Khaydarova Nargiza Akhtamjon kizi
Assistant of the Department of Forensic Medicine, Bukhara State Medical Institute, Uzbekistan
Correspondence to: Khaydarova Nargiza Akhtamjon kizi, Assistant of the Department of Forensic Medicine, Bukhara State Medical Institute, Uzbekistan.
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Introduction: This article presents an analysis of data obtained from macroscopic and microscopic examinations of thyroid tissue in 5-month-old white outbred rats of the control group, as well as an analysis of the similarities and differences in the morphological structure compared to the human thyroid gland. Methods: The scientific research was conducted at the Bukhara State Medical Institute named after Abu Ali ibn Sina until 2023 in the research laboratory of the institute. Results: The thyroid gland of white outbred rats, like in humans, is located in the neck in front of the larynx and consists of two lobes connected by an isthmus. Conclusion: Macroscopically, the thyroid gland tissue of 5-month-old white outbred rats in the control group is located in the anterior part of the trachea, consisting of right and left lobes connected by an isthmus. Microscopically, the gland is covered with a capsule, from which numerous trabeculae penetrate into the gland tissue. The main structural and functional unit of the gland is the follicle, which consists of thyrocyte cells arranged on the basement membrane, with colloid in the center.
Keywords:
Thyroid anatomy, Morphofunctional features, Histoarchitectonics, Morphological structure of the thyroid gland
Cite this paper: Khaydarova Nargiza Akhtamjon kizi, Analysis of the Morphofunctional and Morphometric Characteristics of the Thyroid Gland in 5-Month-Old White Outbred Rats of the Control Group, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1873-1875. doi: 10.5923/j.ajmms.20251506.50.
1. Introduction
This article presents an analysis of data obtained from macroscopic and microscopic examinations of thyroid tissue in 5-month-old white outbred rats of the control group, as well as an analysis of the similarities and differences in the morphological structure compared to the human thyroid gland. [1].
2. Methodology
For the experimental study, 28 white outbred rats of both male and female sex, aged 5 months, were selected. The laboratory animals chosen for the study were raised in the vivarium of Bukhara State Medical Institute. The experimental animals were kept in special rooms in accordance with the requirements for housing and conducting experiments, following the procedural rules approved by the Ethics Committee of Bukhara State Medical Institute "Rules for performing work using experimental animals" (No. 18 dated 16.01.2018). Experimental animalsweredecapitatedon an empty stomach under ether anesthesia, the thyroid gland tissue was isolated, and their general morphological and morphometric indicators were analyzed.
3. Results
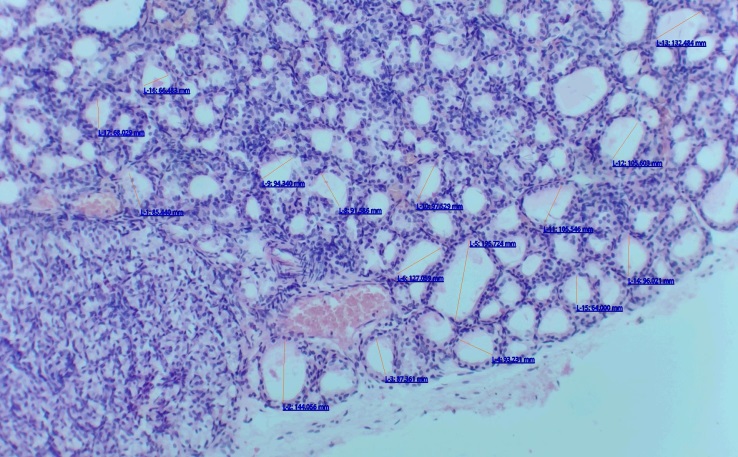
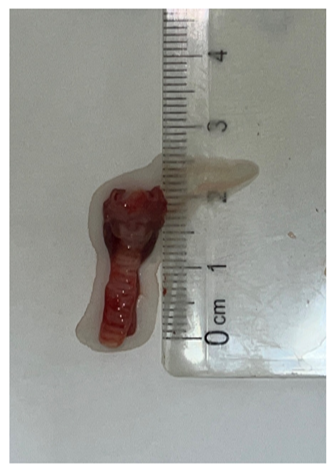
The thyroid gland of white outbred rats, like in humans, is located in the neck in front of the larynx and consists of two lobes connected by an isthmus (see Fig. 1). Hormones produced by the thyroid gland perform the following important functions in the body: cell growth, differentiation, oxygen consumption, and play a crucial role in basic metabolism. Biologically active substances produced by the thyroid gland play a direct and important role in the metabolism of proteins, fats, and carbohydrates. The thyroid gland is composed of thyroid follcles or thyroid follicles. 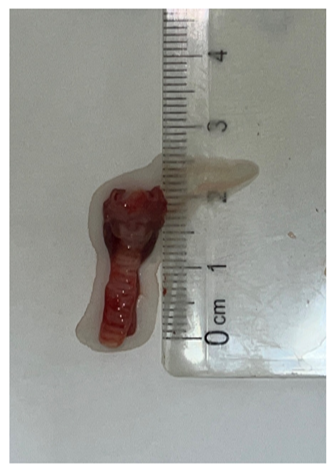 | Figure 1. Figure - macroscopic view of the thyroid gland of a 5-month-old white non-breed rat in the control group. Right lobe of the thyroid gland (1). Left lobe (2). Isthmus (3). Trachea (4) |
The follicular wall is composed of single epithelial cells. It is located along the wall of the follicle, and the jelly-like substance filling the center of the follicle is called colloid. Unlike other endocrine glands, the thyroid gland stores a large amount of secretory products. In the obtained sections, the follicular cells range from flat to columnar in shape. The thyroid gland capsule forms septa that penetrate into the gland's interior, becoming thinner and changing shape. These septa transform into irregular layers of connective tissue formed from reticular fibers, surrounding the follicles and separating them from each other. [2].The thyroid gland is richly supplied with blood vessels, which surround the follicles from all sides. One of the distinctive features of these vessels, particularly the capillaries, is their fenestrated endothelium, which enhances and facilitates the transport of molecules between the blood vessels and tissues. The morphological characteristics of thyroid follicles depend on the gland's region and functional activity; some follicles are large, others small, and consequently, the epithelial cells vary in shape. Some follicles are lined with cuboidal or squamous epithelium, while others are covered with columnar epithelium. The shape of thyrocyte cells can indicate the gland's functional activity; for instance, if the epithelial cells in the follicle are flat, the gland's functional state is considered hypoactive. Thyrocyte cells in the thyroid gland are located on the basal lamina and can simultaneously synthesize, secrete, and absorb proteins. Epithelial cells have basal and apical poles, with well-developed cellular organelles visible in the basal layer. The nuclei of epithelial cells are centrally located within the thyrocyte, round in shape, and normochromatically stained. In the apical part of the cell, small secretory granules containing colloidal substance are secreted towards the center of the follicle (see Fig. 2).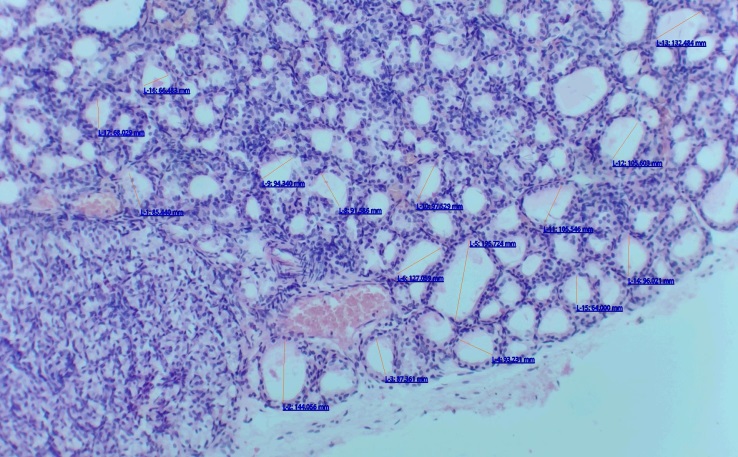 | Figure 2. Microscopic view of the thyroid gland of a 5-month-old white outbred rat. Stained with hematoxylin and eosin dye, magnified 200 times. Morphometric measurements of tissue structures in the thyroid gland are presented |
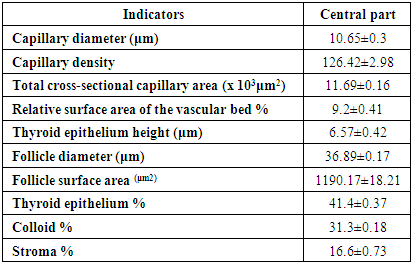
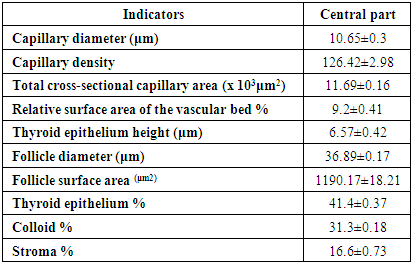
The thyroid gland contains two types of endocrine cells: T-thyrocytes or follicular cells, which develop from stem cells through various pathways. These cells produce iodine-containing hormones. The other type of cells are called C-thyrocytes or parafollicular cells. These cells produce thyrocalcitonin and various peptides. [3].The structure of the thyroid gland: the gland is covered externally by a capsule consisting of connective tissue. The layers formed from this capsule penetrate deep into the gland, dividing it into lobules. Between these lobules, numerous microcirculatory blood vessels and nerves are located. The main functional structures of the thyroid parenchyma are follicles. These follicles are closed spherical or slightly protruding hollow structures of various sizes, composed of a single layer of epithelial cells called follicular cells, along with parafollicular cells. [4] Within the thyroid gland lobules, follicular complexes can be distinguished, which are small lobules consisting of groups of follicles. Colloid substance secreted by T-thyrocytes accumulates in the follicular cavity. The size of the follicles and the thyrocyte cells that make up their walls fluctuate under normal physiological conditions. Thyrocyte cells in the follicle typically have a cuboidal shape. The follicles are separated from each other by thin, loose fibrous connective tissue. Additionally, numerous blood vessels, lymphatic capillaries, mast cells, and lymphocytes are observed in the gland. T-thyrocytes, or follicular endocrinocytes, are glandular cells that constitute the main part of the follicle wall. T-thyrocytes form the wall in follicles and are arranged in a single layer on the basement membrane. [5]. In a state of normal functional activity of the thyroid gland, T-thyrocytes are cuboid-shaped with spherical nuclei. Microvilli are present on the apical surface of T-thyrocytes facing the follicular cavity. With increased thyroid activity, the number and size of microvilli increase. Concurrently, the basal surface of T-thyrocytes under normal functional conditions is almost smooth. When functional activity increases, the surface of the basal layer develops numerous irregular folds and strengthens its interaction with cells located in the perifollicular area. [6]. The closely positioned cells are connected to the follicular cells by numerous desmosomes, and the terminal plates are also well-developed. With increased thyroid activity, finger-like protrusions appear at the lateral poles of the thyrocyte cells, compressing adjacent cells. In the thyroid gland, T and V thyrocytes are highly developed, especially the organelles involved in protein synthesis. Protein products are synthesized by T-thyrocytes, and the synthesized substances enter the follicular cavity, where the formation of iodine-containing tyrosine and tyramine occurs. Thyroid hormones are formed as a result of the breakdown of these thyroglobulins, which are released from these molecules for entry into the circulatory system. When the need for thyroid hormones increases, the functional activity of thyroid cells increases. In this case, the thyroid cells in the follicle become prismatic in shape, the consistency of the colloidal substance inside the follicle becomes liquid, and the number of resorption vacuoles increases significantly. If a decrease in the functional activity of the gland is observed, the amount of colloid in the follicle increases, and it becomes dense. The size of the thyroid cells in the follicle decreases, they flatten, and their nuclei shift towards the surface of the follicle.In addition, S-thyrocytes or parafollicular endocrinocytes of the thyroid gland are located in the follicle wall between the bases of T-thyrocytes, and their apical poles do not reach the follicle. They are also found in the connective tissue space between follicles. S-cells are larger than T-thyrocyte cells and are usually round, though some are angular in shape. These cells do not participate in the production of iodine-containing hormones but synthesize the oligopeptide hormones calcitonin and somatostatin. The cytoplasm of parafollicular cells contains numerous secretory granules. When distinguishing these cells, those filled with small granules and staining well with osmium tetroxide are considered calcitonin producers. Relatively larger cells that stain weakly with osmium tetroxide are identified as parafollicular cells that produce somatostatin.When analyzing morphometric indicators, the following results were obtained from examining thyroid gland parameters in white outbred rats. The average capillary diameter was 10.65±0.3 μm. The average density of capillaries was 126.42±2.98. The total cross-sectional surface area of capillaries was x 103 μm2, averaging 11.69±0.16. The relative surface area of the vascular bed averaged 9.2±0.41%.The height of the thyroid epithelium is 6.57±0.42 μm. The average follicle diameter is 36.89±0.89 μm, and the average follicle surface area is 2 1190.17±18.21 μm2. When considering the ratio of follicular components, the thyroid epithelium averages 40.2±0.32%. The colloid substance averages 32.1± 0.2%, and the stroma ratio is 17.5±0.5%. (Table 1)Table 1. Microcirculatory blood vessels of the thyroid gland and histomorphometric results of the gland in the control group of 5-month-old white outbred rats
 |
| |
|
4. Conclusions
Macroscopically, the thyroid gland tissue of 5-month-old white outbred rats in the control group is located in the anterior part of the trachea, consisting of right and left lobes connected by an isthmus. Microscopically, the gland is covered with a capsule, from which numerous trabeculae penetrate into the gland tissue. The main structural and functional unit of the gland is the follicle, which consists of thyrocyte cells arranged on the basement membrane, with colloid in the center. The activity of the thyroid gland can be assessed by the shape of thyrocyte cells. For example, flat thyrocyte cells and the presence of thick colloid in the follicle cavity indicate decreased gland activity, while prismatic thyrocyte cells and an abundance of vesicles in the colloid at the apical parts of the cells indicate increased gland activity. Morphometrically, the diameter of capillary blood vessels, the density and cross-sectional area of capillary blood vessels, the height of thyrocytes, the diameter and surface area of follicles, as well as the percentage ratio of glandular epithelium, colloid, stroma, and glandular blood vessels were studied, and the average normal values were determined. Since these indicators of the thyroid gland are very close to those of the human body, they allow for experimental study of diseases occurring in the human body.
References
| [1] | Anikin G. S., Stoykova I. V., Kukes V. G. Nonsteroidal anti-inflammatory drugs: safety from the perspective of evidence-based medicine // Consilium Medicum. - 2017. - Vol. 19. - No. 7-2. - P. 28-32. |
| [2] | Akhmediya R. E. et al. Nonsteroidal anti-inflammatory drugs: recommendations and precautions for safe use in a multidisciplinary surgical department // Medicine and Ecology. - 2024. - No. 3. - P. 105-112. |
| [3] | Akhrarov Kh. Kh. et al. The thyroid gland and its functional features //The 11th International scientific and practical conference "European congress of scientific achievements" (November 4-6, 2024) Barca Academy Publishing, Barcelona, Spain. 2024. 547 p. - 2024. - P. 46. |
| [4] | Lesnaya O. A. et al. Rational use of NSAIDs in light of clinical recommendations and data from new research // Difficult Patient. - 2019. - Vol. 17. - No. 10. - P. 31-34. |
| [5] | Lesnaya O. A. Nonsteroidal anti-inflammatory drugs: more than 30 years at the peak of relevance // Difficult Patient. - 2018. - Vol. 16. - No. 11. - P. 45-49. |
| [6] | Mayev I. V. et al. Gastropathies induced by nonsteroidal anti-inflammatory drugs: pathogenetically justified. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML