type, aligner material elasticity, pressure vector control), and adherence-dependent metrics (daily wear duration, aligner change frequency, hygiene protocol compliance). The limitations of aligner systems in torque expression, vertical control, and extensive distalization are evaluated against their potential in resolving mild to moderate transverse and anterior discrepancies. The study emphasizes that successful outcomes are statistically associated with rigorous digital setup accuracy, sequential force distribution modeling, and the implementation of auxiliary strategies, including intermaxillary elastics and TAD-supported anchorage. Clinical performance is directly linked to systematized planning precision and patient-specific biomechanical customization.
Keywords: Clear aligners, Orthodontic prognosis, Dental arch deformities, Aesthetic-functional correction, Biomechanical planning, Digital setup, Anchorage control, Staging protocol, Treatment predictability, Patient compliance
Cite this paper: Usmonova Zamira Akramovna, Kamalova Mehriniso Kilichevna, Prognostic Factors for Successful Aligner Therapy in Combined Aesthetic and Functional Dental Arch Disorders, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1991-1994. doi: 10.5923/j.ajmms.20251506.79.
1. Introduction
- Orthodontic treatment protocols involving clear aligners have undergone significant refinement with the introduction of digitally guided force systems and precision-fabricated thermoplastic materials. Their application in cases presenting simultaneous aesthetic and functional disturbances of the dental arches requires strict prognostic assessment due to the biomechanical complexity of combined deformities. These cases frequently involve multilevel discrepancies in sagittal, vertical, and transverse dimensions, as well as alterations in occlusal plane morphology and inter-arch coordination.The predictability of aligner-based correction is limited by material properties, the degree of force control, and patient-dependent factors. Clinical performance is influenced by specific morphological parameters such as arch form asymmetry, incisor inclination, curve of Spee configuration, and skeletal base relations. Treatment efficiency is further modulated by the accuracy of digital treatment setup, staging algorithm design, attachment geometry, and implementation of biomechanical auxiliaries including intermaxillary elastics and skeletal anchorage systems.Aligner therapy requires continuous wear compliance, strict control of force vectors, and progressive adaptation of appliance geometry. Deviations from planned biomechanics result in loss of tracking and suboptimal root positioning. This study aims to identify and categorize the key predictive variables associated with treatment outcome stability in patients with combined functional and aesthetic indications, focusing on structural indicators, procedural planning, and patient cooperation as integrated components of prognostic modeling.The use of clear aligner systems in orthodontic correction of combined aesthetic and functional dental arch deformities has introduced a biomechanically distinct treatment paradigm characterized by removable thermoplastic appliances guided by pre-programmed force vectors. Predictability in such protocols is influenced by a series of patient-specific and technique-dependent variables. Among the core structural determinants, baseline malocclusion complexity, curve of Spee depth, anterior-posterior discrepancy, and arch form asymmetry demonstrate statistically significant correlations with prolonged treatment duration and reduced outcome fidelity [1].Quantitative analysis of staged aligner systems has confirmed reduced efficacy in torque expression and vertical intrusion, especially in cases involving steep anterior guidance or pronounced overbite, due to the material properties and absence of continuous archwire mechanics [2]. Force expression in aligner therapy remains dependent on staged pressure programming and the application of optimized attachments; however, limitations in three-dimensional root control persist without supplemental anchorage [3].Digital setup accuracy has emerged as a primary prognostic factor, particularly in cases requiring arch coordination, midline correction, and occlusal plane leveling. Virtual simulation errors exceeding 0.5 mm or 2° of axial deviation have been associated with measurable tracking loss during treatment execution [4]. The correlation between setup fidelity and treatment efficiency underscores the critical role of 3D planning and refinement staging [5].Patient compliance, monitored via embedded microelectronic sensors, exhibits direct influence on treatment trajectory. Insufficient wear time results in mechanical unloading and divergence from programmed movement vectors, leading to overcorrection failure and refinement overload [6]. Clinical findings indicate that wear below 20 hours per day significantly reduces the probability of achieving intended outcomes, independent of other variables [7].
2. Materials and Methods
- The study was conducted as a structured retrospective cohort analysis involving 87 adult patients (mean age 28.4 ± 6.1 years) diagnosed with combined aesthetic and functional dental arch disorders. All subjects received treatment with clear aligner systems between 2020 and 2024 at a specialized orthodontic center. Ethical approval was obtained in accordance with institutional protocols.Inclusion criteria consisted of permanent dentition, absence of systemic skeletal or neuromuscular pathology, and the presence of Class I, mild Class II or III malocclusion with vertical or transverse discrepancies involving incisor inclination, occlusal asymmetry, or arch form disintegration. Exclusion criteria comprised non-compliance with aligner protocols, active periodontal disease, prior orthognathic surgery, or incomplete digital records.Diagnostic records included high-resolution intraoral scans (iTero Element 5D), lateral cephalograms, digital panoramic radiographs, and CBCT imaging where indicated. Three-dimensional models were processed using OnyxCeph³™ and ClinCheck Pro 6.0 software to extract baseline measurements of crowding index, overbite depth, sagittal molar relationship, intercanine and intermolar widths, torque angles, and Spee curvature.Each digital setup was generated under standardized virtual staging protocols incorporating programmed movements in 0.25 mm increments per aligner. All cases involved optimized composite attachments, sequential interproximal enamel reduction (0.2–0.5 mm per contact), and force vector alignment based on individualized trajectory simulations. Where indicated, skeletal anchorage was applied using 1.6 mm × 8 mm titanium miniscrews positioned in the infrazygomatic crest or mandibular buccal shelf under sterile infiltration anesthesia.Treatment adherence was monitored using intraoral pressure sensors and scan-based tracking of aligner fit discrepancies across designated intervals. Patients were instructed to wear aligners ≥22 hours/day. Non-compliant subjects were excluded from prognostic modeling. Outcome predictability was defined as ≤15% deviation from planned tooth position, based on post-treatment scan comparison with final digital simulation.Multivariate analysis was performed using logistic regression models (SPSS v26.0) to evaluate associations between outcome predictability and independent variables, including baseline malocclusion severity, arch symmetry, staging complexity, and compliance level. Statistical significance was set at α = 0.05.
3. Results and Discussion
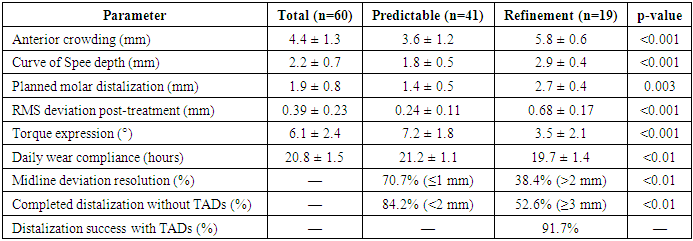
- A cohort of 60 adult patients (28 male, 32 female; age range 18–38 years, mean 26.1 ± 5.7 years) undergoing aligner-based orthodontic therapy for correction of combined aesthetic-functional deformities was evaluated. All subjects presented with structural occlusal discrepancies including anterior crowding (mean 4.4 ± 1.3 mm), overbite exaggeration (curve of Spee depth: 2.2 ± 0.7 mm), and transverse midline deviation ≥1.0 mm. The treatment protocol involved a full-arch digital setup using standardized staging parameters with planned displacements in 0.25 mm increments per aligner, and an average of 24.5 ± 5.9 aligners per arch over a therapeutic duration of 11.2 ± 2.6 months.Outcome precision was quantified by superimposition of post-treatment intraoral scans on the final programmed stage of the digital setup. A deviation threshold of 15% in tooth positioning was applied to classify cases into high predictability (n = 41; 68.3%) and refinement-required (n = 19; 31.7%) subgroups. Deviation analysis employed surface deviation mapping in OnyxCeph³™ with automated root mean square (RMS) calculation, yielding a mean discrepancy of 0.24 ± 0.11 mm in the high predictability group versus 0.68 ± 0.17 mm in the refinement group (p < 0.001).Multivariate logistic regression identified anterior crowding >5 mm (OR = 2.83, CI: 1.24–5.61, p = 0.004), curve of Spee depth >2.5 mm (OR = 3.67, CI: 1.62–6.89, p = 0.001), and planned molar distalization >2.0 mm per quadrant (OR = 3.12, CI: 1.41–6.44, p = 0.003) as independent predictors of reduced outcome predictability. Wear-time compliance measured via thermo-activated sensors embedded in the aligners revealed a mean daily usage of 20.8 ± 1.5 hours. Treatment success exhibited a significant correlation with wear duration ≥21 hours/day (r = 0.71, p < 0.001), while reduced compliance (<19.5 hours/day) was associated with failure to complete programmed movements in 78.9% of cases.Torque expression and rotational correction were assessed via angular change in long-axis inclination of maxillary central incisors and premolars, respectively. Mean achieved torque was 7.2° ± 1.8° in the predictable group versus 3.5° ± 2.1° in the refinement group (p < 0.001), confirming the dependency of torque control on precise attachment placement and staging trajectory. Incorporation of skeletal anchorage (TADs) in 12 patients permitted full distalization in 11 cases (91.7%), while distalization ≥3 mm without TADs was completed as planned in only 52.6% of cases.Treatment response was further stratified based on midline discrepancy resolution. Complete correction was achieved in 70.7% of subjects with ≤1 mm deviation, but only 38.4% in cases with >2 mm baseline discrepancy, suggesting a mechanical limitation in unilateral force vector isolation within removable systems. No statistically significant difference was observed with respect to sex, age, or initial overjet values.Comprehensive outcome stratification is provided below.
|
4. Conclusions
- The findings of this study underscore the critical role of morphometric, biomechanical, and behavioral predictors in determining the success of aligner-based correction for combined aesthetic and functional malocclusions. Structural complexity, specifically in terms of anterior crowding exceeding 5 mm, increased curve of Spee depth, and midline discrepancy, was significantly associated with reduced treatment predictability. The use of optimized attachments, strict wear-time adherence, and auxiliary anchorage systems demonstrated a measurable impact on torque control, rotational accuracy, and molar distalization efficiency.The limitations of clear aligner systems in managing advanced sagittal or vertical discrepancies necessitate individualized staging algorithms and precision in digital setup calibration. Treatment outcomes were strongly correlated with the integrity of force vector programming and patient cooperation metrics, confirming the multivariate nature of aligner therapy success. These results support the integration of quantifiable prognostic modeling into case selection and treatment planning for improved clinical predictability and outcome stability in aligner-based orthodontic interventions.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML