-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1800-1804
doi:10.5923/j.ajmms.20251506.34
Received: May 15, 2025; Accepted: Jun. 2, 2025; Published: Jun. 7, 2025

The Place of Colchicine in the Treatment of Chronic Periodontitis in Patients with Coronary Artery Atherosclerosis
Agababyan Irina Rubenovna, Ismoilov Rajabboy Maxmayusuf O’g’li
Samarkand State Medical University, Uzbekistan
Correspondence to: Agababyan Irina Rubenovna, Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of this work was to study the pleiotropic and lipid-lowering effects of colchicine in patients with chronic ischemic heart disease against the background of severe periodontitis. We examined 80 patients with moderate periodontitis against the background of chronic ischemic heart disease (CIHD). Materials and methods: 80 patients with moderate periodontitis on the background of chronic coronary heart disease (HIBS) were examined. The first group included 40 patients with HIBS who underwent a thorough examination and were prescribed basic therapy using double antiplatelet therapy, rosuvastatin at a dose of 10 mg was prescribed on a regular basis, as well as rosuvastatin at a dose of 10 mg in the form of gum applications for 15 minutes for two weeks, then every other day for 3 months. The second group included 40 patients with diagnosed atherosclerosis – corresponding changes on the ECG or after coronary angiography. The following results were obtained: After 6 months of monitoring the indicators of the first and second groups, the differences in them changed even more in favor of the first group, whose patients received rosuvastatin at a dose of 10 mg orally and 10 mg in the form of gum applications under strict control. Almost all blood counts and changes in periodontal tissue once again confirm a decrease in the level of inflammation around the periodontium, a decrease in the level of plaque, the bleeding index, and the depth of the periodontal pocket. The analysis of the obtained data confirms the connection between atherosclerosis of the coronary arteries and chronic periodontitis. Against the background of taking statins, the level of OH, LDL decreases, and the level of HDL increases. Monitoring the intake of statins in elderly patients with moderate periodontitis with its use in the form of applications significantly reduces the level of C-reactive protein, which once again proves the pleiotropic effect of statins in the elderly against the background of chronic periodontitis.
Keywords: Atherosclerosis, Periodontitis, Lipid spectrum, Interleukins
Cite this paper: Agababyan Irina Rubenovna, Ismoilov Rajabboy Maxmayusuf O’g’li, The Place of Colchicine in the Treatment of Chronic Periodontitis in Patients with Coronary Artery Atherosclerosis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1800-1804. doi: 10.5923/j.ajmms.20251506.34.
1. Introduction
- Currently, cardiovascular diseases occupy the first place in the structure of mortality among all diseases in Uzbekistan [4]. The main disease that ultimately leads to disability and mortality is atherosclerosis. First of all, we are talking about atherosclerosis of the coronary arteries - chronic ischemic heart disease (CIHD), atherosclerosis of the cerebral arteries and atherosclerosis of the peripheral arteries. It has already been proven that inflammation plays a decisive role in the occurrence and development of atherosclerosis. Periodontitis is also a common chronic inflammatory disease associated with other chronic inflammatory diseases, such as atherosclerotic cardiovascular diseases. The mechanisms underlying this association are yet to be fully understood. However, periodontitis and its various manifestations, ranging from aggressive to severe loss of up to several teeth at once, especially in patients with atherosclerosis, are also important, given the quality of life of people. Common factors that contribute to the development of both cardiovascular diseases and chronic periodontitis include aging, smoking, alcohol abuse, ethnicity, education and socioeconomic status, male gender, diabetes mellitus and overweight or obesity [1,5]. Periodontitis is a potential risk factor that can initiate the development, maturation and instability of atheromas in the arteries. A mechanism has been proposed to explain this association: periodontal pathogens directly enter the bloodstream and cause inflammation or indirectly by increasing the systemic levels of inflammatory mediators. Our study focuses on the anti-inflammatory effects of colchicine used in the treatment of CIHD and their impact on reducing inflammation in chronic periodontitis.Coronary atherosclerosis and periodontitis, given their prevalence, represent a serious epidemiological problem. Pathophysiological data indicate a possible common inflammatory etiopathogenetic origin of these diseases.Atherosclerosis is a chronic inflammatory process affecting mainly the intima of large and medium-sized arteries, resulting in the formation of lipid deposits due to the accumulation of inflammatory cells and the formation of a fibrolipid structure known as an atherosclerotic plaque [1]. Theories of the pathogenesis of atherosclerosis have changed over time [2,4]. Currently, the role of autoimmune and inflammatory conditions in the onset and development of atherosclerosis and in the development of its complications is emphasized [3]. Endothelial dysfunction, resulting from immune and inflammatory reactions in the vessel wall, is the earliest and most important process in the development of atherosclerosis [10]. Periodontitis is preceded by gum inflammation (gingivitis), which is reversible with appropriate treatment. As a result of periodontal inflammation, the tissues surrounding the tooth are permeated with neutrophils, macrophages and, subsequently, activated lymphocytes, which secrete, for example, interleukin-1, prostaglandin E 2 and tumor necrosis factor-alpha [8]. The large area of periodontal tissue, as well as its dense vascularization, allow bacteria, bacterial metabolic products and inflammatory mediators to enter the bloodstream and thus contribute to endothelial dysfunction [9].It is known that periodontitis itself is an independent risk factor contributing to the development of atherosclerotic vascular disease, and the main mechanism is systemic inflammation [10].Objective: To study the anti-inflammatory effect of colchicine in patients with chronic ischemic heart disease against the background of periodontitis.
2. Material and Methods
- 80 patients with moderate periodontitis associated with chronic ischemic heart disease (CIHD) were examined.The first group included 40 patients with CIHD, who underwent a thorough examination and were prescribed basic therapy using dual antiplatelet therapy, rosuvastatin was prescribed at a dose of 10 mg on a permanent basis, as well as colchicine at a dose of 0.5 mg in tablets once a day for 6 months.The second group included 40 patients with diagnosed atherosclerosis – corresponding changes on the ECG or after coronary angiography, who received basic therapy for coronary heart disease.Inclusion criteria of the research:• Age >45 years;• Atherosclerotic lesion of the coronary arteries (confirmed by coronary angiography);• Availability periodontitis stage II gravity;• Stable symptoms and hemodynamics;• Those who provided informed consent.Exclusion criteria of the research:• patients under 45 years of age,• planned revascularization of an artery related to infarction or stroke more than 120 days after the qualifying/index event;• a recent cardiovascular event was probably an embolism, according to a neurologist or cardiologist;• severe LV dysfunction (LVEF severe valve disease requiring intervention;• decompensated cardiac heart failure;• active infection (e.g. pneumonia, active skin infections and antibiotic use);• chronic diarrhea;• pregnancy;• the patient has a history of clinically significant active liver or kidney disease;• the presence of data on oncological diseases;• patients with traumatic brain injury;• acute myocardial infarction less than 30 days old;• cannot provide informed consent.To verify the diagnosis of moderate periodontitis, the patient was examined by a dentist according to the generally accepted scheme with determination of the gingival sulcus bleeding index (SBI) and periodontal index (PI) according to Russell (1956). The lipid spectrum was assessed in saliva using the FP -910 (M) analyzer from Labsystems (Finland). Studies were conducted on the level of total cholesterol (TC), low-density lipoproteins (LDL), high-density lipoproteins (HDL), and triglycerides (TG). The diagnosis of coronary artery atherosclerosis was made based on the clinical presence or absence of angina confirmed by ECG and echocardiography or after coronary angiography with the presence of stenosis of the main arteries up to 50%.
|
3. Results and Discussion
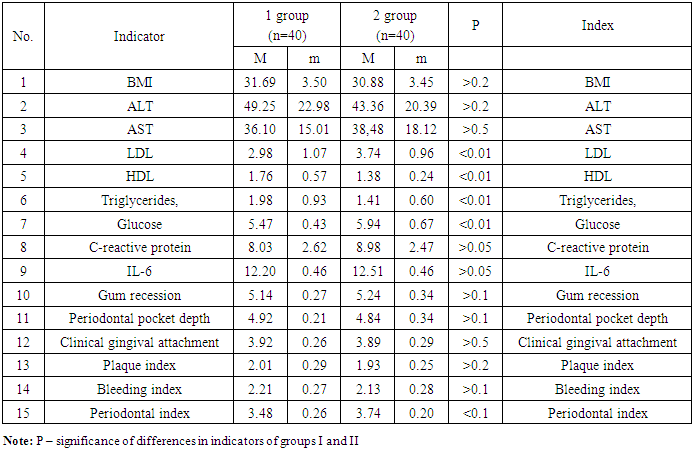
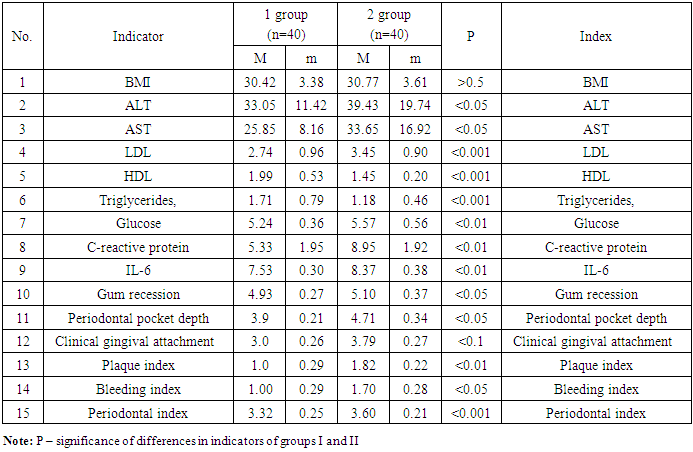
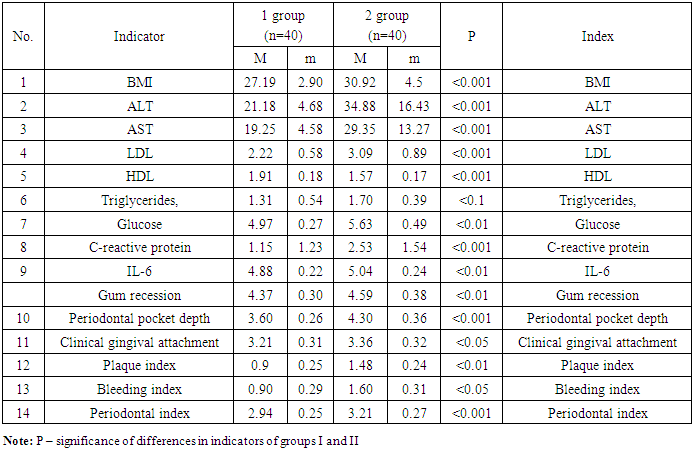
- All patients were relatively the same age, which was 62.0±3.5 years in both groups.
|
|
4. Conclusions
- 1. The analysis of the obtained data confirms the relationship between coronary artery atherosclerosis and chronic periodontitis. 2. When taking colchicine at a dose of 0.5 mg, the level of CRP, IL-6, TNF-a decreases in the studied saliva and blood, and the level of periodontal pocket depth, clinical gingival attachment, plaque index, bleeding index and periodontal index, as well as significant gingival recession, statistically significantly decreases.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML