Khodjimatov Gulomidin Minkhodzhievich1, Yigitov Ayubkhon Azizbekovich2, Yahyoev Sardorbek Mamasobir ugli3
1D.M.Sc., Professor, Andijan State Medical Institute, Andijan, Uzbekistan
2Doctoral Candidate, Andijan State Medical Institute, Andijan, Uzbekistan
3PhD, Assistant, Andijan State Medical Institute, Andijan, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
With the development of laparoscopic surgery, combined simultaneous operations for diseases of different organs have become more popular and are widely used in modern surgery. The object of the study was 276 patients with cholelithiasis combined with other surgical diseases of the abdominal organs, who underwent surgical correction of the identified pathologies. Simultaneous laparoscopic operations are the optimal method for combined diseases of the abdominal organs, offering economic, cosmetic and aesthetic advantages, reducing the hospital days, drug costs, complications and postoperative mortality.
Keywords:
Cholelithiasis, Concomitant surgical pathology, Endovideosurgical technology, Simultaneous operations
Cite this paper: Khodjimatov Gulomidin Minkhodzhievich, Yigitov Ayubkhon Azizbekovich, Yahyoev Sardorbek Mamasobir ugli, The Outcomes of Treatment of Combined Surgical Diseases of Abdominal Organs Using Simultaneous Laparoscopic Surgeries, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1933-1937. doi: 10.5923/j.ajmms.20251506.65.
1. Introduction
Simultaneous Operations (SO) are the concurrent performance of two or more independent operations for different diseases that require surgical treatment. The main stage is a simultaneous operation performed for the patient's primary disease, and the primary disease is the condition with which the patient was admitted to the hospital and which poses the greatest threat to their life during the surgical treatment stage [1-5]. The simultaneous stage is the stage of operations performed for a combined disease, and a combined disease is a condition that poses a lesser threat to the patient's life during surgical treatment compared to the primary disease, and its treatment depends on the surgeons' choice, patient condition, and concomitant disease [6-7].Many domestic and foreign surgeons recommend performing simultaneous operations, considering the following advantages over multi-stage treatment: simultaneous treatment of 2-3 different surgical diseases; prevention of disease progression when surgical treatment was postponed; reducing the total time of patient hospitalization and subsequent treatment; eliminating the risk of repeated anesthesia and its complications; eliminating the need for repeated examination and preoperative preparation; increasing the economic efficiency of treatment [8-11].Despite the obvious advantages of simultaneous operations and a large number of clinical observations, such surgical interventions are performed in an average of 3-5% of surgical patients, whereas the frequency of combined pathology, according to WHO, reaches 20-30% [12-14].In recent publications, reports have begun to appear about simultaneous operations (SO) that are being performed using video laparoscopic techniques. Performing combined laparoscopic interventions does not require expanding access, slightly increases the duration of the operation, and saves the patient from the risk of repeated interventions and anesthesias [15]. Laparoscopic cholecystectomy (LCE) currently occupies the leading place in the total number of operations performed laparoscopically, therefore, SO are most often performed for cholelithiasis [16-18].The work was carried out in accordance with the comprehensive research work of the Department of Surgical Diseases of the Faculty of Advanced Training and Retraining of Doctors at Andijan State Medical Institute "Development of surgical interventions in the treatment of patients with cholelithiasis, gastric ulcer, and duodenal ulcer", state registration No. 0100U005308.Issues dedicated to the comprehensive use of video laparoscopic techniques in surgical correction of combined pathology of abdominal organs are poorly covered in the literature. The issues of indications and contraindications for performing SLO, the scope of preoperative and intraoperative examination, the timing of the operation, the features of anesthesiological care, technical principles, and organizational issues of treating combined pathologies of abdominal organs - whether to operate traditionally or using video laparoscopic technologies - have not been definitively resolved.The aim of the work: to evaluate the effectiveness of simultaneous endovideosurgical operations in patients with combined diseases of abdominal organs.
2. Material and Methods of Research
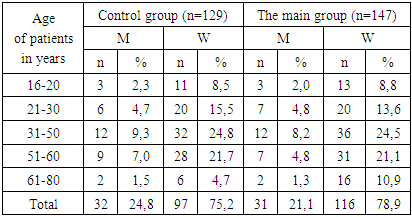
The object of the study was 276 patients with cholelithiasis (CLD) in combination with other abdominal organ diseases, who underwent surgical correction of combined pathology. Among patients who underwent SOV, there were 213 women (77.2%), and 63 men (22.8%). The age of patients ranged from 16 to 80 years (Table 1).Table 1. Distribution of patients by age and gender (n= 276)
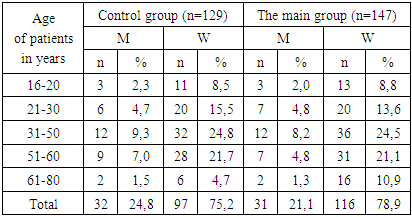 |
| |
|
All patients were divided into two groups: the first control group included 129 patients who underwent simultaneous operations using the traditional open method (from 2015 to 2020). The second study group included 147 patients who underwent laparoscopic simultaneous operations for combined surgical diseases of the abdominal organs (from 2020 to 2025).Patients in the main and control groups were comparable in age, nature and severity of concomitant pathology, and nature and duration of the main disease. All patients who underwent simultaneous operations had histological confirmation.Patient examination was conducted in compliance with accepted standards, taking into account both combined and main concomitant diseases. All patients underwent medical history collection, physical examination, laboratory and instrumental studies, radiation diagnostics, and consultations with specialized specialists.The study used statistical methods of descriptive statistics, correlation analysis, and determination of the reliability of differences between compared values based on the Student's t-test calculation. The difference was considered reliable at p<0.05.All simultaneous abdominal operations performed using the traditional method were carried out in modern operating rooms equipped with all necessary equipment under endotracheal anesthesia with muscle relaxants.Endovideosurgical operative interventions were performed in special video endosurgical operating rooms using Karl Storz (Germany) stands, under intravenous anesthesia with artificial lung ventilation.All patients were operated on in surgical departments of clinics at Andijan State Medical Institute and in the endosurgical department of the Andijan branch of the Republican Scientific Center for Emergency Medical Care, during the period from 2015 to 2025.I. Simultaneous Operations Performed Using the Traditional MethodIn the control group of 129 patients, combined abdominal organ pathology was diagnosed preoperatively in 85 (65.9%) cases. Incomplete preoperative examination, for various reasons, led to the fact that in the remaining 44 (34.1%) cases, the combined disease was identified during intraoperative revision of the abdominal organs.In the first group, 129 patients underwent the following simultaneous operations using the traditional open method:1. In 35 (27.1%) patients with duodenal ulcer disease, cholecystectomy was performed as the main stage of the operation, followed by stomach resection.2. In 34 (26.4%) patients, cholecystectomy was performed first, followed by liver echinococcectomy.3. In patients with ventral hernias (25-19.4% of patients), abdominal wall plasty was performed after cholecystectomy.4. In 20 (15.5%) patients, cholecystectomy was performed first, followed by inguinal canal plasty.5. Removal of a solitary liver cyst after cholecystectomy was performed in 15 (11.6%) patients.All simultaneous operations were performed through a wide median incision, which provided free access to organs on any floor of the abdominal cavity for their full revision and created the most favorable conditions for performing combined surgery.II. Simultaneous operations performed laparoscopicallySurgical intervention was performed in an endovideosurgical operating room using racks manufactured by Karl-Storz (Germany), under general anesthesia with artificial ventilation.In the study group of 147 patients, 54 (36.7%) had chronic calculous cholecystitis (CCH) combined with morbid obesity on the background of diabetes mellitus. In 32 (21.8%) patients, HCG was combined with liver echinococcosis, in 24 (16.3%) patients with anterior abdominal hernia, in 23 (15.7%) inguinal hernias, and in 14 (9.5%) solitary liver cyst (Рисунок 2.)Laparoscopic cholecystectomy (LCE) was performed in all patients at the first stage, followed by simultaneous surgery. Patients with LHE were performed according to a generally accepted method (Puchkov K.V. 2005). The LHE time did not exceed 20±10 minutes.During the operation, we used one monitor for all 54 morbid obese patients, which is located behind the patient's right shoulder so as to provide a convenient overview for all team members. As a rule, 5-port access was used. Access to the abdominal cavity is obtained by installing, under visual control, an operating laparoscope with an optical axis angle of 0° of an optical 12-13 mm trocar along the left mid-clavicular line in the middle between the navel and the costal arch. After applying carboxyperitoneum, 12-14 mmHg. under the visual control of an operating laparoscope with an optical axis angle of 30, other trocars were installed — a 12 mm (13 mm when using a reusable trocar) trocar along the right mid-clavicular line at the same level as the left trocar and a 10 mm trocar in which a laparoscope will be installed during the entire operation and which is inserted supraumbilically; the distance from the navel depends on It depends on the patient's height and constitution and is determined after a visual assessment of the abdominal cavity. A trocar for the liver retractor was installed subxyphoidally; The 5 mm trocar for the assistant clamp is installed in the left hypochondrium slightly higher than the 12 mm trocar.Stages of the operation: 1) Laparoscopic cholecystectomy was performed according to the generally accepted method (Puchkov K.V. 2005). The LHE time did not exceed 20±10 minutes. 2) then, longitudinal resection of the stomach was performed as follows: mobilization of the gastro-diaphragmatic ligament, the Lymer—Bertelli membrane; 3) access to the omentum; 4) mobilization of the stomach along a large curvature; 5) laying of the calibration probe; 6) resection of the stomach; 7) strengthening of the stapler line; 8) removal of the calibration probe; 9) checking for tightness of the stapler line; 10) removal of the resected stomach; 11) drainage of the abdominal cavity (according to indications).The following tools are used during the operation: a disposable 60 mm stapler and cassettes for it; the tip of an ultrasonic dissector; the tip of a brewing tool and 2 disposable 12 mm trocar.Indications for laparoscopic echinococcectomy from the liver were: single cysts of medium size 10-15 cm in diameter localized in the III, IV, V segments of the liver, exclusively of type CL; C; CE-1 or CE-3; partial surface location of the cyst, according to the classification of ultrasound images of echinococcal cysts according to H.A.Gharbi (1981) [7] as modified by WHO (2003) [8].Thoracoports were installed during laparoscopic echinococcectomy from the liver in 32 patients, as in LHE according to a generally accepted technique, however, in the right subcostal region, a 20mm thoracoport is installed in place of 5mm. After delineating the echinococcal cyst with a gauze swab soaked in 76-80% alcohol, the echinococcal cyst was punctured with aspiration of the contents. 76% alcohol was injected into the cavity through this needle, and then washed with a hot solution of furacillin (78-80°C) at an exposure of 5-8 minutes. Then the fibrous capsule was dissected, the chitinous membrane was removed and removed from the abdominal cavity in a special container. The residual cavity was treated with 76% alcohol, then with a warm solution of furacillin (78-80°C). In 21 patients, the residual cavity was then tamponed with a large omentum. In 11 (7.5%) patients, due to the inability to tampon the residual cavity with an omentum, a "mini" laparotomy access was used in the projection of the residual cavity. To perform echinococcectomy from a mini laparotomy, diagnostic laparoscopy established the exact location of the cyst and the place on the anterior abdominal wall where a mini laparotomy incision was planned. The length of the skin incision varied about 5 cm. Small-sized mechanical wound expanders were used. The raised roller under the patient's back brought the liver closer to the wound, and the bright illumination of the abdominal cavity with a laparoscope is an undoubted advantage of the operation. Stages of operations: cyst puncture with evacuation of the contents of the echinococcal fluid, then opening and removal of the chitinous membrane. Treatment of the residual fibrous membrane cavity with glycyrine with an exposure of 10 minutes, treatment with a hot solution of furacillin and then 80 C0 alcohol. Excision of the fibrous capsule protruding above the liver parenchyma. Through a "mini" laparotomy access, the residual cavity was eliminated using the Delbe method. The operation was completed by draining the subhepatic area with a silicone tube through a 20 mm thoracoport installed in the right hypochondrium.In 14 (9.5%) patients who were diagnosed with HCG concomitant soletary cyst of the liver, which was located mainly superficially in the III, IV, V and VI segments of the liver. Laparoscopic cholecystectomy was performed according to a generally accepted procedure (Puchkov K.V. 2005). The LHE time did not exceed 20±10 minutes. Then, laparoscopic resection of a solitary liver cyst was performed in the second stage. First, the cyst was punctured and the contents were aspirated, and the cyst cavity was rinsed with a warm furacilin solution through a puncture needle. Then the capsule was precisely removed, and if it was impossible, 2/3 of the brush wall was excised.In 24 (16.3%) patients with ventral hernia, after performing LCE according to a generally accepted technique, plastic surgery of the anterior abdominal wall was performed in 14 cases and in 10 cases using propylene mesh. In 23 (15.6%) patients with inguinal hernias, inguinal ring plastic surgery was performed using propylene mesh and 4 composite mesh.
3. The Results of the Study
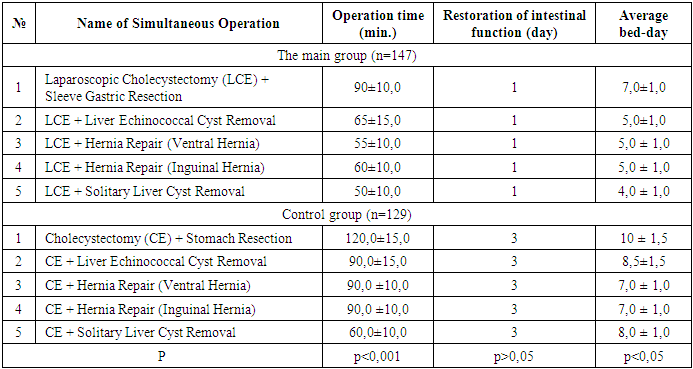
In patients of the control group who underwent simultaneous operations in the traditional way, the average duration of surgery was HE + Gastric resection was 120.0±15.0minutes; HE + Removal of an echinococcal cyst of the liver 90.0± 15.0 minutes; HE + herniation (ventral hernia) 90.0 ± 10.0 minutes and HE + herniation (inguinal hernia) 90.0 ± 10.0 minutes; HE + removal of solitary cyst of the liver 60.0±10.0 min.In the control group, complications occurred in 20 (15.5%) patients. Of these, 2 (1.6%) patients had duodenal stump failure after Balfour gastric resection, 8 (6.2%) patients had cystic duct stump failure and limited biliary peritonitis. Early adhesive intestinal obstruction in 3 (2.3%) patients. Suppuration of the residual cavity with the formation of a liver abscess after echinococcectomy was observed in 2 (1.6%) patients. Postoperative wound suppuration in 5 (3.9%) and 6 (4.7%) patients developed congestive pneumonia. Fatal outcome in 3 (2.3%) patients.In the control group, the average bed per day of the patient's stay in the hospital was: in patients who underwent HE + Gastric resection 10 ± 1.5 days; HE + Removal of echinococcal cyst of the liver 8.5 ± 1.5 days; HE + herniation (ventral hernia) – 7.0 ± 1.0 days; HE + herniation (inguinal hernia) – 7.0 ± 1.0 days, HE + removal of solitary cyst of the liver 8.0 ± 1.0 days. Out of all 147 (100.0%) patients in the main group, 104 (70.7%) patients underwent surgery as planned. The diagnosis of CCH with combined pathology was established during examination in the preoperative period, and in 43 (29.3%) patients, concomitant pathology was an operational finding. The indication for emergency CP was acute pain in the right hypochondrium, with signs of obstructive calculous cholecystitis.The duration of CP in patients of the main group were: the average duration of LHE + Sleeve-Gastric resection 90±10.0 min.; LHE + Removal of echinococcal cyst of the liver 65 ± 15.0 min.; LHE + herniation (ventral hernia) 55 ± 10.0 min. and LHE + herniation (inguinal hernia) 60 ± 10.0 min.; LHE + removal of solitary liver cysts 50.0±10.0 min.All 147 operated patients did not need narcotic analgesics in the postoperative period, they became more active by the end of the day, and felt satisfactory.Of the 54 patients with morbid obesity, 1 (0.7%) patient developed partial failure of the staple sutures in the cardiac part of the gastric tube on day 5, which healed independently on day 10 after conservative therapy. 2 (1.4%) patients developed congestive pneumonia in the postoperative period. In 1 (0.7%) patient, suppuration of the postoperative wound was complicated. In 118 (80.3%) patients, drainage tubes were removed 2-3 days after control abdominal ultrasound. In 29 (19.7%) patients who underwent emergency simultaneous laparoscopic cholecystectomy (SLC) + liver echinococcal cyst removal, bile discharge from the drainage tube was observed at 120-160 ml per day, which spontaneously stopped 11-21 days after the operation.On control abdominal ultrasound of these patients, due to the absence of residual cavity, drainage tubes were removed 8-29 days after the operation.In all operated patients, bowel peristalsis restoration and gas passage occurred 2-3 days after the operation.Average hospital bed-day stay was:• Patients who underwent SLC + Sleeve Gastric Resection: 7.0 ± 1.0 days• SLC + Liver Echinococcal Cyst Removal: 5.0 ± 1.0 days• LCE + Hernia Repair (Ventral Hernia): 5.0 ± 1.0 days• LCE + Hernia Repair (Inguinal Hernia): 5.0 ± 1.0 days• LCE + Solitary Liver Cyst Removal: 4.0 ± 1.0 daysIn the postoperative period, activation of all patients was achieved by the end of the first day, and they did not require narcotic analgesics.Patients' condition was not severe in the postoperative period, and we did not observe any fatal outcomes (Table 2).Table 2. Results of Simultaneous Operations
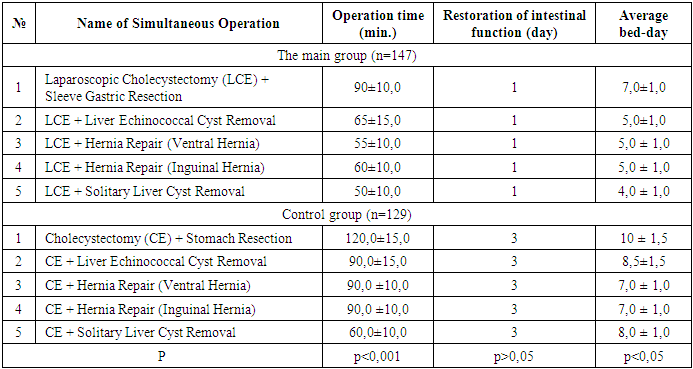 |
| |
|
Due to the impossibility of laparoscopic correction of concomitant surgical diseases of the abdominal organs, 13 (8.8%) patients were combined with a "mini" laparotomy approach.The combined technique using a "mini" access operation is promising, which significantly reduces the duration of the operation, thereby making the postoperative period more favorable for patients.Thus, laparoscopic simultaneous operations for correcting combined surgical diseases of the abdominal organs and anterior abdominal wall are the most optimal and justified intervention, which eliminates combined surgical pathologies during a single anesthesia, reduces the patient's hospital stay and rehabilitation period. After simultaneous laparoscopic operations, patients feel quite satisfactory.
4. Conclusions
1. Ensuring simultaneous operations is possible only in highly qualified multidisciplinary institutions equipped with modern equipment and specialists.2. Simultaneous laparoscopic operations for correcting combined surgical diseases of the abdominal organs and anterior abdominal wall are the most optimal and justified intervention, which eliminates combined surgical pathologies during a single anesthesia, reduces the patient's hospital stay and rehabilitation period.3. To eliminate the residual cavity after laparoscopic liver echinococcectomy, it is necessary to use tamponade with a large omentum; in case of technical impossibility of performing this manipulation, use the Delbet method from mini-laparotomy.4. The advantages of simultaneous laparoscopic operations undoubtedly include an economic effect due to reduced bed-days and reduced medication expenses. The cosmetic and aesthetic effect of the operation for patients plays a significant role.5. The introduction of simultaneous laparoscopic operations for surgical diseases of the abdominal organs into wide clinical practice allows achieving a sharp reduction in complications and postoperative mortality.
References
| [1] | Mishalov V.G. et al. Simultaneous laparoscopic interventions on abdominal organs in obese patients with correction of anterior abdominal wall ptosis // Surgery of Ukraine. – 2017. – No. 1. – P. 30-34. |
| [2] | Artykov K.P., Rakhmatullaev R.R., Rakhmatullaev A.R. Simultaneous operations for combined surgical diseases of abdominal organs // Avicenna Bulletin. – 2015. – No. 2 (63). – P. 114-118. |
| [3] | Rakhmatullaev A.R., Khasanov S.M. Possibilities and feasibility of performing simultaneous laparoscopic operations for combined surgical diseases of abdominal organs // Eurasian Union of Scientists. – 2015. – No. 10-1 (19). – P. 113-116. |
| [4] | Ibragimov Sh.U. Results of surgical treatment of patients with abdominal hernias and combined abdominal pathology // Problems of Science. – 2022. – No. 4 (73). – P. 69-73. |
| [5] | Golbrah V.A. et al. Modern approaches to simultaneous operations (indications, execution algorithms, complications) // Journal of Volgograd State Medical University. – 2021. – Vol. 18. – No. 2. – P. 28-36. |
| [6] | Galimov O.V., Khanov V.O., Aminova A.N., Ziganshin D.M. Simultaneous laparoscopic operations on pelvic organs // Endoscopic Surgery. - 2010. - No. 5. - P. 51-56. |
| [7] | Hayakawa S. et al. Simultaneous transabdominal preperitoneal hernia repair and laparoscopic cholecystectomy: A report of 17 cases // Asian Journal of Endoscopic Surgery. – 2019. – Vol. 12. – No. 4. – P. 396-400. |
| [8] | Hart S. Laparoendoscopic single-site combined cholecystectomy and hysterectomy / S. Hart, S. Ross, A. Rosemurgy // J. Minim. Invasive Gynecol. — 2010. — Vol. 17, No. 6. - P. 798-801. |
| [9] | Murodov A.I., Aliev Z.O., Ermakov N.A. Application of "fast track surgery" program in simultaneous laparoscopic operations // Healthcare of Tajikistan. – 2017. – No. 3. – P. 51-55. |
| [10] | Orr N.T., Davenport D.L., Roth J.S. Outcomes of simultaneous laparoscopic cholecystectomy and ventral hernia repair compared to that of laparoscopic cholecystectomy alone // Surgical Endoscopy. – 2013. – Vol. 27. – P. 67-73. |
| [11] | Rakhmatullaev A.R., Khasanov S.M. Possibilities and feasibility of performing simultaneous laparoscopic operations for combined surgical diseases of abdominal organs // Eurasian Union of Scientists. – 2015. – No. 10-1 (19). – P. 113-116. |
| [12] | Toktorov S. et al. Analysis of simultaneous and isolated laparoscopic operations in cholelithiasis // Bulletin of Science and Practice. – 2022. – Vol. 8. – No. 7. – P. 330-335. |
| [13] | Fedorov A.V., Kriger A.G., Kolygin A.V., Kochatkov A.V. Simultaneous operations. Terminology (literature review and own proposal) // Surgery. - 2011. - No. 7. - P. 72-76. |
| [14] | Ismailov U.S. et al. Simultaneous laparoscopic operations in high-risk patients // Research Journal of Trauma and Disability Studies. – 2023. – Vol. 2. – No. 6. – P. 58-70. |
| [15] | Reiffersceid М. Simultaneous intervention in the abdominal cavity - Surgical Aspects // Zent. Bl. Chir. - 1971. - Vol. 5. - P. 2010. |
| [16] | Surico D. Laparoendoscopic single-site surgery for treatment of concomitant ovarian cystectomy and cholecystectomy / D. Surico, S. Gentilli, A. Vigone // J. Minim. Invasive Gynecol. - 2010. - Vol. 17, No. 5. - P. 656-659. |
| [17] | Quezada N. et al. Simultaneous TAPP inguinal repair and laparoscopic cholecystectomy: results of a case series // Hernia. – 2019. – Vol. 23. – P. 119-123. |
| [18] | Lee J.H. et al. A technique for simultaneous cholecystectomy during bariatric surgery // JSLS: Journal of the Society of Laparoendoscopic Surgeons. – 2015. – Vol. 19. – No. 4. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML