-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1859-1863
doi:10.5923/j.ajmms.20251506.47
Received: May 13, 2025; Accepted: Jun. 9, 2025; Published: Jun. 14, 2025

Laboratory Data Peculiarities of Children with Suspected Sepsis
G. Sh. Khamrayeva1, Sh. K. Razikova2, S. R. Rakhimova2, G. Kh. Ismagilova2, M. A. Kholmatova2, U. P. Burieva2, N. T. Mirakbarova2
1Center for Development of Professional Qualification of Medical Workers, Tashkent, Uzbekistan
2Republican Research Center of Emergency Medicine, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to investigate the peculiarities of microbiological landscape and levels of blood inflammatory markers in sepsis in early age children. Background. Globally, there are an estimated 22 cases of childhood sepsis per 100,000 populations and 2,202 cases of neonatal sepsis per 100,000 live births, corresponding to 1.2 million cases of childhood sepsis per year. Material and Methods. Medical examination of 100 children aged 1 month to 3 years admitted to hospital with sepsis in 2022-2024 was conducted at the Republican Research Center of Emergency Medicine in order to improve diagnostic and intensive treatment tactics of children with sepsis. Results. The etiologic structure of sepsis was dominated by Gram-positive flora - 71.6%. Gram-negative flora amounted to 23.9%, fungi - 4.4%. Conclusions. The level of presepsin above 325 ng/l on the 1-3rd day of hospitalization indicates the development of sepsis on the background of pneumonia.
Keywords: Pediatrics, Sepsis, Blood microbiological analysis
Cite this paper: G. Sh. Khamrayeva, Sh. K. Razikova, S. R. Rakhimova, G. Kh. Ismagilova, M. A. Kholmatova, U. P. Burieva, N. T. Mirakbarova, Laboratory Data Peculiarities of Children with Suspected Sepsis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1859-1863. doi: 10.5923/j.ajmms.20251506.47.
Article Outline
1. Introduction
- The problem of sepsis morbidity remains one of the most difficult current problems of medical science. Sepsis is the leading cause of morbidity, mortality and medical care-seeking in children worldwide. The increased attention to sepsis and septic shock by specialists is due to the following reasons: high mortality rate, increasing number of cases, difficulties in making the diagnosis.In 1992, a consensus conference of the American College of Pulmonologists (ACCP) and the Society of Critical Care Medicine (SCCM) developed recommendations that form the basis for the modern classification, diagnostics and treatment of sepsis. The concepts of "systemic inflammatory response syndrome" (SIRS) were established, and definitions were given for "sepsis", "severe sepsis", and "septic shock". The definitions were designated as "Sepsis-1", and the clarifications/definitions that appeared later in 2001 and 2016 were "Sepsis-2" and "Sepsis-3", respectively.Globally, there are an estimated 22 cases of childhood sepsis per 100,000 populations and 2,202 cases of neonatal sepsis per 100,000 live births, corresponding to 1.2 million cases of childhood sepsis per year [1]. Over 4% of all hospitalized patients under 18 years of age and ~8% of patients admitted to intensive care units in high-income countries suffer from sepsis [2–6]. Mortality in children with sepsis ranges from 4% to 50% depending on severity of the disease, risk factors, and geographic location [2-3,7-9]. Most children dying from sepsis suffer from refractory shock or multi-organ dysfunction syndrome, and many deaths occur within the first 48-72 hours of treatment [10,13]. Thus, early detection and appropriate resuscitation and treatment are critical for optimizing outcomes in children with sepsis.In early-age children due to the imperfection of the thermoregulatory, excretory and respiratory systems, the generalization of the inflammatory process occurs much faster, and therefore sepsis is 10 times more common in children under one year of age than in older children. The number of hospitalizations due to sepsis per 100,000 people increased from 143 in 2000 to 343 in 2007 [2]. A 5-year analysis of pediatric and nononatal sepsis statistics (children aged 0 to 19 years) in seven U.S. states revealed that the incidence of severe pediatric sepsis increased from 45% to 81%, and the incidence of severe neonatal sepsis increased from 4.5 to 9.7 cases per 1,000 births [10].Results of another international study, including a study of sepsis in 198 intensive care units in 24 European countries, showed that the most common pathogens were Staphylococcus aureus (30%, including 14% resistant to methicillin), Pseudomonas spp. (14%) and Escherichia coli (13%). In multivariate analysis, Pseudomonas spp. was the only microorganism associated with increased sepsis mortality [6].The leading cause of sepsis is infections of the respiratory system, including the lungs and upper respiratory tract (on average 42%), followed by infections of the abdominal organs, as well as urinary tract infections (on average 18% and 18.4%, respectively). Bloodstream infections, including catheter-associated infections, are the third leading cause of sepsis (4% on average). Skin and soft tissue infections account for an average of 3.6%, while cardiovascular, central and peripheral nervous system infections account for less than 0.5%.Considering the high mortality rate of sepsis and its high social and economic importance, there is a need for a marker with the following features: rapid and specific elevation in sepsis, rapid response to ongoing antibiotic therapy, and a widely available, reliable and rapid method of detection. Circulating biomarkers can help in the diagnosis and administration of antimicrobial therapy to patients with sepsis, but few of them have proven useful for individual prognostic stratification [4-5]. Today, the determination of procalcitonin and C-reactive protein in the blood is used to diagnose sepsis and septic shock. But recent scientific studies have proven the nonspecificity of these inflammatory markers in sepsis. In 2005, a group of researchers from Iwate Medical University (Japan) discovered Presepsin (sCD14-ST), which is a soluble N-terminal fragment of the cluster of differentiation (CD) marker protein CD14, which is released into the bloodstream during monocyte activation upon recognition of lipopolysaccharide (LPS) from infectious agents [6]. Presepsin is proposed to be used as an early marker for recognizing sepsis, for monitoring antimicrobial therapy, and as a prognostic marker [3]. Higher baseline presepsin levels are directly correlated with higher mortality rates in intensive care unit patients with septic shock, according to separate studies [6]. Determination of presepsin in blood allows diagnosing CD14-cell activation at the earliest time of sepsis development, ahead of other indicators such as procalcitonin and C-reactive protein [13].The aim of the study was to investigate the peculiarities of microbiological landscape and levels of blood inflammatory markers in sepsis in early age children.
2. Material and Methods
- In order to improve diagnostic and intensive treatment tactics for children with sepsis, we conducted a medical examination of 100 children aged 1 month to 3 years hospitalized with sepsis in 2022-2024 in the Department of Somatic Resuscitation and Intensive Care Unit of the Republican Research Center of Emergency Medicine. The patients were divided into two groups: Main group (n=55) and Control group (n=45). The Main group included patients aged from 1 month to 3 years with a qSOFA score over 2 on admission, a pSOFA score over 2 on admission, and suspected or confirmed pneumonia complicated by sepsis. The Control group included children aged from 1 month to 3 years with a qSOFA score of more than 2 at admission to the emergency room, but with a pSOFA score of less than 2 in the ICU with a diagnosis of pneumonia uncomplicated by sepsis.Inclusion criteria for the study were:- children with complicated births;- patients with suspected immunodeficiency;- the presence of two or more clinical manifestations of sepsis according to the p SOFA scale.Exclusion criteria were as follows:- newborns and children under 1 month;- genetic pathology and metabolic diseases;- multiple malformations, congenital heart and kidney defects;- patients with a previously confirmed diagnosis of sepsis.The following investigation methods were used:• Physical examination methods (measuring temperature, heart rate, respiratory rate, blood pressure);• General blood test, biochemical blood test (total protein, urea, creatinine, bilirubin, potassium, medium molecular weight peptides, LDH, albumin, ALT, AST);• Inflammatory markers: procalcitonin, lactate, C-reactive protein and presepsin;• Instrumental research methods (chest X-ray, ECG, MSCT, ultrasound).In all patients included in the study, 2 ml of blood was taken before starting antibiotic treatment to ensure the accuracy of blood microbiologic results. The investigated material was cultured on several nutrient media in order to grow and identify the maximum number of pathogens. The nutrient medium consisted of 1.7%-2% agar and a semi-liquid medium prepared from broth with the addition of glucose and agar. Antibiotic susceptibility was tested using the traditional disc method. Microbiological examination was carried out in the bacteriological laboratory of the Republican Research Center of Emergency Medicine. All patients underwent blood plasma analysis for Presepsin marker to diagnose sepsis early. The main material for the study was blood taken from peripheral and central veins of the patients. Venous blood taken from the patient and plasma was stored at -20°C with all storage rules being observed, strictly following the instructions provided by the manufacturers of the test system.A MINDREY BC-5300 hematology analyzer for general blood analysis (Shenzhen Mindray Bio-Medical Electronics Co., Ltd., China) was used.
3. Results
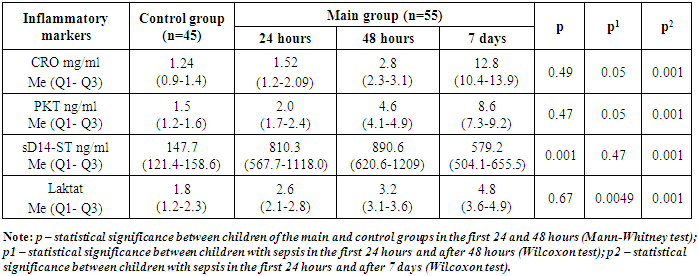
- When studying blood sterility, microbial growth was detected in 32 patients of the main group, which amounted to 71%. Gram-positive flora prevailed in the etiological structure of sepsis - 71.6%. Gram-negative flora amounted to 23.9%, fungi - 4.4%.In the analysis of Gram-positive microflora, S. epidermidis was 35.1%, S. aureus was 18.8%, Enterococcusfaecium and Streptococcusviridians were 9.4% and 8.2%, respectively (Fig. 1).
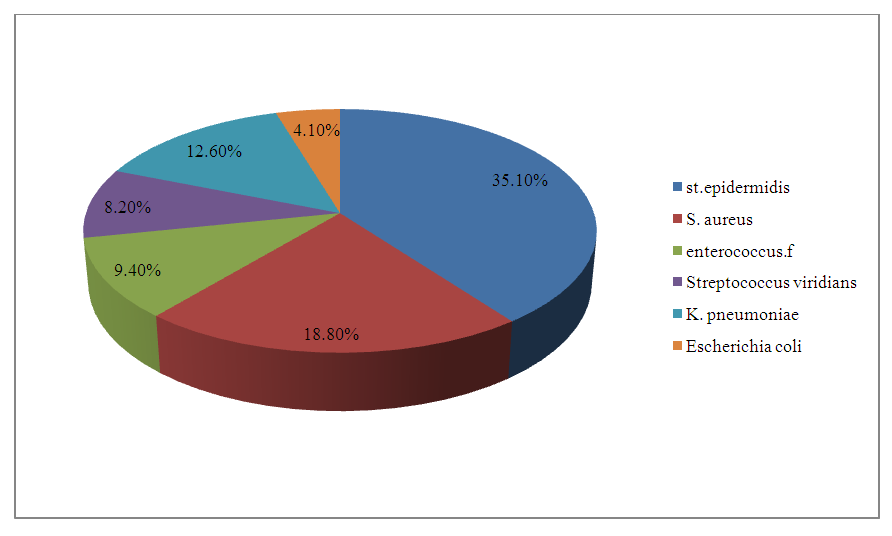 | Figure 1. Microbiological blood culture |
|
4. Discussion
- Most of the identified microorganisms were found to be sensitive to commonly used antibiotics (Fig. 2).
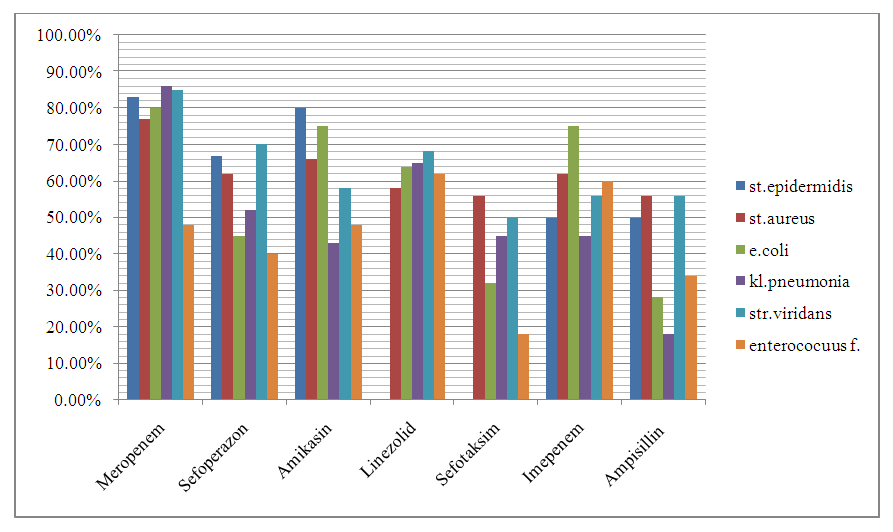 | Figure 2. Sensitivity of cultured microorganisms to antibiotics |
5. Conclusions
- Thus, despite modern methods of diagnostics and treatment of sepsis, the latest recommendations for the management of children with sepsis and septic shock, the problem of mortality and disability remains an urgent problem in pediatrics. Early diagnostics, timely antibiotic therapy and correct evaluation of the severity of the condition can be the basis for preserving the patient's life. We can say from the research papers we have studied that presepsin offers great potential as an early marker for recognizing sepsis. Increased presepsin concentration can serve as an early diagnostic marker of bacterial infection, as its level rises earlier than the level of traditional inflammatory markers (C-reactive protein, procalcitonin), and its high levels indicate severe development and course of sepsis in children. A decrease in the level of presepsin can serve as a prognostically favorable indicator of the course of the disease or a reliable marker of the efficiency of antibacterial therapy, because when monitoring the therapy of sepsis, it reflects the degree of its efficiency faster and more reliably than CRP and procalcitonin.Gram-positive bacteria remain the leading cause of sepsis in early age children. It can be said that a high titer of bacteria in the microbiological blood test corresponds to the severity of the patient's condition. Despite the diverse etiologies of sepsis, its clinical manifestations remain very similar and nonspecific.
Conflict of Interests’ Statement
- The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
ACKNOWLEDGMENTS
- The authors express their gratitude to the management of the multidisciplinary clinic of Republican Research Center of Emergency Medicine for the material provided for our study.
Ethical Approval and Consent to Participate
- The Research Ethics Board of our institution does not require review or approval of case reports. Our research was carried out in accordance with the World Medical Association Code of Ethics (Declaration of Helsinki).
Source of Funding
- Each of the authors has reviewed and approved this manuscript. None of the authors has a conflict of interest, financial or otherwise. This manuscript is original, no part of it has been previously published and is not being considered for publication elsewhere. The corresponding author agrees to accept full responsibility for authorship at the submission and review stages of the manuscript.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML