-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1831-1833
doi:10.5923/j.ajmms.20251506.41
Received: Apr. 11, 2025; Accepted: May 8, 2025; Published: Jun. 10, 2025

Pathogenetic Role of Violation in the Cytokine System in Non-Specific Interstitial Pneumonia
Zakiryayeva Parvina Odilovna1, Ismailov Jamshed Abduraimovich2, Kamalov Zainitdin Saifutdinovich3
1Assistant Professor, Department of Internal Medicine, Samarkand State Medical University No. 4, Samarkand, Uzbekistan
2DSc, Associate Professor, Head of the Department of Internal Medicine No. 4, Samarkand State Medical University, Samarkand, Uzbekistan
3MD, Professor, Head of the Laboratory of the Institute of Immunology and Human Genomics of the Academy of Sciences of the Republic of Uzbekistan, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

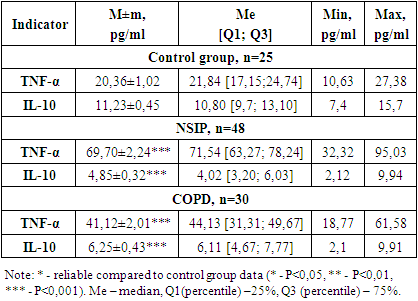
PURPOSE: study of the role of production of pro- (TNFα) and anti-inflammatory (IL10) cytokines in the prognosis of the course of non-specific interstitial pneumonia. MATERIAL AND METHODS: Blood serum of 78 patients with NSIP and COPD. The control group consisted of 25 practically healthy people of the same age. The concentration of TNFα and IL-10 in the blood serum is determined by the method of solid-phase enzyme immunoassay using the AO-Vector-Best test (Novosibirsk, Russia). RESULTS: Characteristic features of the level of secretion of cytokines TNFα and IL-10 in the blood serum of patients with NSIP in comparison with COPD were established, which indicates a significant role of these cytokines in the pathogenesis of fibrosis.
Keywords: Pneumonia, Cytokines, Serum, Imbalance
Cite this paper: Zakiryayeva Parvina Odilovna, Ismailov Jamshed Abduraimovich, Kamalov Zainitdin Saifutdinovich, Pathogenetic Role of Violation in the Cytokine System in Non-Specific Interstitial Pneumonia, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1831-1833. doi: 10.5923/j.ajmms.20251506.41.
1. Introduction
- In recent decades, the discovery of cytokines and their regulatory role in the immune response has determined the priorities of research in this area in various pathological processes. [4]. It has been shown that cytokine deficiency contributes to the development of a number of diseases, and their normal content increases the body's resistance to infections [6].There is quite a lot of evidence of the pathogenetic role of cytokines and imbalance in their system in respiratory diseases [2]. But despite intensive research into the process of lung damage in pneumonia [3], Until now, the role of various cytokines has not been determined, the issues of identifying integral markers of the development of the pathological process in the lungs in pneumonia associated with different etiological agents, as well as the role of the etiological factor in the development of pneumonia have not been resolved [1].Pulmonary fibrosis is a chronic and progressive tissue repair response that results in irreversible scarring and remodeling of the lung, characterized by high mortality and limited treatment options [13]. Non-specific interstitial pneumonia (NSIP) is the most devastating progressive interstitial lung disease that remains refractory to treatment. The pathogenesis of NSIP is based on aberrant crosstalk, which also damaged alveolar cells and myofibroblasts, ultimately leading to an aberrant fibrotic reaction. Recent evidence suggests that both innate and adaptive immune responses may be involved in the fibrotic process. The contribution of the immune system to the development of NSIP remains poorly understood [11].In connection with the above, the aim of this study was to investigate the role of production of pro- (TNFα) and anti-inflammatory (IL10) cytokines in assessing the prognosis of the course of nonspecific interstitial pneumonia.
2. Material and Methods
- The present study involved 103 women and men. All examined individuals were divided into 3 groups: Group 1 consisted of 14 men and 34 women with an established diagnosis of NSIP (48), Group 2 for comparison consisted of 13 men and 17 women with COPD (30), and the control group included 25 practically healthy individuals. Immunological studies of the examined patients were conducted in the laboratory of immunoregulation of the Institute of Human Immunology and Genomics of the Academy of Sciences of the Republic of Uzbekistan. The concentration of tumor necrosis factor alpha (TNFα) and interleukin-10 (IL10) in the peripheral blood serum was determined by solid-phase enzyme-linked immunosorbent assay using test systems from JSC VECTOR-BEST (Russia, Novosibirsk). The quantitative evaluation of the results was carried out by constructing a calibration curve reflecting the dependence of optical density on concentration for a standard antigen and allowing comparison of the studied samples with it. Statistical processing of the obtained data was performed using the Statistica 6.0 computer program. The reliability of differences in the mean values (p) of the compared indicators was assessed using the Student's criterion (t).
3. Results and Discussion
- A decisive role in immune surveillance of the lungs, connecting innate and adaptive immunity, is played by many immunocompetent cells (ICC), which are producers of immune response mediators (cytokines). Resident alveolar macrophages and monocytes recruited to the lungs play an important role in enhancing the inflammatory response in the lower respiratory tract [10]. Any inflammatory process begins with the formation of a focus of inflammation and the synthesis of key mediators of the immune response, which is tumor necrosis factor alpha (TNFα). TNFα – occupies a special place among cytokines. The main producers are monocytes and macrophages. It is also secreted by neutrophils, endothelial and epithelial cells, eosinophils, mast cells, B and T lymphocytes when they are involved in the inflammatory process. The biological properties of TNFα are extremely diverse and depend on the predominance of one or another cytokine from its family [8]. TNFα enhances the expression of adhesion molecules, the synthesis of proinflammatory cytokines and chemokines, acute phase proteins, phagocytic cell enzymes, etc. TNFα is involved in the formation of all major local, as well as some systemic manifestations of inflammation [7].The results we obtained are presented in Table 1.
|
4. Conclusions
- 1. Analysis of serum TNFα levels showed that in the group of patients with NSIP, the cachexin content was increased by 3.4 times.2. It was revealed that IL-10 synthesis in the group of patients with NSIP was reduced by 56.8%.3. The results obtained indicate a profound disruption of the regulatory system of cytokines responsible for the regulation of humoral, cellular and nonspecific immunity.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML