-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1980-1982
doi:10.5923/j.ajmms.20251506.76
Received: May 25, 2025; Accepted: Jun. 13, 2025; Published: Jun. 21, 2025

Effectiveness of Dwips MRI Imaging and Use of Interleukin-6 Inhibitors in Takayasu Arteritis
Akmal Abdullayevich Irnazarov1, 2, Abdurasul Abdujalilovich Yulbarisov1, 2, Khojiakbar Kashipovich Alidjanov1, 2, Saidjon Khomitali ugli Rakhmataliyev1
1Republican Specialized Center of Surgical Angioneurology, Tashkent, Uzbekistan
2Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Saidjon Khomitali ugli Rakhmataliyev, Republican Specialized Center of Surgical Angioneurology, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article discusses the diagnostic value of the DWIPS MRI method in Takayasu arteritis and the therapeutic efficacy of interleykin-6 (IL-6) inhibitors in treatment [2,3]. MRI with DWIPS allows early detection of vascular wall inflammation [1,3,5]. At the same time, IL-6 inhibitors, particularly drugs like tocilizumab, are considered effective in controlling the chronic inflammatory process of the disease [4].
Keywords: Takayasu arteritis, Interleykin-6 (IL-6), MRI DWIPS, CRP, MSCTA, Carotid artery, ESR, Tocilizumab
Cite this paper: Akmal Abdullayevich Irnazarov, Abdurasul Abdujalilovich Yulbarisov, Khojiakbar Kashipovich Alidjanov, Saidjon Khomitali ugli Rakhmataliyev, Effectiveness of Dwips MRI Imaging and Use of Interleukin-6 Inhibitors in Takayasu Arteritis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1980-1982. doi: 10.5923/j.ajmms.20251506.76.
1. Introduction
- Takayasu arteritis is a chronic granulomatous vasculitis of unknown etiology that predominantly affects large arteries, especially the aorta and its major branches. Early and precise visualization methods, particularly MRI DWIPS technology, play an important role in diagnosis. In treatment, beyond conventional immunosuppressive therapy, the use of biological agents — IL-6 inhibitors — is increasingly emphasized.Takayasu Arteritis: Pathogenesis and Clinical Features [7,9,14]• Autoimmune in nature.• Manifests with stenosis, occlusion, or aneurysms in the aorta and brachiocephalic branches [8].• Symptoms: fatigue, signs of ischemia, pulse deficit, headache, visual disturbances, and hypertension.Significance of DWIPS MRIWhat is DWIPS?DWIPS — "Diffusion-Weighted Imaging with Background Suppression" — is an MRI technology with high sensitivity to detect inflammatory processes in parenchymal tissues [10,16].Capabilities of DWIPS in Takayasu Arteritis:• Detects inflammatory activity in the arterial wall [2,8,15].• Identifies active vasculitis without contrast agents.• Assesses treatment efficacy.Interleukin-6 Inhibitors: A Modern Therapeutic ApproachRole of IL-6• IL-6 is a key cytokine involved in inflammation, and its level is elevated in Takayasu arteritis.• Contributes to edema, fever, and increased ESR and CRP levels [10,12].Tocilizumab and Other Inhibitors• Tocilizumab is a monoclonal antibody that blocks IL-6 receptors.• Clinical studies show that tocilizumab reduces vasculitis activity and increases the likelihood of remission [11,13,16].
2. Material and Methods
- A retrospective analysis of the surgical treatment of 42 patients with NAA who were hospitalized at the Republican Center for Surgical Angioneurology and at the Department of Vascular Surgery of the Multidisciplinary Clinic of the Tashkent Medical Academy in the period 2019-2024 was carried out.Clinical CasesPatient X, 32 years old, presented to the Republican Specialized Center of Surgical Angioneurology in 2016 with complaints of neck pain, dizziness during physical exertion, and low-grade fever. Nonspecific aortoarteritis (NSAA) had been diagnosed in 2013 according to ACR criteria (1990). Examination revealed a moderate general condition, preserved orientation in time and space, and absence of pulse in both radial arteries. A systolic bruit was heard over the right carotid artery.Apart from microcytic anemia (Hb 95 g/L), lab tests showed elevated inflammatory markers (ESR 9 mm/hr; serum CRP 0.2 mg/dL). Liver and kidney functions, immunoglobulins, and complement levels were normal. ANA and ANCA were negative. Serologic testing for syphilis was also negative.At admission, the patient was on glucocorticoid therapy with prednisolone 10 mg/day. Carotid ultrasound revealed concentric, hypoechoic thickening of the brachiocephalic vessel walls, causing stenosis on the right and complete occlusion of the left common carotid artery. Proximal subclavian artery occlusion was seen bilaterally; vertebral arteries appeared normal.Two months earlier, MSCT had confirmed bilateral involvement of the carotid and subclavian arteries, as well as the circle of Willis.To assess inflammatory activity, diffusion-weighted MRI was performed. Increased signal intensity was observed in the carotid and subclavian arteries, consistent with inflammation seen on MSCTA.
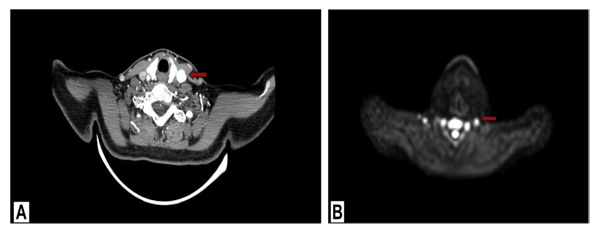 | Figure 1. MSCTA (A) and DW MRI (B) images showing inflammation of the same arterial wall (red arrows) |
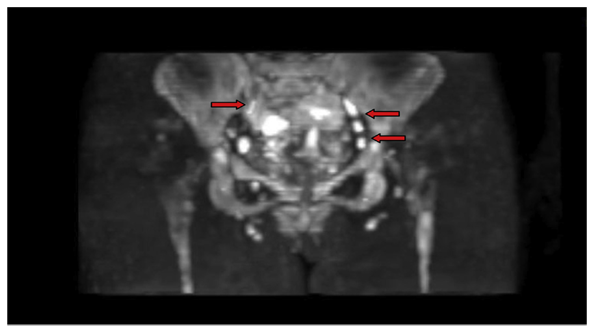 | Figure 2. DW MRI of pelvic area showing high signal from both iliac arteries and enhanced signal from perivascular lymph nodes |
3. Conclusions
- DWIPS MRI visualization and IL-6 inhibitors (particularly tocilizumab) are among the most significant innovations in the diagnosis and treatment of Takayasu arteritis. These methods enable early disease detection, monitoring of treatment efficacy, and control of inflammation. Further clinical studies are needed to better understand and validate these approaches.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML