-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1964-1968
doi:10.5923/j.ajmms.20251506.73
Received: May 28, 2025; Accepted: Jun. 16, 2025; Published: Jun. 21, 2025

Modern Treatment Methods for Mallory-Weiss Syndrome
Sattarov O. T., Ashuraliev Sh. X.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Treatment of bleeding in Mallory-Weiss syndrome (MWS) remains an urgent problem in emergency surgery. According to some authors; MVS accounts for up to 15% or more of the total number of upper gastrointestinal bleedings. In 84% of cases, MVS develops against the background of chronic liver and kidney diseases, chronic alcoholism, gastric and duodenal ulcers, and exacerbation of chronic pancreatitis. Mallory-Weiss syndrome occurs in 10-12% of all cases of gastrointestinal bleeding. This condition is an acute pathology, manifested by severe bleeding from ruptures in the mucous membrane of the lower third of the esophagus and the gastric cardia Our study included 124 patients with Mallory-Weiss syndrome complicated by bleeding. In the Emergency Surgery Department of the Multidisciplinary Clinic of the Tashkent Medical Academy, endoscopic manipulations were used to stop bleeding in all patients from December 2019 to December 2024.
Keywords: Mallory-Weiss syndrome, Emergency surgery, Hemorrhagic syndrome, Endoscopic injection
Cite this paper: Sattarov O. T., Ashuraliev Sh. X., Modern Treatment Methods for Mallory-Weiss Syndrome, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1964-1968. doi: 10.5923/j.ajmms.20251506.73.
1. Introduction
- Mallory-Weiss syndrome - degenerative damage (rupture) of the mucous membrane of the esophagus and the cardiac parts of the stomach, develops against the background of severe vomiting or other pathogenetic factors. In addition, hiccups and even cough can be the cause of Mallory-Weiss syndrome [4,24,14]. There is also an increase in intra-abdominal pressure during vigorous physical activity. There are enough reasons for this. The issue of origin is determined individually. Prevention and prevention of recurrence of the pathological condition depend on understanding the nature of the phenomenon [21,2,27].This condition is an acute pathology, manifested by severe bleeding from ruptures in the mucous membrane of the lower third of the esophagus and the gastric cardia [15,23,24]. As a result of studies by world scientists, it became known that the mortality rate in patients with Mallory-Weiss syndrome is 3.8% in the UK, 9.7% in Japan, 1.3% in the USA, and 2.5% in India [7,12,18].In this regard, surgical control of bleeding is accompanied by severe postoperative complications in the form of hepatorenal failure, alcoholic psychosis, and high mortality, ranging from 15 to 30%. In recent years, there has been a trend towards the treatment of this disease using endoscopic methods to stop bleeding [11,22,23].However, existing methods of endoscopic hemostasis do not completely guarantee against recurrent bleeding, the frequency of which ranges from 5.6 to 30.6%.Modern diagnosis of acute gastrointestinal bleeding in Mallory -Weiss syndrome presents significant challenges, as the disease is characterized by a lack of characteristic clinical signs [9,27]. To date, there is no single treatment strategy.All of the above indicates the great scientific and practical importance of this problem, which requires in-depth, comprehensive scientific research and the development of optimal treatment methods.Despite the many achievements in the treatment of Mallory-Weiss syndrome in modern medicine, many unresolved problems remain. The issues of early detection of this pathology, the development of more effective methods of treatment and their introduction into surgical practice remain relevant. To date, a special classification of Mallory-Weiss syndrome according to the degree of damage and a treatment algorithm based on this classification have not been developed [5,13,30].Mallory-Weiss syndrome occurs in 10-12% of all cases of gastrointestinal bleeding. This condition is an acute pathology, manifested by severe bleeding from ruptures in the mucous membrane of the lower third of the esophagus and the gastric cardia [1,16]. The severity of the hemorrhagic syndrome depends on the damage to the vessels of different diameters of the mucous membrane, as well as the vessels of the muscular and subserous layers of the esophagus and stomach, and the depth of the rupture of the walls of these organs [8,17,20].The leading factor in the pathogenesis of this syndrome is an increase in intraesophageal pressure, often in the lower third of the esophagus and at the esophageal-gastric junction, with a simultaneous increase in abdominal pressure. The main etiological factors are vomiting, hiccups, regurgitation. Rarely, but still, mucosal tears associated with endoscopic examination occur.Currently, drug therapy is considered the main treatment for Mallory-Weiss syndrome. However, in some cases, for example, when a bleeding episode recurs or when drug treatment is ineffective, endoscopic surgery is used. In cases where the bleeding intensity is high and it is not possible to stop the bleeding using endoscopic methods, patients are urgently treated with open surgery [6,26]. In a study conducted in Japan, 66 (78.5%) of the 84 patients (18 women, 66 men, mean age 43.8) who were taken for observation were successfully treated with drug treatment. Rebleeding was observed in 4 patients (4.76%). Endoscopic injection was performed in 12 patients (14.3%). Open surgery was performed in 1 patient (1.19%). Death occurred in 1 patient (1.19%) [19,24].Research goal: To improve treatment outcomes based on modern integrated approaches to the diagnosis and treatment of Mallory-Weiss syndrome.
2. Research Object
- Our study included 124 patients with Mallory-Weiss syndrome complicated by bleeding. In the Emergency Surgery Department of the Multidisciplinary Clinic of the Tashkent Medical Academy, endoscopic manipulations were used to stop bleeding in all patients from December 2019 to December 2024.All patients were divided into two groups: The main group included 64 patients who underwent a new method of endoscopic hemostasis in 2019-2024. The control group included 60 patients who underwent traditional endoscopic intervention to stop bleeding in Mallory-Weiss syndrome in 2019-2024. For comparison, a significant predominance of male patients was observed in both the main and comparison groups: 54 (84. 4 %) men and 10 (15.7%) women in the main group, respectively. In the control group, 52 (86.6%) men and 8 (13.4%) women.In the control group, patients with Mallory-Weiss disease complicated by bleeding had Forrest grade 1A in 5 (8.3%) patients, all of whom were male. Grade 1B bleeding was observed in 8 (13.3%) patients, including 7 (11.6%) men and 1 (1.66%) women, grade 2A bleeding was observed in 20 (33.3%) patients, including 17 (28.3%) men and 3 women, grade 2B bleeding was observed in 23 (38.3%) patients, including 20 (33.3%) men and 3 (5%) women, grade 2C bleeding was observed in 4 (6.66%) patients, including 3 (5%) men and 1 (1.66%) women, and grade 3 bleeding was not detected in any of the patients in the control group.In the control group of 5 patients with Mallory-Weiss syndrome complicated by bleeding, grade 1A bleeding was detected, and in 2 of the 5 patients (40%) a Blackmore probe was inserted for 24 hours. After 24 hours, the Blackmore probe was removed and the patient had rebleeding. In patients complicated by bleeding and in whom a Blackmore probe was inserted again, the cause of rebleeding was considered to be the large size of the fissures. During diagnostic endoscopy, it was determined that the size of the Mallory-Weiss fissure in patient 1 was 2.5x1 cm, and in patient 2, the size of the fissure was 2x1 cm. As a result, the patients were reinserted with a Blackmore probe for another 24 hours. After 24 hours, the Blackmore probe was removed again in the patients, and diagnostic endoscopy was performed on the patients. In the control patients, infiltrative changes were found in all areas of the esophagus in the inner mucosa of the esophagus and around the Mallory-Weiss fissure due to the long-term installation of the Blackmore probe. The mucous membranes are infiltrated and hyperemic. No signs of active bleeding are detected. Taking into account the changes in the esophageal mucosa, the patient underwent endoscopic injection of 33% alcohol around the Mallory-Weiss fissure.
3. Results
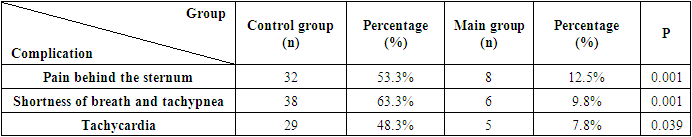
- As a result of our scientific research We have developed a modern, improved classification of Mallory-Weiss syndrome.Improved classification created in Mallory-Weiss syndromeI. According to the location of the injury- EF type (esophageal fissure) - lower third of the esophagus.- CEF type (cardioesophageal fissure) – cardioesophageal junction.- KESF type (cardioesophageal-gastric hernia) – with the transition of the lesion from the cardioesophageal junction to the gastric mucosa.- HF type (herniated hernia) – ruptures in the area of the hiatal hernia.II. By the number of cracks:- One- SeveralIII. By length of cracks:- Small - up to 1.0 cm- Average - 1.0 to 2.0 cm- Large - more than 2.0 cmIV. By depth of cracks:Stage 1 - mucosal rupture.Stage 2 - rupture of the mucosa and submucosa.Stage 3 - rupture involving the circular muscle layer.Stage 4 - rupture of all layers of the esophagus.V. According to the intensity of bleeding:Grade 1 - ongoing bleeding1a - reactive, massive arterial bleeding, the source of bleeding is not visible due to the impossibility of sanitizing the esophagus from blood.1b - reactive, arterial bleeding, allows for the possibility of esophageal resection and identification of the source of bleeding.1c - venous bleeding, no blood clots.1d - the crack is covered with fresh blood clots, blood flow is detected from under them.Grade 2 – stopped bleeding:2 a - Thrombosed vessel visible in the area of the rupture.2 b - fixed thrombus in the rupture area without bleeding.2 c - the rupture area is covered with fibrin.3 - Rupture without signs of bleeding, granulation of the crack.Also, the lack of a clear treatment algorithm for patients with Mallory-Weiss syndrome so far creates many difficulties in early diagnosis of the disease and conducting treatment procedures. This, in turn, remains a major factor in the quality of medical care received by patients and the extension of the duration of their hospitalization, as well as the rehabilitation period in the post-disease period. As a result of our scientific research, we have created a new treatment algorithm based on the above modern improved classification. The medical significance of the treatment algorithm is that after the disease is diagnosed based on the classification we have proposed, the type of treatment is selected based on this diagnosis, depending on the degree of the disease, based on the algorithm.Also, a new improved special probe was developed based on the above new classification for Mallory-Weiss syndrome. Until now, the Blackmore probe has been used for patients with Mallory-Weiss syndrome complicated by bleeding. This, in turn, has led to the following unpleasant sensations and complications in patients: shortness of breath, pain in the epigastric region, tachycardia, increased respiratory rate, as well as hyperemia and infiltration of the esophageal mucosa, etc.A distinctive feature of the special probe developed as a result of our scientific work is the low incidence of the above-mentioned unpleasant sensations and complications.The special probe we developed is made of silicone, 18 Fr size, consists of 2 balloons, 88mm long, inner diameter - 6mm, outer diameter - 10mm. The balloons and the probe cavity open to the outside through separate channels that are not connected to each other. The function of this probe is to prevent the mechanical impact of the esophageal balloon part of the Blackmore probe on the esophageal mucosa and the complications that arise from it.1st balloon - a gastric balloon that ensures fixation of the probe in the stomach when inserted.2- Balloon - inflates in the lower part of the esophagus and exerts a compression effect to stop bleeding in Mallory-Weiss fissures complicated by bleeding.Balloon 1 is located 1 cm from balloon 2.
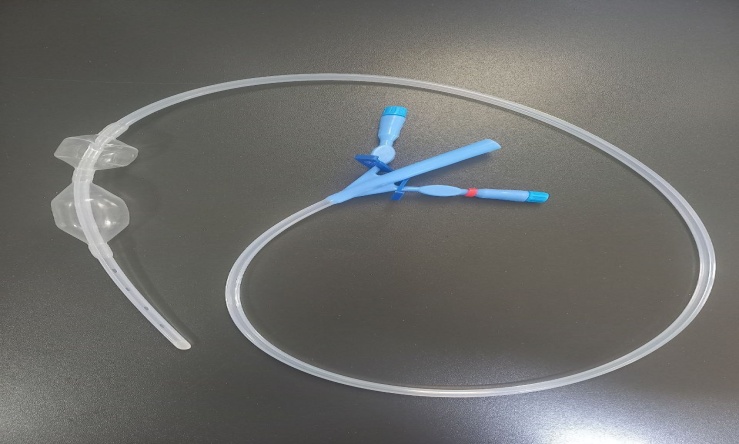 | Figure 1. A special probe used in Mallory-Weiss syndrome |
|
4. Conclusions
- 1. The analysis showed that in the control group, after the procedures performed using traditional methods, the pain behind the sternum increased significantly by 53.3%, shortness of breath and tachypnea increased by 63.3%. Infiltration and hyperemia of the mucous membranes after the probe increased by 16.6%. This is due to the use of the Blackmore probe in Mallory-Weiss syndrome. This, in turn, requires the abandonment of the Blackmore probe in Mallory-Weiss syndrome and the development of a probe that is suitable for this disease and causes less harm.2. The Forrest classification used in the control group is actually used in diseases complicated by gastrointestinal bleeding. Until now, the use of this classification in Mallory-Weiss syndrome and the subsequent treatment of this disease have had a negative impact on the correct treatment tactics and the reduction of the rehabilitation period of patients in the post-disease period. This, in turn, requires the development of a special and disease-specific classification for Mallory-Weiss syndrome.3. The diversity of treatment tactics in patients with Mallory-Weiss syndrome and the lack of a perfect treatment algorithm have so far caused several confusions in early detection of the disease, correct diagnosis, and correct choice of treatment tactics. This, in turn, requires the creation of a suitable treatment algorithm for Mallory-Weiss syndrome.4. In patients with Mallory-Weiss syndrome, the use of a special probe created based on our scientific work, the diagnosis of patients based on the newly created classification, and the treatment based on the algorithm created based on this classification are of great importance in reducing the complications of the disease in patients. This plays an important role in reducing the incidence of rebleeding, pulmonary congestion, chest pain, and mortality in patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML