-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1917-1920
doi:10.5923/j.ajmms.20251506.61
Received: May 20, 2025; Accepted: Jun. 17, 2025; Published: Jun. 20, 2025

The Association of CRP and Vitamin D Deficiency with Cardiovascular Disease: A Study among Prediabetic Patients in Andijan City and Markhamat District of the Republic of Uzbekistan
R. H. Abdurakhmonova
Free Applicant of the Department of Hospital Therapy and Endocrinology, Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: R. H. Abdurakhmonova, Free Applicant of the Department of Hospital Therapy and Endocrinology, Andijan State Medical Institute, Andijan, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

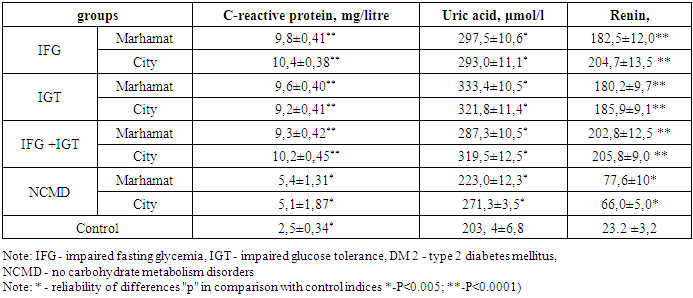
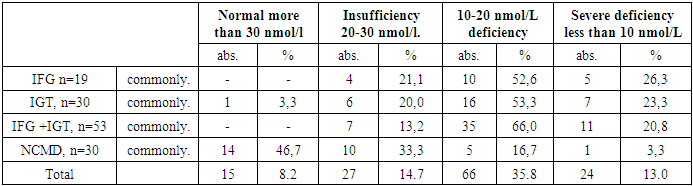
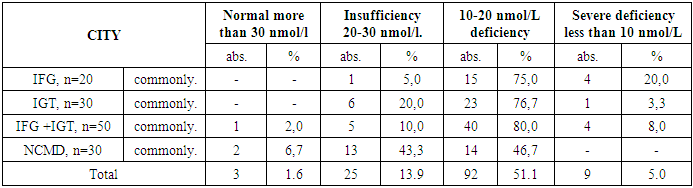
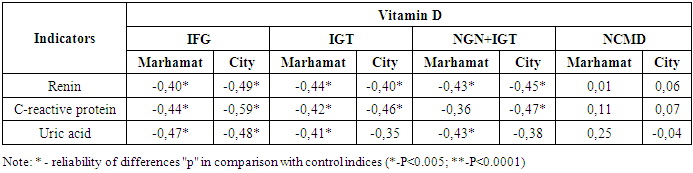
The study aimed to assess the association between C-reactive protein (CRP), vitamin D deficiency, and cardiovascular diseases in patients with prediabetes in Andijan city and Markhamat district, Uzbekistan. A total of 3,400 individuals at risk were examined using the Findrisk questionnaire and laboratory tests. Results showed significantly elevated levels of CRP, uric acid, and plasma renin in prediabetic patients compared to the control group (p<0.005; p<0.0001). An inverse correlation was found between vitamin D levels and CRP, renin, and uric acid, indicating their potential role in cardiovascular risk among prediabetic individuals.
Keywords: Vitamin D, C-reactive protein, Prediabetes
Cite this paper: R. H. Abdurakhmonova, The Association of CRP and Vitamin D Deficiency with Cardiovascular Disease: A Study among Prediabetic Patients in Andijan City and Markhamat District of the Republic of Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1917-1920. doi: 10.5923/j.ajmms.20251506.61.
Article Outline
1. Introduction
- Cardiovascular disease (CVD) is commonly perceived as a major public health problem leading to high morbidity and mortality rates. Extensive and mounting evidence suggests that inflammation is an important part of this chronic condition [1]. Vitamin D is a fat-soluble steroid that has been found to play an important role in the regulation of inflammatory cytokines and immune cells [2]. Novel studies have shown that vitamin D deficiency is associated with increased inflammatory responses and immune system activation, and may have an inverse relationship with various pathological processes such as myocardial infarction [3,4,5].C-reactive protein (CRP), which is a sensitive indicator of inflammation, has been demonstrated as an important element in predicting cardiovascular disease in a number of prospective epidemiological studies. One such study suggested that the inclusion of SRB measurement in screening based on lipid levels could significantly improve the methodology for identifying women at risk of cardiovascular events [6,7,8].Observational studies have demonstrated an association between reduced serum vitamin D levels and an increased risk of cardiovascular disease. At the same time, optimal vitamin D levels seem to have a positive effect on the cardiovascular system, which may be partly explained by its immunomodulatory and anti-inflammatory properties [9,10,11].Randomised controlled trials (RCTs) and information on the relationship between vitamin D intake through food or supplements and cardiovascular disease risk show mixed results: some studies indicate a beneficial effect, while others find no association with cardiovascular disease. There is a possibility that the effect of vitamin D supplementation may vary depending on C-reactive protein (CRP) levels [12].All of the above provided the basis for the present study.The aim of the study was to investigate the association of C-reactive protein and vitamin D deficiency with cardiovascular diseases: a study among patients with prediabetes in Andijan city and Markhamat district of the Republic of Uzbekistan.
2. Material and Methods of Research
- The study was conducted on the basis of Andijan State Medical Institute. In total 3400 persons of risk groups were examined, of which 1800 were residents of Markhamat district of Andijan region and 1600 residents of Andijan city. The control group consisted of 30 healthy people. Inclusion criteria: individuals over 20 years of age who were overweight, dyslipidaemic or hypertensive. Exclusion criteria: type 1 diabetes mellitus, other endocrine diseases, metformin use, severe autoimmune diseases, vasculitis, oncology. According to the design, the study was conducted in two phases.At stage 1, according to the study design, cardiovascular risk factors including waist circumference, body mass index (BMI), blood pressure level, lipid profile, presence of diabetes mellitus and metabolic syndrome, and anamnestic information extracted from relevant medical records were analysed. Patients were questionnaired using the Findrisk scale.At the 2nd stage, freshly collected biological material (venous blood) was collected and then promptly delivered to the laboratory for research.The study methods included general clinical approaches, biochemical testing (measurement of fasting blood glucose levels and two hours after meals, determination of glycated haemoglobin, bilirubin (both direct and indirect), as well as ALT, AST, PTI, coagulogram, C-reactive protein, urea, creatinine and lipid profile), hormonal analyses (insulin and C-peptide levels in the blood as needed) and instrumental methods such as ECG, ultrasound of endocrine glands and internal organs, chest X-ray and other tests. Data were expressed as mean ± SD, n (%) or OR (95% CI), all statistical tests were two-sided, and a P value < 0.05 was considered statistically significant.Multiple logistic regression was used to determine the independent association between 25(OH)D status, with normal 25(OH)D as the reference category, and high and low CRP and CVD levels, respectively, after adjusting for demographic variables including age, sex, physical activity, education level, marital status, family history, chronic kidney disease, alcohol consumption, BMI, hypertension, diabetes mellitus, and hypercholesterolemia.We selected covariates as potential confounders based on previous studies or on their biological plausibility. The following covariates were included in our association analysis: age, sex, body mass index (BMI), marital status, education level, smoking status, alcohol consumption, physical activity, hypertension, diabetes, hypercholesterolaemia, chronic kidney disease (CKD), BMI, and dyslipidaemia.
3. Results of the Study
- Figure 1 shows the material and design of the study.
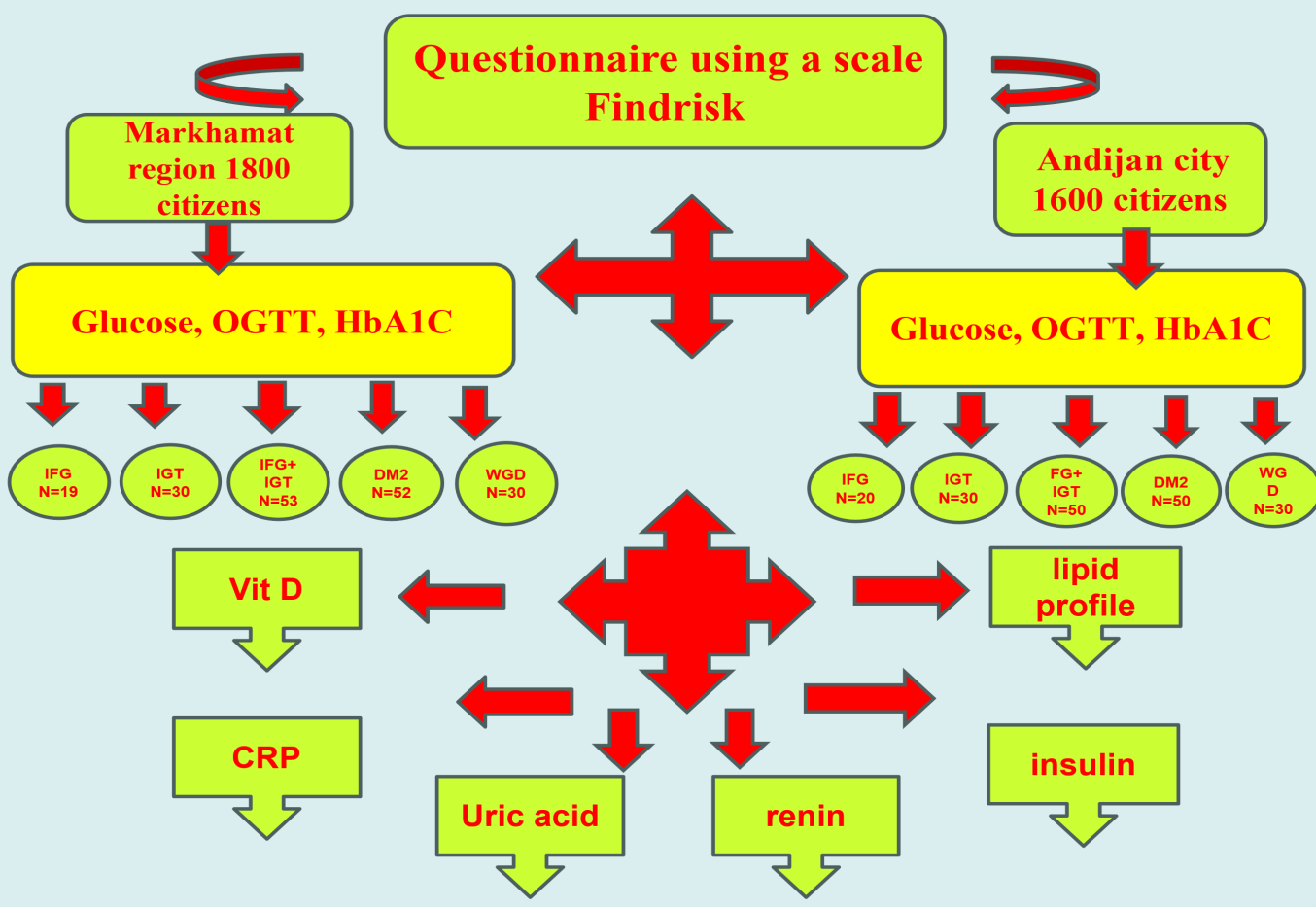 | Figure 1. Material and study design |
|
|
|
|
4. Conclusions
- 1. According to our studies, the mean values of SRB were significantly higher than the control group in all groups and regions (*-P<0.005; **-P<0.0001). 2. A significant inverse correlation between vitamin D, SRB, renin and uric acid content was found in almost all groups of prediabetes patients of both regions (P<0.005).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML