-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1796-1799
doi:10.5923/j.ajmms.20251506.33
Received: May 7, 2025; Accepted: Jun. 5, 2025; Published: Jun. 7, 2025

Clinical-Immunological Description of Cytomegalovirus Infection in Children
Mukhtorova Shohida Abdulloevna
Assistant, Department of Infectious Diseases and Infectious Diseases of Children, Bukhara State Medical Institute named after Abu Ali ibn Sino, Uzbekistan
Correspondence to: Mukhtorova Shohida Abdulloevna, Assistant, Department of Infectious Diseases and Infectious Diseases of Children, Bukhara State Medical Institute named after Abu Ali ibn Sino, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Cytomegalovirus (CMV) infection is a widespread viral illness affecting children, with particularly severe outcomes in neonates and immunocompromised individuals. The infection may present asymptomatically or with diverse clinical manifestations depending on the child’s immune status. This study provides a descriptive analysis of the clinical symptoms and immunological responses in CMV-infected children, highlighting diagnostic approaches and treatment strategies. Key immunological markers, including T-cell subpopulations, NK cells, and cytokine profiles, are discussed to better understand the host response. The findings suggest that immune profiling may serve as a supportive tool in the management of pediatric CMV infection.
Keywords: Cytomegalovirus, CMV, Children, Congenital infection, Immunology, T lymphocytes, Cytokines, NK cells, Viral diagnosis, Pediatric infection
Cite this paper: Mukhtorova Shohida Abdulloevna, Clinical-Immunological Description of Cytomegalovirus Infection in Children, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1796-1799. doi: 10.5923/j.ajmms.20251506.33.
Article Outline
1. Introduction
- Cytomegalovirus (CMV) is a DNA virus belonging to the Herpesviridae family and is recognized as one of the most common viral infections in the pediatric population [1,2,3]. It is estimated that 0.2% to 2.5% of all live births worldwide are affected by congenital CMV infection, making it the leading non-genetic cause of sensorineural hearing loss and neurodevelopmental delays in children [4,5]. CMV is transmitted through various body fluids including saliva, urine, blood, breast milk, and genital secretions. The infection can be acquired in utero (congenital), during birth (perinatal), or after birth (postnatal), depending on the mode of transmission and the timing of exposure [6,7,8,9].In immunocompetent children, CMV infection is often asymptomatic or presents as a mild febrile illness with symptoms similar to infectious mononucleosis [10,11,12]. However, in newborns, particularly those infected in utero, CMV can lead to severe complications such as microcephaly, intracranial calcifications, chorioretinitis, hepatosplenomegaly, jaundice, and thrombocytopenia [13,14,15]. The risk is significantly higher if the mother acquires a primary CMV infection during pregnancy, especially in the first trimester. In immunocompromised children, such as those undergoing chemotherapy, organ transplantation, or with HIV infection, CMV can cause life-threatening systemic disease involving the lungs, liver, gastrointestinal tract, and central nervous system [16].The immune system plays a critical role in the control and outcome of CMV infection [17,18,19]. Both innate and adaptive immune responses are activated upon infection. Natural killer (NK) cells and cytotoxic CD8+ T lymphocytes are particularly important for viral clearance and long-term immune surveillance. The virus has evolved multiple mechanisms to evade immune recognition, including downregulation of MHC class I molecules and modulation of cytokine signaling, which contributes to its persistence and latency [20]. Changes in cytokine profiles, such as elevated levels of Interleukin-4 (IL-4), Interleukin-10 (IL-10), and Interleukin-17A (IL-17A), reflect immune activation and regulation during infection. These immunological alterations can also be used as biomarkers to assess disease severity and guide treatment decisions [21,22,23].Despite its high prevalence and potential for causing serious long-term consequences, CMV infection remains underdiagnosed in many healthcare settings due to its often-nonspecific presentation [24,25]. Timely diagnosis using serological testing, PCR, and immune cell profiling can significantly improve the management of CMV-infected children. Moreover, a better understanding of the immunopathogenesis of CMV may support the development of targeted therapies and effective vaccines in the future [26,27].
2. Purpose of the Research
- Our aim of the study is clinical-immunological description of cytomegalovirus infection in children.
3. Material and Methods
- This descriptive clinical-immunological study was conducted at the Bukhara Infectious Diseases Hospital between 2022 and 2024. A total of 120 pediatric patients aged from birth to 14 years, diagnosed with cytomegalovirus (CMV) infection, were included in the study. The diagnosis was confirmed using a combination of clinical signs and laboratory investigations, including the detection of CMV-specific IgM and IgG antibodies by enzyme-linked immunosorbent assay (ELISA), as well as polymerase chain reaction (PCR) testing for CMV DNA in blood and/or urine samples [28].Patients were categorized into three groups based on age and infection type: Group I included 40 children with congenital CMV infection diagnosed within the first month of life, Group II included 45 immunocompetent children with acquired CMV infection, and Group III included 35 immunocompromised children (those undergoing chemotherapy, post-transplantation, or with chronic diseases). Detailed clinical evaluation, including history, physical examination, and assessment of symptoms such as fever, rash, hepatosplenomegaly, jaundice, neurological signs, and hearing impairment, was performed.Immunological assessment was carried out by analyzing peripheral blood samples. Flow cytometry was used to quantify lymphocyte subsets, including CD3+, CD4+, CD8+ T cells, CD16+/CD56+ natural killer (NK) cells, and CD20+ B cells. Cytokine levels (IL-2, IL-4, IL-10, and IL-17A) were measured using commercially available ELISA kits. The CD4/CD8 ratio and changes in NK cell counts were used as indicators of immune response patterns. All data were statistically processed using SPSS software version 26.0. Differences between groups were considered statistically significant at p < 0.05.The study protocol was approved by the local ethics committee of the Bukhara Infectious Diseases Hospital, and informed consent was obtained from the parents or legal guardians of all participants.
4. Results
- Among the 120 pediatric patients with cytomegalovirus infection observed at the Bukhara Infectious Diseases Hospital, clinical and immunological findings varied according to age, infection type, and immune status.In Group I (congenital CMV, n = 40), the most common clinical features included hepatosplenomegaly (75%), prolonged jaundice (60%), microcephaly (35%), petechial rash (30%), and neurological abnormalities such as hypotonia and delayed motor reflexes (25%). Sensorineural hearing loss was confirmed in 5 cases (12.5%). In most cases, these infants showed signs of intrauterine growth retardation.In Group II (acquired CMV in immunocompetent children, n = 45), clinical presentation was relatively mild. The majority of children exhibited fever (78%), cervical lymphadenopathy (60%), fatigue (51%), and mild hepatomegaly (40%). These cases resembled mononucleosis-like syndrome and resolved without significant complications.Group III (immunocompromised children, n = 35) demonstrated more severe manifestations. CMV-associated pneumonia occurred in 11 cases (31%), gastrointestinal involvement in 9 cases (26%), and hepatitis in 8 cases (23%). Two children developed CMV retinitis. The disease course was prolonged and required antiviral treatment in most cases.
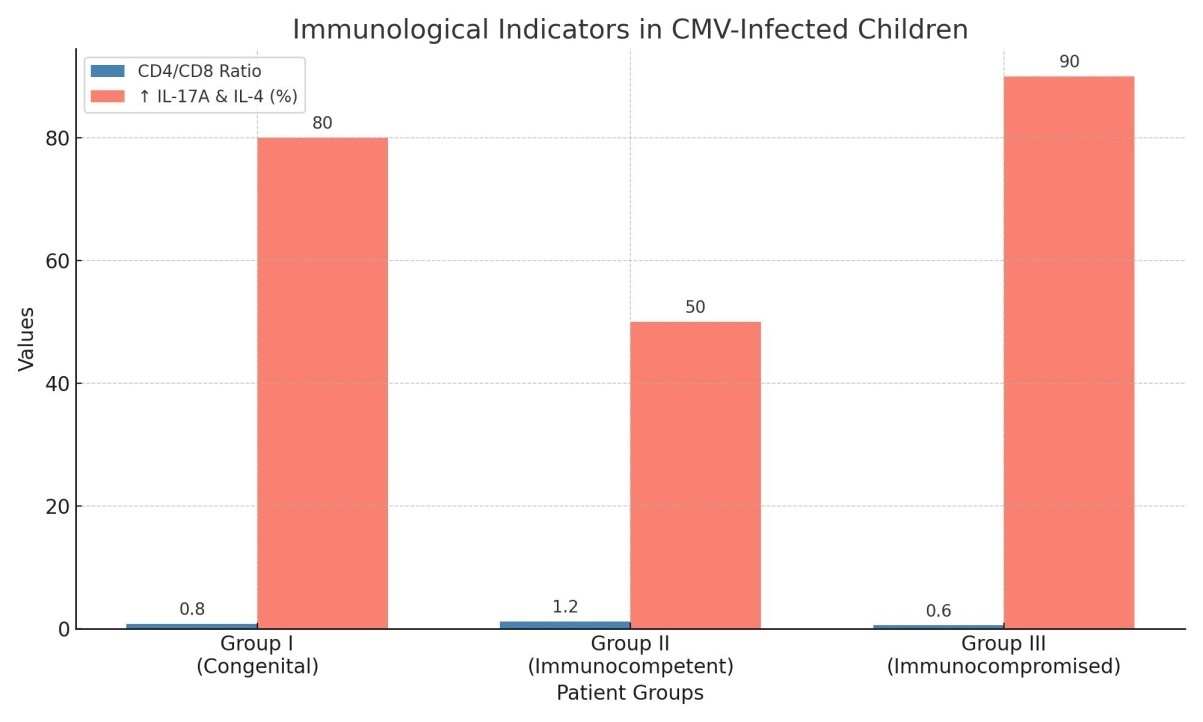 | Picture 1. The CD4/CD8 ratio and IL-17A and IL-4 elevation (%) in each group are shown |
5. Discussion
- The findings support the notion that CMV infection in children exhibits variable clinical features depending on immune status. Congenital infections tend to result in more permanent damage due to intrauterine exposure, while postnatal infections are typically mild unless the immune system is compromised. The immunological data demonstrate that both cellular and humoral responses are involved in disease progression and resolution. The elevated CD8+ T cell and NK cell activity reflects a strong antiviral response, whereas altered cytokine profiles may contribute to inflammation and tissue damage. Early identification of immunological imbalances can be useful in predicting disease severity and guiding therapy.
6. Conclusions
- Cytomegalovirus infection in children presents with a broad spectrum of clinical and immunological manifestations depending on the age of the patient and the status of their immune system. Congenital CMV infection is associated with severe systemic complications, including neurological and developmental impairments, and demonstrates significant immune dysregulation, particularly with a decreased CD4/CD8 ratio and elevated pro-inflammatory cytokines such as IL-4 and IL-17A. In contrast, immunocompetent children generally exhibit milder symptoms with transient immunological shifts, while immunocompromised patients experience more severe and prolonged disease courses, marked by pronounced immune suppression and cytokine imbalance.These findings highlight the importance of early and accurate diagnosis of CMV infection in pediatric populations, especially in high-risk groups such as neonates and immunocompromised children. Immunological markers such as T-cell subset distribution and cytokine levels may serve as valuable tools for assessing disease severity and guiding therapy. A comprehensive understanding of these immune responses is essential for improving clinical outcomes, optimizing antiviral treatment strategies, and informing vaccine development efforts aimed at controlling CMV infection in children.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML