-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1786-1790
doi:10.5923/j.ajmms.20251506.31
Received: May 2, 2025; Accepted: Jun. 1, 2025; Published: Jun. 7, 2025

Specificity of Hemorrhagic Stroke with Different Underlying Diseases and Prediction of Cerebral Hemorrhage in Diabetes Mellitus
Akbaralieva Sayyora, Ataniyazov Maksud, Rakhimbaeva Gulnora
Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Akbaralieva Sayyora, Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article presents the specificity of blood coagulation parameters such as hematocrit, thrombin time, fibrinogen, etalon test, thrombotest in hemorrhagic stroke and type 2 diabetes mellitus, and the dependence of these values on various comorbidities and the age and gender of patients. Hemorrhagic stroke, especially the parenchymal type, is a common and urgent medical and social problem. Cardiovascular and endocrine diseases are increasing the frequency of hemorrhagic stroke as a background and their effect on the walls of blood vessels and the rheological properties of blood is known. As a result, patients have varying degrees of neurological disorders and premature death.
Keywords: Hemorrhagic stroke, Coagulogram, Diabetes mellitus, Hypertension
Cite this paper: Akbaralieva Sayyora, Ataniyazov Maksud, Rakhimbaeva Gulnora, Specificity of Hemorrhagic Stroke with Different Underlying Diseases and Prediction of Cerebral Hemorrhage in Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1786-1790. doi: 10.5923/j.ajmms.20251506.31.
Article Outline
1. Introduction
- Relevance of the problem: Acute disruption of blood circulation in the brain is called a stroke. Ischemic, hemorrhagic, and mixed strokes are distinguished. Ischemic stroke is a clinical syndrome caused by a sharp decrease or cessation of blood circulation in a certain part of the brain, the symptoms of which are detected for more than 24 hours [1,2]. Hemorrhagic stroke occurs due to rupture of pathologically altered blood vessels or penetration of blood from the brittle vessel wall into brain tissue (perdiapedesis) [1,2]. Depending on the localization of the focus of stroke development, patients experience various motor and mental disorders. In most patients, disorders of speech (aphasia, dysarthria), writing (agraphia), reading (alexia), calculation (calculus), thinking, motor sphere (paresis, apraxia), perception (agnosia), attention, and emotional (depression, apathy) are observed [6]. Diabetes mellitus increases the likelihood of stroke development by 3-4 times and worsens the outcome [3]. It also plays a key role in the development of hypertension, cerebral and vascular atherosclerosis. Diabetes mellitus, cerebral micro-, macroangiopathies, dysmetabolic syndrome, frequent hypo- and hyperglycemic changes in the blood, as well as arterial hypertension, aneurysms sharply increase the risk of hemorrhagic stroke. It is known that hemorrhagic stroke is a disease that is less common than other strokes, but is more common in middle-aged people with high rates of disability, a sharp decline in life activity, and mortality [7]. As a result of numerous laboratory and instrumental studies, the levels of biomarkers such as neuron-specific enolase (NSE), S-100 protein, glial neurotrophic factor (GNTF), vascular endothelial growth factor (VEGF), and superoxide dismutase change in the blood during the acute and very acute stages of hemorrhagic stroke. (A.M. Golubev, A.V. Grechko, M.A. Govorukhina, V.E. Zakharchenko, A.N. Kuzovlev, M.V. Petrova. Molecular markers of hemorrhagic stroke. General Resuscitation. 2020), which is important in assessing the effectiveness of diagnosis and treatment of hemorrhagic stroke. Despite the fact that neuroimaging and biochemical blood tests are currently sufficient for the diagnosis of hemorrhagic stroke, our studies have proven that the course of hemorrhagic stroke is more severe in patients with type 2 diabetes mellitus, especially acute, acute, early and late recovery periods after stroke, prognosis, and mortality. Nevertheless, effective methods of treatment and positive rehabilitation of patients with type 2 diabetes mellitus with hemorrhagic stroke, which have not been fully resolved, still remain a mystery.Purpose of the study: to study the features of blood coagulation system parameters in hemorrhagic stroke observed in patients with a different comorbid background and to predict the probability of hemorrhagic stroke in patients with type 2 diabetes mellitus in the compensation and subcompensation periods using the HEMORR2HAGE scale. Study of the correlation between the results of thrombotest, fibrinogen, hematocrit tests and the results of the Rankin and Scandinavian scales in patients with hemorrhagic stroke.
2. Main Body
2.1. Materials and Methods of Research
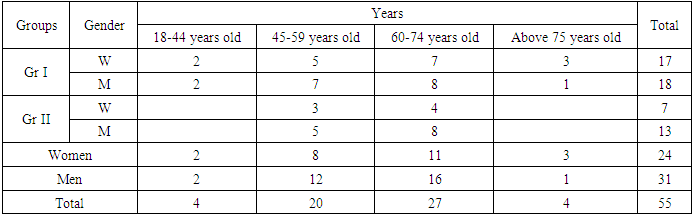
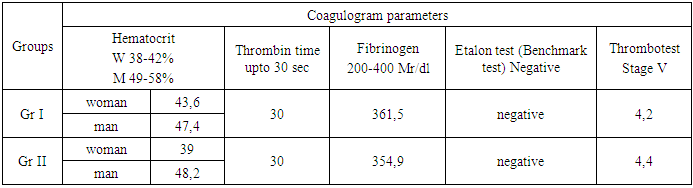
- 55 patients with hemorrhagic stroke and 50 patients with type 2 diabetes mellitus in the period of compensation and subcompensation in the departments of intensive neurology, neurology and therapeutic resuscitation and endocrinology of the multidisciplinary clinic of the Tashkent Medical Academy in 2023-2024 were taken as research material. 35 patients with hemorrhagic stroke formed on the basis of hypertension and atherosclerosis made up group I, and 20 patients with hemorrhagic stroke developed on the basis of hypertension and type 2 diabetes mellitus made up group II. Of the 50 patients with type 2 diabetes mellitus, 17 were in the compensation period, and the remaining 33 were in the subcompensation period. In these patients, the clinical course of the disease, the results of MSCT, MRI, and MRI of the brain, as well as coagulogram parameters, namely hematocrit count, thrombin time, fibrinogen, reference test, thrombotest, were analyzed. Also, the degree of disability of patients in groups I and II was assessed according to the Scandinavian scale, and the severity of the stroke according to the Rankine scale. The correlation between the fibrinogen and Rankine scales, hematocrit and Scandinavian scale values was analyzed.The correlation between the fibrinogen and Rankine scales, hematocrit and Scandinavian scale values was analyzed. The strength of the correlation between the Rankine and Scandinavian scales was analyzed. The risk of hemorrhagic stroke in patients with type 2 diabetes mellitus was assessed using the HEMORR2HAGE scale.
2.2. Discussion and Results
- Among the 35 patients in the study group I, 48.6% (n=17) were women and 51.4% (n=18) were men, and the age of patients in this group was divided into 4 groups according to WHO criteria, that is, the number of patients aged 18-44 years was 4 (11.4%), 45-59 years - 12 (34.3%), 60-74 years - 15 (42.9%), and over 75 years - 4 (11.4%). Among 20 patients in group II, 35% (n=7) were women and 65% (n=13) were men, among these patients 8 (40%) were 45-59 years old, 12 (60%) were 59-74 years old (Table 1).
|
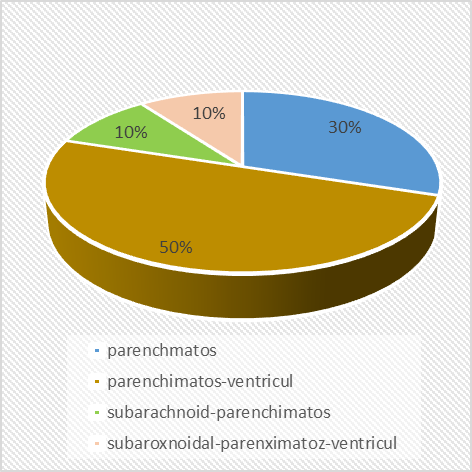
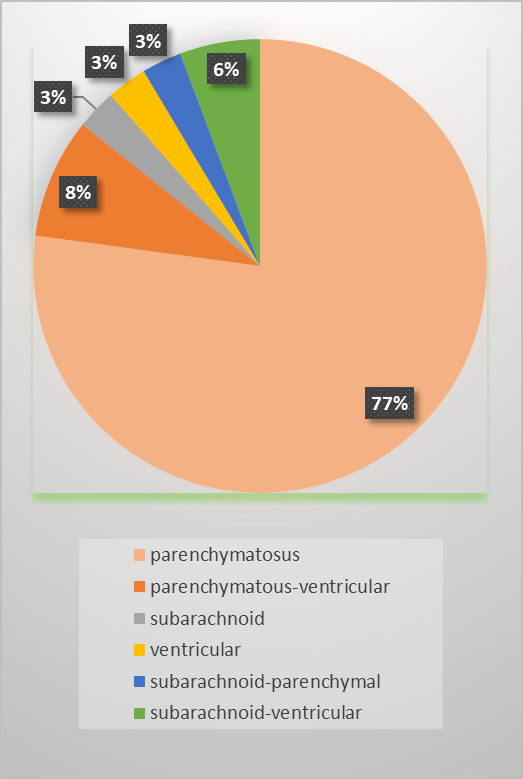 | Figure 1. Types of hemorrhagic stroke group I |
 | Figure 2. Types of hemorrhagic stroke of group II |
|
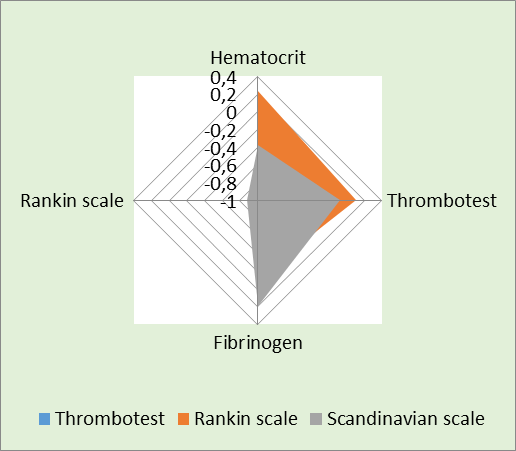 | Figure 3. Correlation analysis between blood clotting indicators of group I and Rankin, Scandinavian scales |
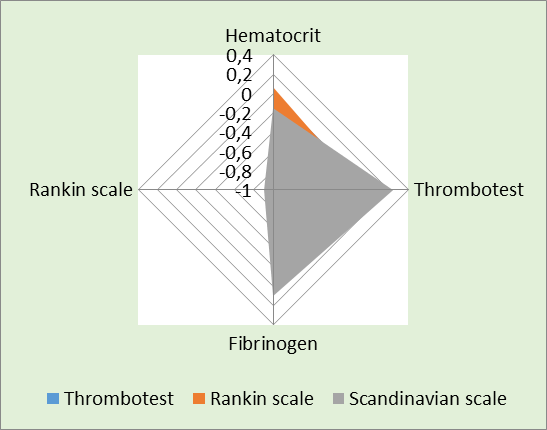 | Figure 4. Correlation analysis between blood clotting indicators of group II and Rankin, Scandinavian scales |
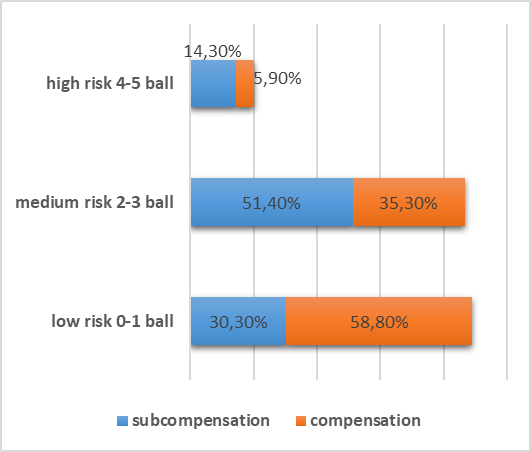 | Figure 5. Analysis of the HEMORR2HAGES scale in type 2 diabetes mellitus |
3. Conclusions
- 1. When analyzing the clinical course of hemorrhagic stroke in the groups, it was revealed that the parenchymal type of hemorrhagic stroke prevailed mainly in patients with a comorbid background of hypertension and cerebral atherosclerosis (77.1%), and in hemorrhagic stroke developed in type 2 diabetes mellitus, the parenchymal-ventricular type prevailed (50%). Nevertheless, mixed and severe forms of hemorrhagic stroke, namely parenchymatous-ventricular, subarachnoid-parenchymatous-ventricular types, accounted for a larger proportion (60%) in patients of group II.2. According to the results of the study, the specificity of the indicators of the reference test and thrombin time in patients with various comorbid background diseases in groups I and II did not differ.3. When predicting the probability of developing hemorrhagic stroke using the HEMORR2HAGES scale in patients with type 2 diabetes mellitus, the severity of the disease increases the risk of hemorrhagic stroke.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML