-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1772-1775
doi:10.5923/j.ajmms.20251506.28
Received: Apr. 30, 2025; Accepted: Jun. 3, 2025; Published: Jun. 7, 2025

A Pharmacoepidemiological Analysis of Antibiotic Therapy in Patients with Chronic Pyelonephritis was Conducted in Some Hospitals in the Khorezm Region
Akhmedova Nazakat Marimbayevna1, Ismoilov Soloy Ruzmamatovich2, Bekchanova Yulduzkhan Khayitbayevna3
1Assistant, Department of Pharmacology and Clinical Pharmacology, Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan
2Associate Professor, Department of Pharmacology and Clinical Pharmacology, Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan
3PhD, Department of Pharmacology and Clinical Pharmacology, Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan
Correspondence to: Akhmedova Nazakat Marimbayevna, Assistant, Department of Pharmacology and Clinical Pharmacology, Urgench Branch of the Tashkent Medical Academy, Urgench, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

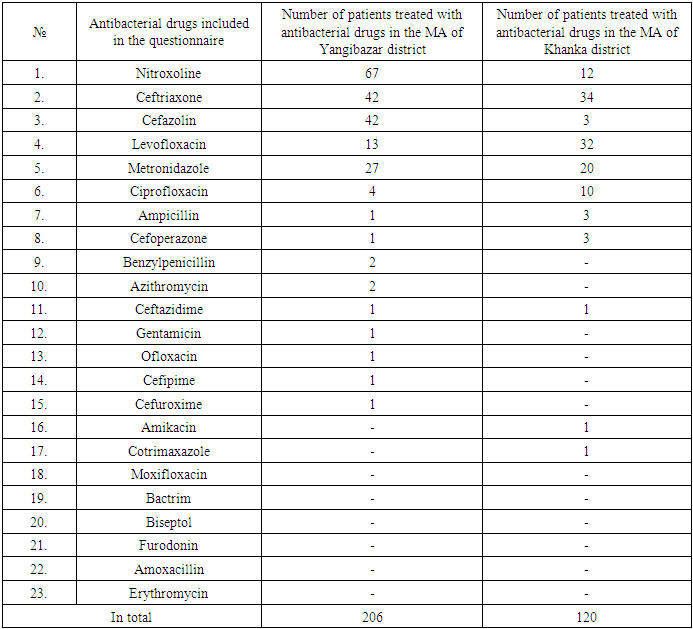
In the course of the study, the case histories of 230 patients treated for chronic pyelonephritis in some hospitals of Khorezm region, namely 128 patients in the Medical Association (MA) of Yangibazar district and 102 patients in the MA of Khanka district, were studied retrospectively using pharmacoepidemiological methods. The pharmacoepidemiological analysis focused on the use, efficacy and safety of antibacterial agents alone or in appropriate combinations. All data were statistically analysed. According to the data obtained, only 13 out of more than 20 antibacterial drugs studied were used in the MA of Yangibazar district, 11 drugs were used in the MA of Khanka district, and the remaining drugs were not used at all in the patients studied. Antibacterial drugs used for treatment of chronic pyelonephritis in these hospitals do not fully comply with the national clinical protocol recommended by nephrologists of Uzbekistan.
Keywords: Chronic pyelonephritis, Pharmacoepidemiology, Antibacterial drugs
Cite this paper: Akhmedova Nazakat Marimbayevna, Ismoilov Soloy Ruzmamatovich, Bekchanova Yulduzkhan Khayitbayevna, A Pharmacoepidemiological Analysis of Antibiotic Therapy in Patients with Chronic Pyelonephritis was Conducted in Some Hospitals in the Khorezm Region, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1772-1775. doi: 10.5923/j.ajmms.20251506.28.
Article Outline
1. Introduction
- Chronic pyelonephritis is a long-term infectious and inflammatory process of the kidneys in which the renal parenchyma and the pelvis are affected simultaneously or sequentially, and is the second most common inflammatory disease of the urogenital tract after acute respiratory viral infections, accounting for up to 65% of all inflammatory diseases of the urogenital tract. [1,4,5] There is a marked gender difference in the incidence rate - women are more likely to be affected (3-5 times more often). This fact is explained by the peculiarities of the anatomy of the female urinary system: short urethra, which facilitates the invasion of microorganisms into the urinary system. [6,7]The World Health Organisation classifies pyelonephritis as a problem of social importance, as the disease occurs more frequently in people of working age and is often disabling. [4,5] The most important aetiological factor provoking the development of chronic pyelonephritis is bacterial flora and is the second most common reason for prescribing antibiotics after acute respiratory infections. [7] Chronic pyelonephritis is caused both by a single type of microorganism and by microbial associations, when several types of microorganisms are simultaneously isolated during bacteriological examination and the use of antibacterial agents is an obligatory component of therapy, and their rational use contributes to the elimination or reduction of the microbial inflammatory process in the kidney tissue and urinary tract, reduces the likelihood of damage to the kidney parenchyma, and prevents the growth of antibiotic-resistant pathogens, which is an important factor in the development of chronic pyelonephritis. [8] According to current recommendations, the choice of an initial antibiotic should be based not only on local data from microbiological studies, but also on the therapeutic efficacy and safety of different antibacterial agents. [2,3]
2. Purpose of the Research
- The purpose of this pharmacoepidemiological study is to analyze and evaluate the patterns of antibiotic therapy in patients with chronic pyelonephritis across selected hospitals in the Khorezm region. Specifically, the research aims to assess Prescription Practices – Examine the types, frequency, and duration of antibiotics prescribed for chronic pyelonephritis to understand current treatment trends.By conducting this analysis, the study seeks to contribute to better clinical practices, promote antimicrobial stewardship, and ultimately improve the management of chronic pyelonephritis in the region.The aim of this research is to study the pharmacoepidemiology of antibacterial drugs in patients treated for chronic pyelonephritis in some hospitals of Khorezm region.
3. Materials and Methods
- Clinical studies were conducted on the basis of medical records of patients with chronic pyelonephritis who were treated as inpatients in the medical associations of Yangibazar and Khanka districts of Khorezm region. Using pharmacoepidemiological methods based on a specially designed questionnaire, the case histories of 230 patients treated in the period 2019-2024 from the archives of these MAs of Khorezm region were retrospectively analysed.The following data were collected during the review of the patients' case histories Full name, age and sex of the patients, duration of the disease, frequency of exacerbations and presence of complications of the disease, nature, efficacy, combination and compliance with national clinical standards of treatment of the drugs used in these patients.
4. Results and Discussion
- Based on the results of the study, we can say that according to the gender distribution of 128 patients treated in the MA of Yangibazar district 60% (77) were women and 40% (51) were men, and in 102 patients treated in the MA of Khanka district 75% (76) were women and 25% (26) were men. On this basis, the picture for the MAs studied in both districts is as follows: women account for 67% (153) and men for 33% (77). At the same time, a high incidence of morbidity was observed in women, which is in line with literature data (Figure 1).
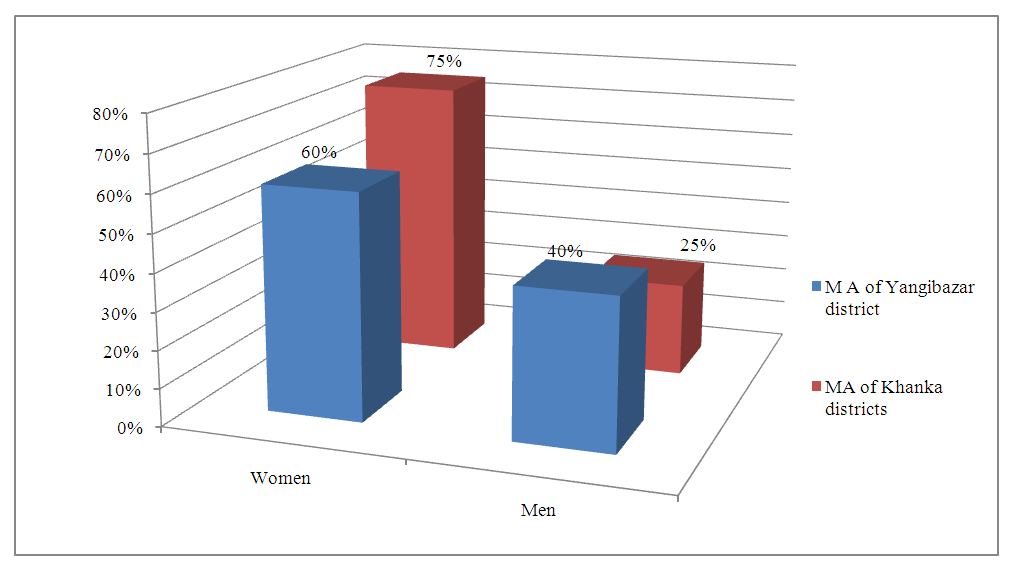 | Figure 1. Gender distribution of patients |
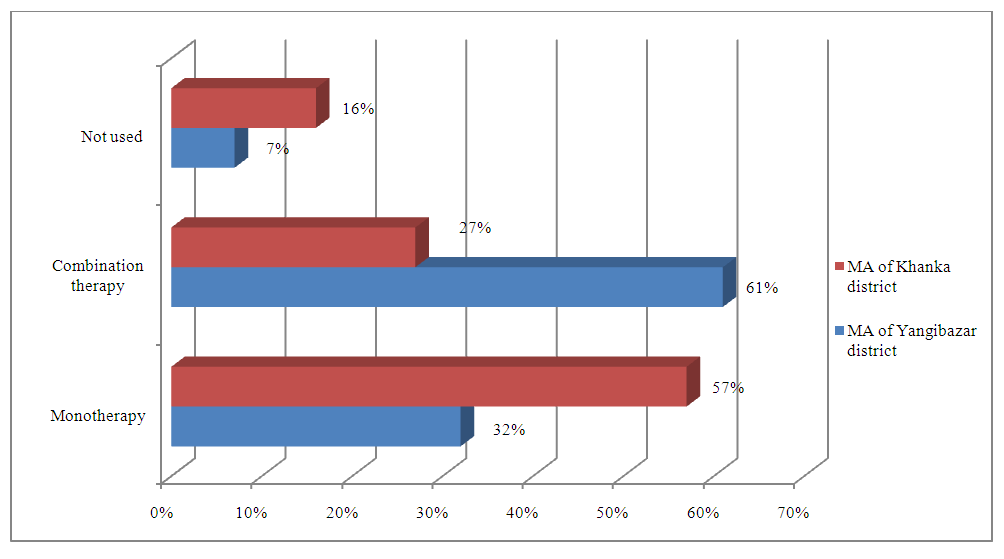 | Figure 2. Types of antibacterial drug use therapy |
|
5. Conclusions
- The incidence of chronic pyelonephritis among women in the MAs of Yangibazor and Khanka districts of Khorezm region is high, which is consistent with literature data. Antibacterial agents were used as monotherapy and in combination in the treatment of chronic pyelonephritis. The antibacterial drugs used for the treatment of chronic pyelonephritis in the MAs of Yangibazor and Khanka districts of Khorezm region do not fully comply with the national clinical protocol recommended by nephrologists in Uzbekistan. This pharmacoepidemiological study on antibiotic therapy in patients with chronic pyelonephritis in selected hospitals of the Khorezm region provided valuable insights into current prescribing practices, adherence to clinical guidelines, and potential areas for improvement. The findings revealed the most commonly used antibiotics, their dosage regimens, and treatment durations, highlighting both appropriate practices and deviations from recommended protocols.Key observations included possible instances of antibiotic overuse, misuse, or suboptimal selection, which could contribute to the risk of antimicrobial resistance (AMR) and reduced treatment efficacy. The study underscores the need for enhanced adherence to evidence-based guidelines, continuous medical education for healthcare providers, and the implementation of antimicrobial stewardship programs in the region.By optimizing antibiotic prescribing patterns, healthcare professionals can improve patient outcomes, minimize adverse effects, and combat the growing threat of antibiotic resistance. Future research should include larger, multicenter studies and longitudinal assessments to monitor the long-term impact of antibiotic therapy in chronic pyelonephritis management.Ultimately, this study serves as a foundation for policymakers and clinicians to refine treatment strategies, ensuring safer and more effective care for patients with chronic pyelonephritis in the Khorezm region and beyond.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML