-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1810-1816
doi:10.5923/j.ajmms.20251506.36
Received: May 18, 2025; Accepted: Jun. 3, 2025; Published: Jun. 7, 2025

A Modified Sparing Uranoplasty to Preserve the Topographic Structure of the Eustachian Tube
M. E. Makhkamov1, O. K. Baltabaev2, N. E. Makhkamova1
1Tashkent State Dental Institute, Uzbekistan
2Republican Multidisciplinary Medical Center named after U. Khalmuratov, Located in Nukus, Karakalpakstan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Congenital cleft palate is one of the most severe forms of malformations of the maxillofacial region. Preoperative orthodontic preparation is necessary for successful primary early or bicycle surgery. With early veloplasty before cheiloplasty, the strength of muscles and scars leads to the expansion of the cleft lip. Early performed cheiloplasty leads to a decrease in pathological changes in the tissues of the nasopharyngeal space.
Keywords: Congenital cleft palate, Palatopharyngeal insufficiency, Eustachian tube
Cite this paper: M. E. Makhkamov, O. K. Baltabaev, N. E. Makhkamova, A Modified Sparing Uranoplasty to Preserve the Topographic Structure of the Eustachian Tube, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1810-1816. doi: 10.5923/j.ajmms.20251506.36.
1. Introduction
- Improving surgical treatments for congenital cleft palates has more than 200 years of history. To date, wide varieties of surgical techniques have been developed.Langenbeck described the principle of using local tissues to surgically close the cleft palate in 1861. Langenbeck proposed to cover the crevice with the convergence of tissues of soft palate and mucosal extremities from hard palate. The Langenbeck method does not involve elongation of the palate and narrowing of the pharyngeal ring [36; 337].A.A. Limberg developed radical uranoplasty, which allows to simultaneously solving all the tasks facing the surgeon: fissurorrhaphy, retrotransposition, mesopharyngoconstriction [23; 595]. Yu.I. Vernadsky improved the technique of surgery, developed 26 variants of palate plasty, applied depending on the nature of the defect [3; 21].Schweckendiek (1979) proposed to operate the cleft palate in two stages: in the first months of life, to produce only soft palate plastics (veloplastics), and the second stage - to close the cleft in the anterior section of the hard palate - to produce at the age of 5-6 years [49; 262]. Schweckendieck’s assumption of two-stage surgery can be considered theoretically valid, as the technique ensures early recovery of speech and acoustic tube function and prevents facial deformation [40; 73-77]. There are a large number of variants of uranoplasty in which operative treatment is carried out in two stages [6; 63, 8; 151, 10; 59, 22; 110-112, 28; 40, 32; 45, 35; 112-115]. Modifications and new techniques are known using the basic elements of radical uranoplasty [3; 21, 11; 18, 14; 20, 37; 51-59, 38; 270-277].By studying the pathomorphological and functional disorders in the tissues and organs of the face-jaw area with the accumulation of lip and palate, using new data on the pathogenesis of deformities, it was concluded that B.N.Davydov, R.D.Novoselov (1983) proposed a number of basic surgical methods; it is used in 3 different options, depending on the index of non-cohesion, the degree of contraction of the hard and soft palate, the activity of the muscles of the pharynx. The authors suggest that children who are not partially attached to the palate are operated on 4-5 years old, incomplete and unilateral and bilateral - 6-7 years old. By describing the anatomical features of the smooth palate muscles without Fusion, they do not recommend surgical procedures such as tendon dislocation to break the pterygoid hook according to Billrot and reduce the tension of the buttocks [13; 18].T.F.Vinogradova believes that the optimal period for operation in the sky is preschool age, and this is a social change in the life of the child and emphasizes the need to enter the school community at 6-7 years old [5; 256].At the same time, according to a number of authors, the main bone diseases are associated with an alveolar process and a very pronounced defect in the laying of the Palatine tissue. Supporters of this theory of deformation development insist on a complete surgical recovery of anatomical relations in early childhood, followed by orthopedic treatment [46; 104-111, 55; 142-148].M.Fara (1989) believes that a one-stage operation on the complete closure of the palate defect can be performed at 3 years old, when the cross-growth of the upper jaw slows down. However, such a complication as deformation of the upper jaw is rarely observed, at the same time, the function of the pharyngeal closure and auditory tube is well restored [45; 134-141].An increase in the quality of surgical treatment of congenital insertions of the palate against the background of a decrease in the invisibility of the intervention allowed uranoplasty to be recommended not at a late preschool age (5-7 years), but a little earlier - at a young age. 2-4 years [1; 20, 3; 21, 7; 60-62, 8; 151, 9; 48-49, 10; 59, 15; 91-94, 16; 68, 28; 40, 29; 26-27]. This requires the participation of orthodontists in the preparation for the operation and the management of the child in the postoperative period in order to avoid jaw deformation in the postoperative period [2; 40, 4; 282-286, 17; 91-93, 18; 163, 19; 71, 41; 183-184, 48; 181-185, 51; 207-215, 52; 57-68].T.V. Sharova (1985) and others believe that orthodontic treatment before surgery has a positive effect on the growth of maxillary Arc [39; 36, 41; 183-184].The above shows that from the point of view of the time of surgical treatment, on the one hand, a rational compromise tactic is necessary to prevent the risk of serious violations of the development of the upper jaw and restore integrity; on the other hand, as soon as possible of the closure of the pharyngeal as an articulating organ.At the same time, on the basis of literature analysis, a clear trend is observed in relation to the previous periods of surgery, while the techniques and methods of plastic surgery are constantly being improved in order to reduce trauma [20; 235-239, 21; 20, 27; 151-155, 25; 117-118, 26; 122-123, 33; 155]. There are publications on the conduct of one-two-stage uranoplasty in patients under the age of 1 year [22; 110-112, 31; 16-18, 33; 155].Despite the existing differences in views on the timing of carrying out uranoplasty, a clear trend has recently been identified - it is recommended that surgical treatment of the deposition of the palate be carried out sooner.Analysis of the direct and long-term results of surgical treatment of children with congenital palatal fractures by a variety of surgical methods shows a high percentage of unsatisfactory results in the form of postoperative defects, the rehabilitation of these patients requires additional surgical intervention [42; 80-83, 43; 35, 53; 423-429]. After primary uranoplasty, there is a narrowing of the soft palate and changes in the cicatricial, which is observed in 30-82, 6% of cases [41; 183-184, 50; 112-122], which leads to palatopharyngeal insufficiency and impaired speech function, which in some cases requires repeated surgical treatment [12; 33, 30; 152-153, 37; 55-59, 54; 613-618].
2. The Main Findings and Results
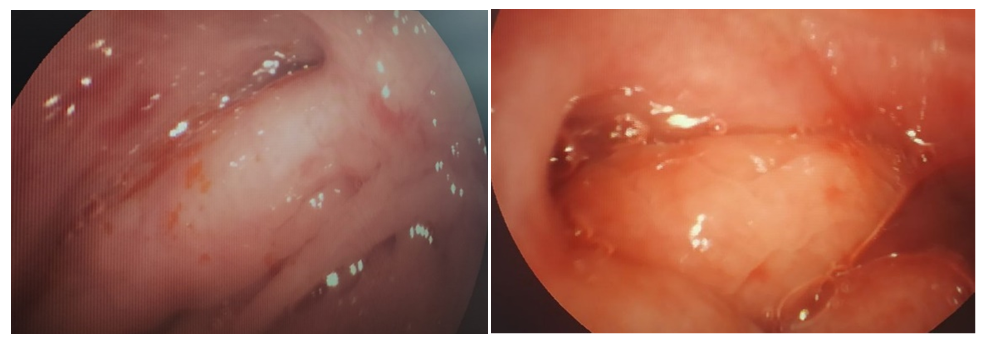
- The most popular of the lengthening methods is the “Oxford Palatplasty” (V-Y - push back or “толчок кзади”). This technique initially does not increase the length of the palate, but adds the amount of muscle detached from the back edge of the hard palate. The transverse cuts of the new mucous membrane in the area of the boundaries of the hard and soft palate release the tissues and allow them to move back. However, according to W.Lindsay (1996), this results in pathological scarring [47; 881-884].Therefore, many options have been proposed to close the wound surface of the nasal mucosa of the soft palate. T.Cronin (1957) proposed dissecting the nasal mucous membrane by 1 cm from the back edge of the solid palate, then moving the mucous membrane and binding it to soft palate tissues [44; 474-484].Some authors suggest that the muscles of the soft palate be detached and stitched transversely instead of inclined. This technique ensured that the defect of the palate was closed in three layers: nasal mucosa, muscles and oral mucosa. This method is a variant of the “intravelar veloplasty” method proposed by F. Braithwaite in 1968.To the same group of operations can be attributed and the method proposed by Ad.A.Mammadov in 1995, while groups of muscles of the soft palate were stitched “joint at the junction” or “overlap”. On the basis of this method together with A.G.Leonov and H.A.Koryakin in 1995; a modification differs in the advanced preparation m. Tensor veli palatini, careful mobilization and stitching “end to end” [24; 309].L.E.Frolova proposed in 1972 the plastic of the palate with a contraction of the vaginal-pharyngeal ring, with incisions running along the edges of the crevices continuing under the bases of the tongue and transitioning to the side wall of the throat, forming the oral and nasal mucous-muscle layers. The method was widely used as it yielded positive results in all forms of cleft of the palate. On its basis, during the period 1988-1989 Ad.A.Mammadov created several modifications used in the treatment of isolated cleft palate [24; 309].It should be noted that operative interventions on the roof require professionalism and thoroughness. Roof plastic in the hands of a particular author is most often a complete surgical method, performed qualitatively and efficiently, but this plastic can give negative results in the hands of another, less experienced surgeon [24; 309]. Certainly, when assessing the quality of palate surgery, it is necessary to take into account the form of pathology, the degree of injury, the age of the patient and many other related circumstances that make up, so to speak, the surgical personality of the patient. Synchronization plays an important role in the interpretation of results. The method performed by the surgeon in patients of different age groups can give different results, i.e. when interpreting the results it is necessary to take into account the shape, degree, severity of pathology and age of the patient [34; 175-196, 45; 134-141].However, it should be recognized that all variants of this sparing method of uranoplasty have their usual shortcomings: in some cases, the scarring of the wound occurs in the postoperative period, after the operation, the soft palate muscles are again attached to the back edges of the Palatine plates with a scar, which leads to a wrinkle and a significant reduction of the soft palate; the presence of a soft palate and a noticeable linear wound in the area of the nasal.The above disadvantages do not allow the normal operation of a soft palate. There is a palatopharyngeal insufficiency - the penetration of air into the nasal cavity of the pharynx during phonation and the outflow of liquid food from the oropharynx into the nose. Violation of the function of speech and nutrition does not allow the patient to fully socialize. This requires repeated surgical treatment and long-term rehabilitation (Figure 1).
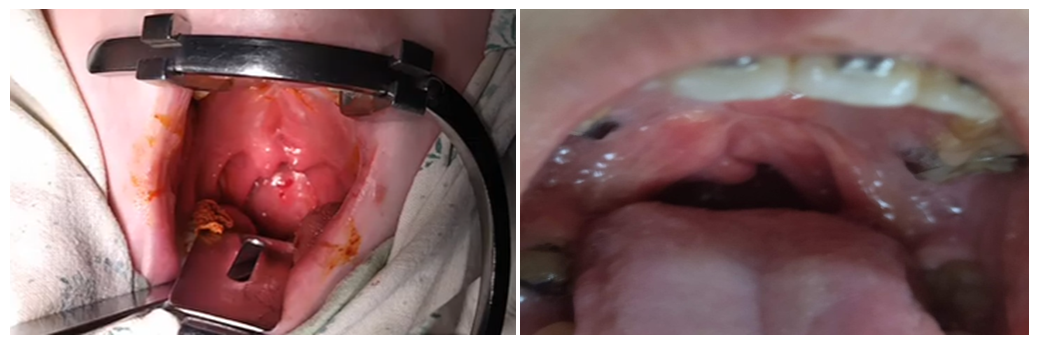 | Figure 1. Scarring of soft palate and weakness of pharyngeal ring |
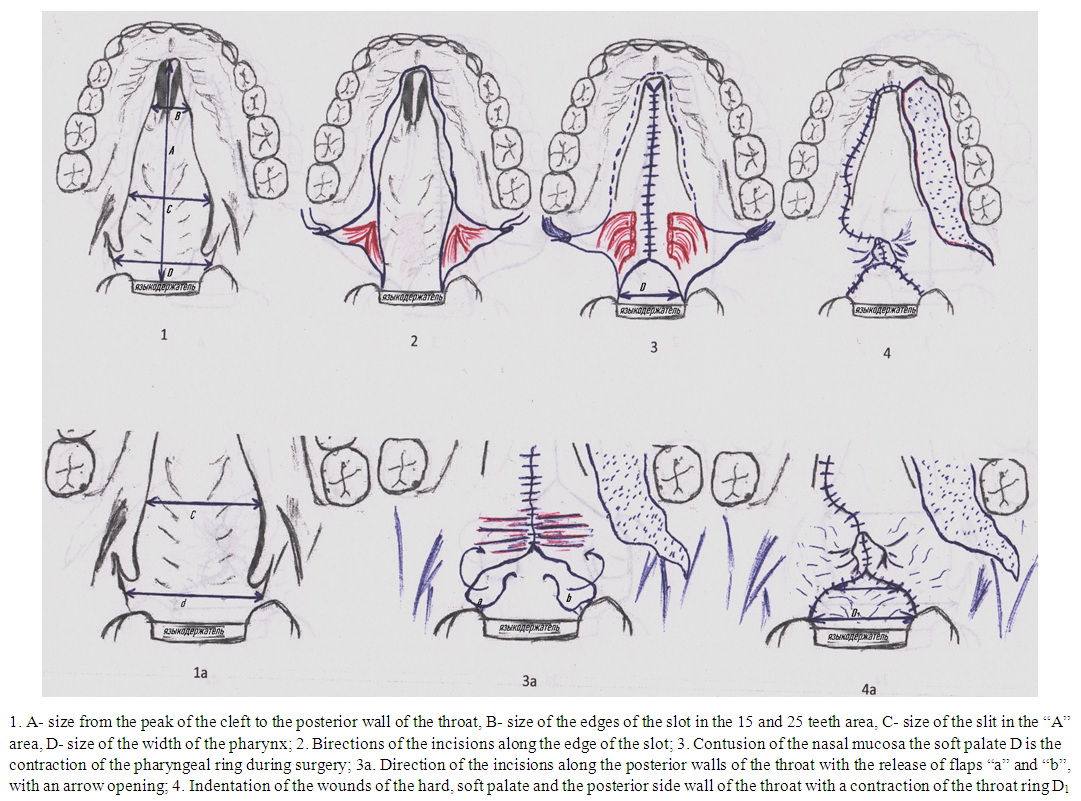 | Figure 2. Stage Diagram of the Modified Uranoplasty Method by Makkamov E.U. |
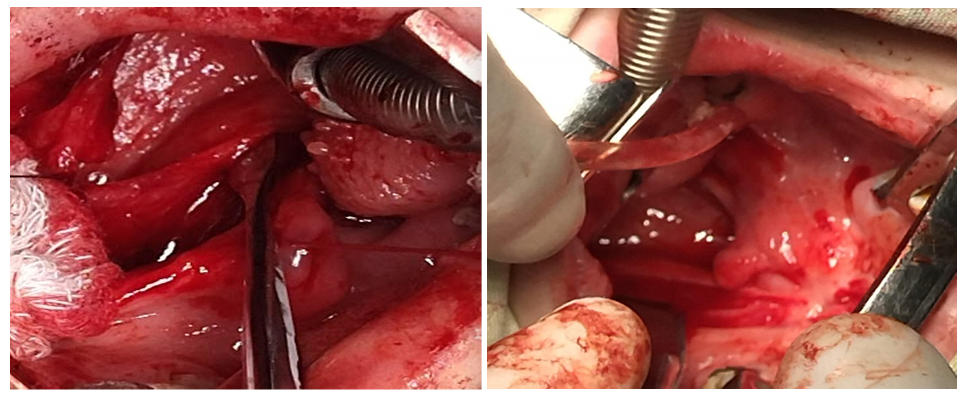 | Figure 3. Immobilization of the side and back walls of the pharynx |
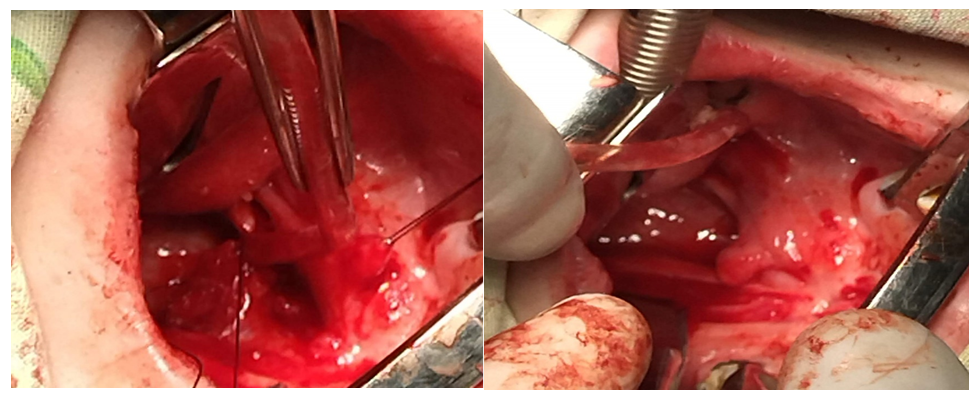 | Figure 4. Muscle-mucous flap when bruised on the back wall of soft palate curtain |
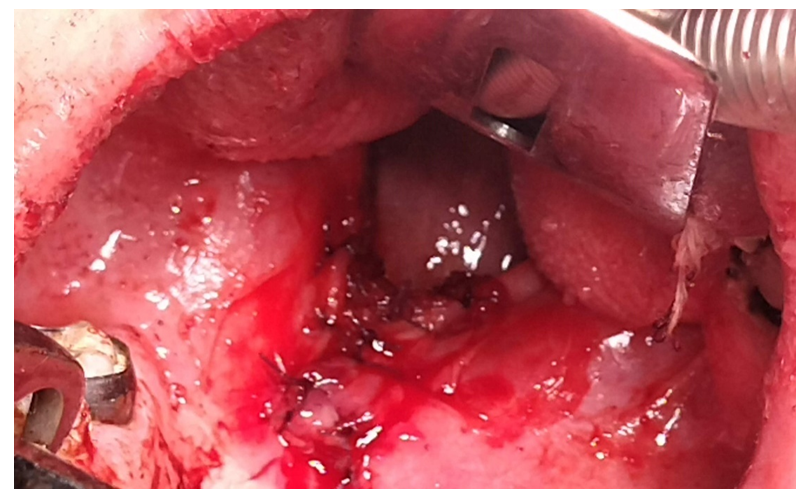
 | Figure 5. Eustachian tubes on the right (a) before (b) after the proposed modification |
 | Figure 6. Indentation of the anterior wall of the soft sky with formation of the tongue of scar-altered mucosa |
3. Conclusions
- Considering that the features of the topographic location of the Eustachian tube after the mobilization of the walls of the pharyngeal walls leads to bending and worsens the emptying of the contents, which leads to local inflammation and pain in patients. In this regard, our proposed modification of uranoplasty eliminates this deficiency, especially in older patients. The developed technique introduced into practice allows early rehabilitation and accelerates the improvement of speech therapy sound correction. Preoperative ENT examinations of a doctor and a speech therapist help to identify groups of children with different perspectives of the correction already being given or planned for individualization of approaches to surgery.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML