-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1912-1916
doi:10.5923/j.ajmms.20251506.60
Received: May 15, 2025; Accepted: Jun. 12, 2025; Published: Jun. 20, 2025

Clinical and Morphological Analysis of Diffuse and General Peritonitis
B. K. Rakhimov1, H. A. Rasulov2, B. D. Eshonkulova2
1Clinics Hospital named by I. Irgashev, Tashkent, Uzbekistan
2Tashkent Medical Pediatric Institute, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The prominent Austrian surgeon W.Wagner said his famous phrase in 1876: “I and my generation of doctors were brought up in the fear of God and peritonitis.” Despite the fact that almost 150 years have passed, the fear of peritonitis has not passed to this day. After all, peritonitis is one of the most severe complications of acute surgical diseases of the abdominal organs. Mortality in diffuse peritonitis, which causes failure of vital organs, remains high - from 20-30% to 40-50%. That is why the topic of peritonitis does not lose its relevance. This scientific study retrospectively analyzed the clinical data of patients (n=1830) treated in the surgical department of the 4th city hospital in Tashkent named after I. Irgashev during 2023. The purpose of this study was to evaluate the volume and effectiveness of the selected operation, taking into account the clinical picture of peritonitis, its duration and prevalence. At the same time, the studies also took into account the reaction of the morphological structures of the peritoneum depending on the duration of inflammation of the peritoneum and its prevalence.
Keywords: Diffuse peritonitis, Surgical treatment, Mast cells
Cite this paper: B. K. Rakhimov, H. A. Rasulov, B. D. Eshonkulova, Clinical and Morphological Analysis of Diffuse and General Peritonitis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1912-1916. doi: 10.5923/j.ajmms.20251506.60.
1. Introduction
- All the complexity and drama of the peritonitis problem “melt” against the background of the vagueness of the generalizing concept. In general, the diagnosis of peritonitis is understood as inflammation of the peritoneum of any form and degree. In this regard, I. I. Grekov said with bitter irony: it is very easy to “correct” the depressing statistics of peritonitis outcomes: it is enough to “melt” observations of real peritonitis with forms for the treatment of which one operation is enough, performed in a timely and competent manner, and does not require other measures. Experience shows that these traditions exist today. They justify both the optimistic conclusions of some dissertations and the serious concerns of most doctors, which are reflected in some articles in connection with the high mortality rate. According to the summarized data published by B. K. Shurkalin (2000), the average mortality rate is 20-30%, and in the most severe forms of peritonitis it reaches 40-50%. Despite the undeniable achievements of modern medicine, armed with new promising technologies, peritonitis remains a surgical, general clinical, general pathological problem. Therefore, studies on the frequency of occurrence in patients with acute peritonitis, the choice of tactics and methods of treatment, indications for surgery, its type, volume and description, as well as observation of morphological processes occurring in the peritoneum in this pathology, are of great relevance [2,3,4,10,11].Objective. To analyze the approach used in the clinic in patients with acute peritonitis, treatment methods, indications for surgery, type, volume of surgery, as well as morphological changes in the peritoneum.
2. Materials and Methods
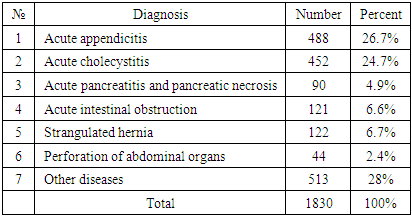
- The study was conducted on 1830 patients who were treated in the surgical department of Tashkent City Clinical Hospital No. 4 in 2023. This scientific work uses clinical, instrumental, morphological studies, surgical and conservative treatment, statistical methods of analysis. The medical records and surgical logs of 1830 patients treated for surgical diseases were retrospectively studied (Table 1). Of these, 488 (26.7%) patients had acute appendicitis, 452 (24.7%) patients had acute cholecystitis, 90 (4.9%) patients had pancreatitis, 121 (6.6%) patients had acute intestinal obstruction, 122 (6.7%) patients had strangulated hernia, 44 (2.4%) patients had perforation of abdominal organs, and the remaining 513 (28%) patients had other surgical diseases. Of these, 1190 (65%) patients underwent surgery, and 640 (35%) patients were treated conservatively.
|
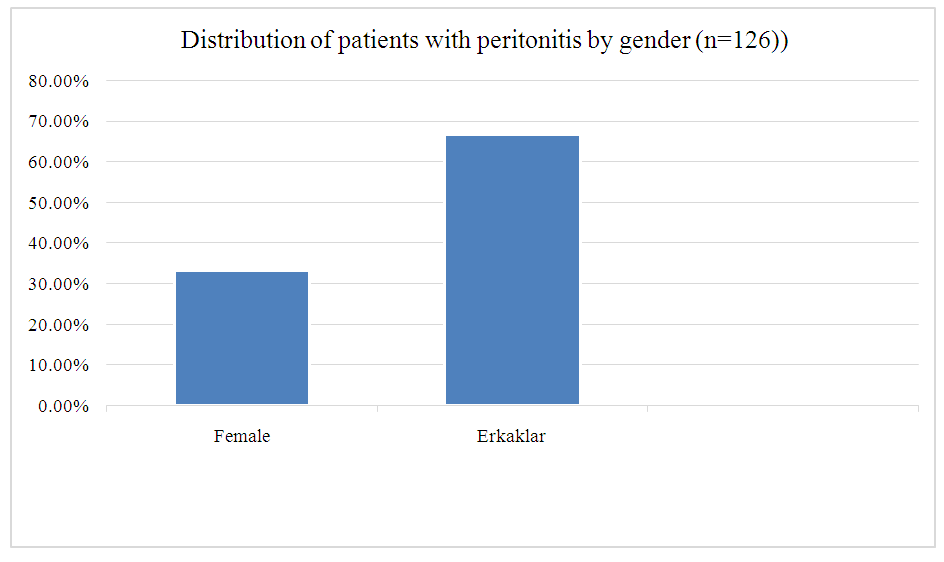 | Diagram 1. Distribution of patients with peritonitis by gender (n=126)) |
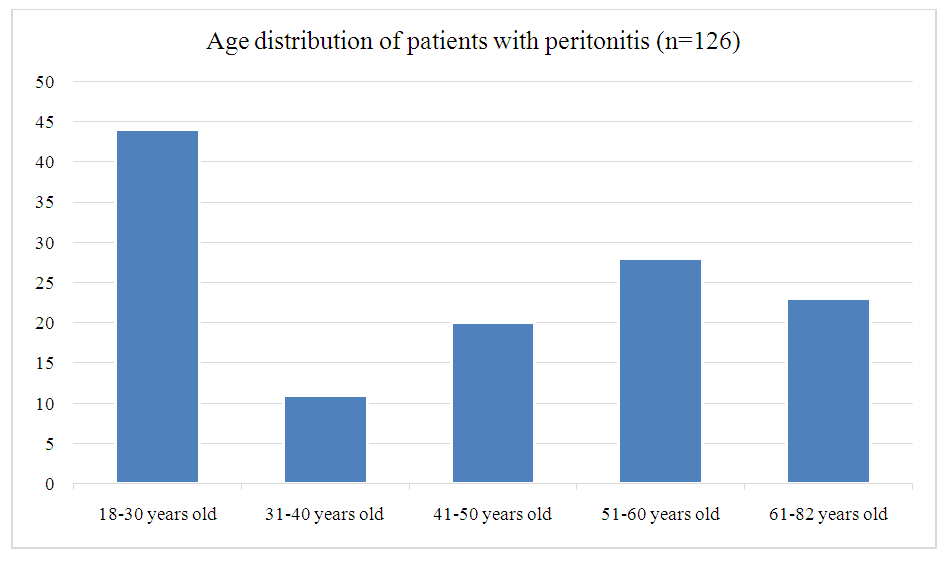 | Diagram 2. Age distribution of patients with peritonitis (n=126) |
3. Results and Discussion
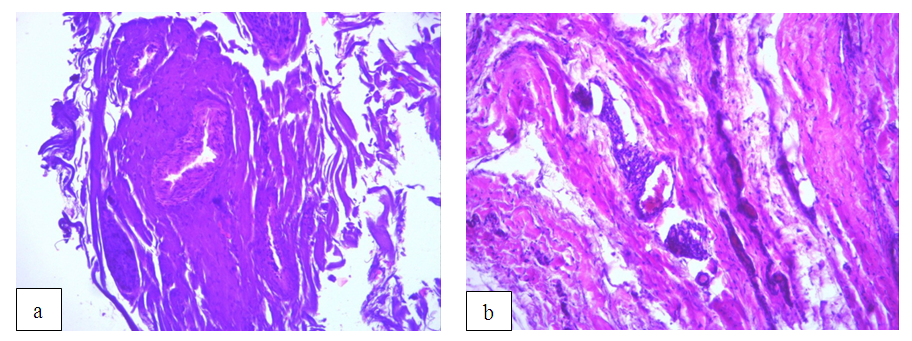
- Peritonitis in patients was caused by the following reasons: acute appendicitis - 43.6%; perforated gastric ulcer and duodenal ulcer - 34.9%; pancreatic necrosis - 2.4%; damage to the abdominal organs and retroperitoneal space - 3.2%; MDP (acute phlegmonous-stony cholecystitis, choledocholithiasis, empyema of the gallbladder) - 3.9%; strangulated hernia (inguinal, femoral, postoperative) - 3.2%; acute intestinal obstruction (adhesions, volvulus) - 2.4%; pancreatic tumor - 0.8%; mesenteric vein thrombosis - 2.4%; primary bacterial peritonitis (ascites-peritonitis) - 3.2%. The results of treatment of various forms of peritonitis were also analyzed. The patients were divided into two groups depending on the surgical approach:Group 1. The patients of this group (with diffuse and widespread peritonitis, n=80) underwent a single surgical intervention, during which the inflammation focus in the abdominal cavity was completely eliminated. Then the abdominal cavity was thoroughly cleaned and drained. The effectiveness of treatment in this group was 100%.Group 2. The patients of this group (n=46), complicated by widespread peritonitis, were treated using a semi-open method. The criteria for choosing this approach were: a) high level of bacterial contamination; b) impossibility of completely eliminating the inflammation focus in the abdominal cavity or factors aggravating it, the presence of multiple organ failure syndrome. Elective relaparotomies were performed 24-36 hours after the first surgical intervention. The effectiveness of treatment in this group depended on the following factors: the period of peritonitis development and the time before surgery, the initial severity of the patient's condition, the volume of the performed surgery, the effectiveness of intensive treatment methods and detoxification therapy. Mortality in this group was 21.7% (10 patients).At the next stage of scientific research, the morphological characteristics of the peritoneal areas taken during surgery were studied and analyzed [Figures 1 and 2].
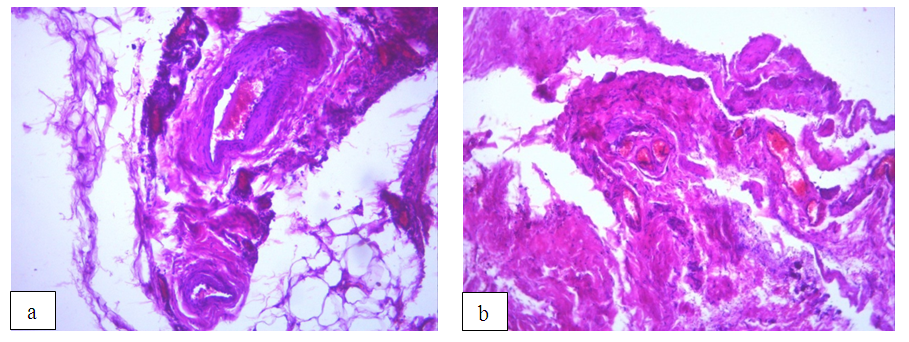 | Figure 1. (a, b). Venular stasis, impaired microcirculation, signs of edema, dense fibrous layer of vessels, GE, K.400 |
 | Figure 2. (a, b). Degranulated neutrophilic leukocytes, macrophages, fat droplets, and cell shadows are visible, GE., K.400 |
4. Conclusions
- Among the patients examined in the conducted scientific study, 126 (6.9%) patients with peritonitis were examined, of which 61% had diffuse peritonitis, and the remaining 39% had generalized peritonitis. The most common cause of peritonitis was destructive appendicitis - 43.6%. Mortality was higher in the group with generalized peritonitis - 21.7%.The duration and spread of the inflammatory process in peritonitis are directly related to the deepening of morphological changes in the fibrous and cellular structures of the peritoneum. Initially, there is swelling of fibrous structures, then hemorrhage, and in the remote period, disruption of the arrangement of fibers and blockage.As for the dynamics of the cell population, they first accumulate towards the walls of the vessels, which, as a result of endothelial dysfunction, causes subendothelial migration, and ultimately degranulation of neutrophilic leukocytes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML