-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1925-1929
doi:10.5923/j.ajmms.20251506.63
Received: May 19, 2025; Accepted: Jun. 15, 2025; Published: Jun. 20, 2025

Optimization of Laparoscopic Cholecystectomy Technique for Acute Calculous Destructive Cholecystitis in the Elderly
Atadjanov Sh. K., Hakimov O. S., Kurbaonov Sh. P., Nosirov M. M., Hamidov F. Sh.
Andijan State Medical Institute, Andijan, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The authors studied the possibility of reducing the number of conversions when performing laparoscopic cholecystectomy in patients of older age groups with acute cholecystitis in complex technical cases. The results of the execution laparoscopic cholecystectomy in 63 patients in a group of 177 patients. The procedure for performing the operation is described. The conclusion is made about the high efficiency of the methods worked in the clinic atypical paroscopic cholecystectomy.
Keywords: Acute Calculous Cholecystitis, Laparoscopic Cholecystectomy, Surgical Tactics, Elderly
Cite this paper: Atadjanov Sh. K., Hakimov O. S., Kurbaonov Sh. P., Nosirov M. M., Hamidov F. Sh., Optimization of Laparoscopic Cholecystectomy Technique for Acute Calculous Destructive Cholecystitis in the Elderly, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1925-1929. doi: 10.5923/j.ajmms.20251506.63.
1. Introduction
- To date, calculus of gallbladder is detected in about 10% of the adult population, more often in women over the age of 40, while the number of complicated forms of calculous cholecystitis remains consistently high [1,2,9,13]. At the same time, the problem of acute calculous cholecystitis (ACC) and its complications significantly increases in elderly and senile patients with a high operational and anesthetic risk due to the presence of severe concomitant metabolic pathology, disorders of the cardiovascular and pulmonary systems.Laparoscopic cholecystectomy (LCE) has now become the method of choice in the treatment of patients with chronic calculous cholecystitis (CCC) [1,2,3,5,10]. The emergence of intraoperative complications and complications in the group of patients with acute cholecystitis, especially in the elderly and senile age, quite often leads to the transition from LCE to laparotomy [1,2,4,7]. Conversion, of course, negates all the advantages of LCE over open surgery. Costs increase significantly, the results of the treatment process deteriorate [6,12,14].Thus, to date, clinical trials, performing laparoscopic surgical interventions in elderly and senile patients with acute cholecystitis, can provide good results with a minimum risk of complications and deaths in the postoperative period and improve patient survival.Aim of the study: development of a technique for laparoscopic cholecystectomy for acute destructive cholecystitis in patients of older age groups.
2. Materials and Methods
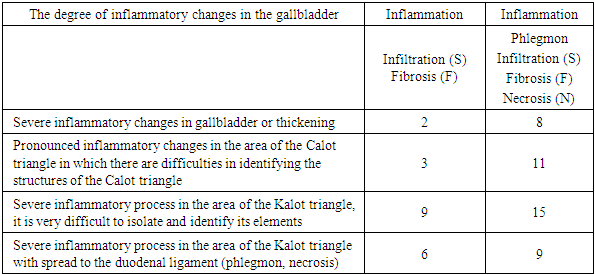
- The paper studied the possibility of reducing the number of conversions during LCE in elderly and senile patients with acute destructive cholecystitis in difficult technical cases. The results of performing LCE in 63 elderly patients with destructive changes from 177 patients are presented. The procedure for performing the operation is described. In laparoscopic operations on the gallbladder, we used an endosurgical complex and sets of operating instruments from Karl Storz (Germany).According to the general status, the severity of concomitant diseases, as well as the risk of surgery and anesthesia, patients were distributed according to the scale proposed by the American Society of Anesthesiologists (ASA). This scale is based on the presence and severity of severe concomitant systemic diseases in patients and implies the allocation of the following 5 classes.Class I - patients without systemic diseases;Class Il - patients with compensated systemic disease that does not significantly limit physical activity;Class Ill - patients with a systemic disease that limits physical or social activity, but can be compensated by treatment;Class IV - patients with decompensated disease requiring constant medication;Class V - patients who may die within 24 hours, regardless of whether or not they receive medical care.In our study, the risk class of ASA anesthesia in patients of all groups varied from Ill to IV. In patients at risk of class Ill anesthesia, concomitant diseases were compensated after preliminary short-term preoperative preparation. In 18 (28.7%) patients, the general condition at admission was assessed as moderate, 5 (7.9%) patients were in serious condition and 2 (3.1%) in extremely severe.The severe and extremely serious condition of the patients was due to the severity of the underlying disease, as well as the severity of concomitant diseases.All patients on admission to the hospital underwent a comprehensive general clinical study. The presence of pathology from the gallbladder and bile ducts was diagnosed according to the clinical picture, laboratory, ultrasound and endoscopic methods. Prediction of the course of the pathological process and the choice of the treatment method were determined by the clinical picture, temperature reaction, indicators of clinical and biochemical studies, and most importantly, depending on the version of ultrasound imaging of the gallbladder.Ultrasonic signs of AC were thickening of the walls of the gallbladder more than 5 mm, heterogeneity and stratification, double wall contour, an increase in the size of the gallbladder, an impacted stone in the mouth of the cystic duct, the nature of the intravesical fluid, the presence of perivesical infiltrate and (or) exudate.We have identified 3 options for ultrasound imaging of the gallbladder in acute destructive calculous cholecystitis:- signs of destruction of the gallbladder wall, the wall thickness exceeds 4 mm, there is its layering. Similar signs were found in all 63 patients (35%).- signs of perivesical changes (infiltrate and exudate) in 19 patients (11%) had the listed signs.- signs of limited local or widespread peritonitis. With ultrasound, free fluid is visualized in the subhepatic space and other parts of the abdominal cavity. Similar changes were diagnosed in 7 patients (4%) (Table 1).
|
|
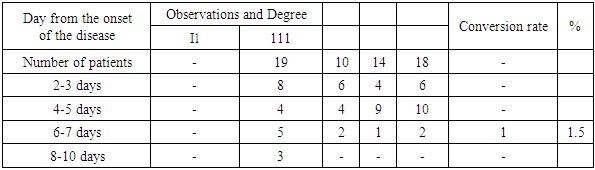
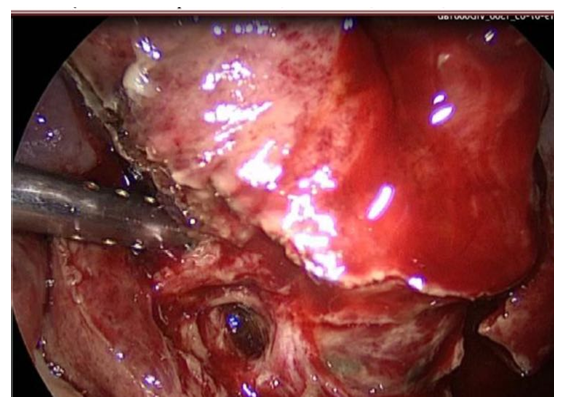
 | Figure 1. Expressed fibrous changes in the wall of the gallbladder are accompanied by changes in the paravesical tissue |
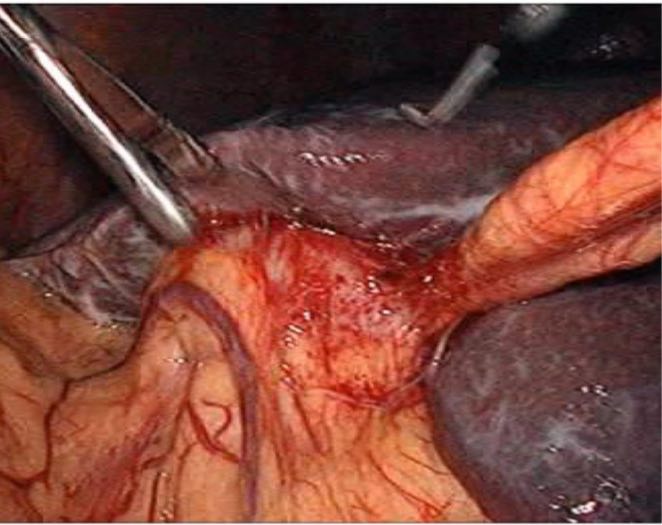
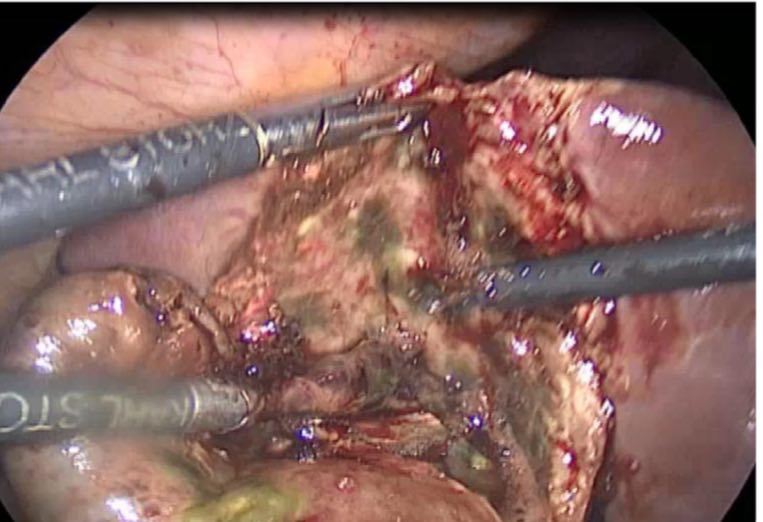
 | Figure 2. Infiltrated gallbladder (puncture and aspiration of the gallbladder) |
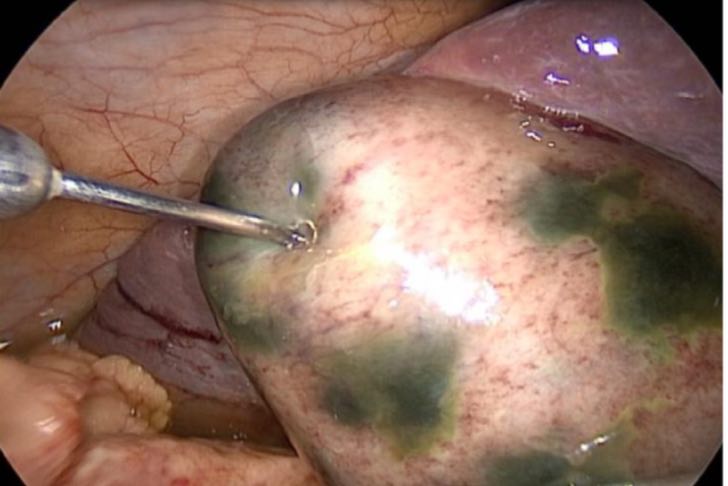
 | Figure 3. Mobilization of the cystic artery |
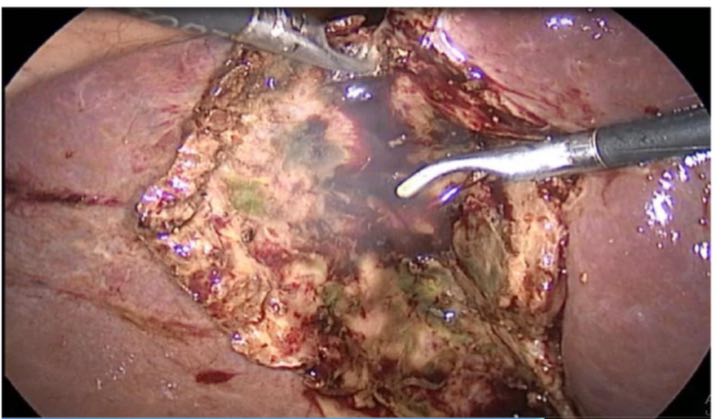
 | Figure 4. Isolation of the gallbladder from the gallbladder bed |
 | Figure 5. Clips with large size or medium clips are placed using the ladder method and intersection |
 | Figure 6. Control of the bleeding gallbladder bed |
3. Results
- After the introduction of the improved LCE technique into clinical practice, since 2015, the conversion rate has decreased to 2%, and since 2000 to the present day it is 0.4%. This was a consequence of the development and further improvement of the techniques of laparoscopic cholecystectomy.The results of the use of LCE remain ambiguous, and above all with regard to ensuring their safety. Differences in the anatomy and topography of the bile ducts, cystic duct and artery do not allow to classify interventions on the gallbladder as "standard". The conditions of the operation are complicated by acute inflammatory and adhesive processes, in which even the "typical" anatomy of the subhepatic space can undergo significant changes. Practically insurmountable difficulties arise when acute cholecystitis is combined with ductal and vascular dystopias.
4. Conclusions
- The developed clear technical methods for performing laparoscopic cholecystectomy (LCE) in destructive forms of acute calculous cholecystitis will allow achieving high positive results while maintaining a stable rate of complications at the level of I -2% and reducing mortality to - 0.1%.One of the advantages of minimally invasive surgery is the ability to stage-by-stage treatment of severe and non-standard cases. The presence in the arsenal of a medical institution of the whole complex of minimally invasive methods of diagnosis and treatment of destructive forms of acute calculous cholecystitis allows to reduce the number of complications and deaths to a minimum. The final choice of the method and methods of treatment for this category of patients depends on the equipment of the given medical institution and the availability of appropriate qualified specialists.The developed and applied tactics for the treatment of destructive forms of gallstone disease showed good results.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML