-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1767-1771
doi:10.5923/j.ajmms.20251506.27
Received: Apr. 30, 2025; Accepted: Jun. 2, 2025; Published: Jun. 7, 2025

Characteristics of Anthropometric Indicators in Children with Abdominal Obesity Complicated by Metabolic Syndrome
Garifulina Lilia Maratovna, Islamova Dilbar Sadykovna, Ashurova Maksuda Jamshedovna, Goyibova Nargiza Salimovna
Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: Garifulina Lilia Maratovna, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Relevance of the study. The degree of obesity, the age of onset of obesity, and the type of distribution of adipose tissue in the child's body are of great importance in the development of metabolic syndrome in children. Objective of the study: to conduct a comparative characteristic of anthropometric indicators in children with different types of obesity and metabolic syndrome. Material and methods: 211 children with primary exogenous constitutional obesity, aged 7 to 18 years, anthropometric methods used. A set of anthropometric studies was conducted. Results of the study: in boys aged 7-9 years with abdominal obesity, the body mass index and waist-to-hip ratio exceeded the indicators of girls and approached the anthropometric indicators of older children. The dependence of anthropometric indicators on the presence of metabolic syndrome components was noted. Conclusion: obese boys aged 7-9 years had anthropometric indicators corresponding to severe obesity. The waist-to-hip ratio characterizing abdominal obesity was highest in children with complete metabolic syndrome, and increased depending on the number of metabolic syndrome components. Conclusion: boys with obesity aged 7-9 years had anthropometric indicators corresponding to severe obesity. The waist-to-hip ratio characterizing abdominal obesity was highest in children with complete metabolic syndrome, and increased depending on the number of metabolic syndrome components.
Keywords: Obesity, Children, Anthropometry, Metabolic syndrome
Cite this paper: Garifulina Lilia Maratovna, Islamova Dilbar Sadykovna, Ashurova Maksuda Jamshedovna, Goyibova Nargiza Salimovna, Characteristics of Anthropometric Indicators in Children with Abdominal Obesity Complicated by Metabolic Syndrome, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1767-1771. doi: 10.5923/j.ajmms.20251506.27.
1. Introduction
- Childhood obesity is currently a global problem. The World Health Organization's European Childhood Obesity Surveillance Initiative (COSI) shows that "...29% of children aged 7–9 years are overweight and obese, with a higher prevalence of pathology in boys (31%) compared to girls (28%)..." [1]. The relevance of the problem of obesity is that this pathology is associated with the development of metabolic syndrome (MS), one of the most acute medical and social problems of the modern healthcare system [2,3].Abdominal obesity is an important component of metabolic syndrome, and if previously it was believed that MS is a problem of middle-aged people, then in the last decade its steady growth has been observed among children. Thus, the prevalence of MS among adolescents with obesity is 26–49% [4].The degree of obesity, the age of onset of obesity, and the type of distribution of adipose tissue in the child’s body are of great importance [4,5], in connection with this, the aim of the study was set: to conduct a comparative analysis of anthropometric indicators in children with different types of obesity and metabolic syndrome.
2. Material and Methods
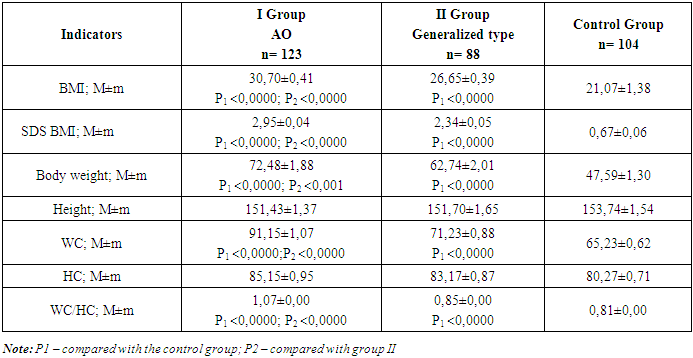
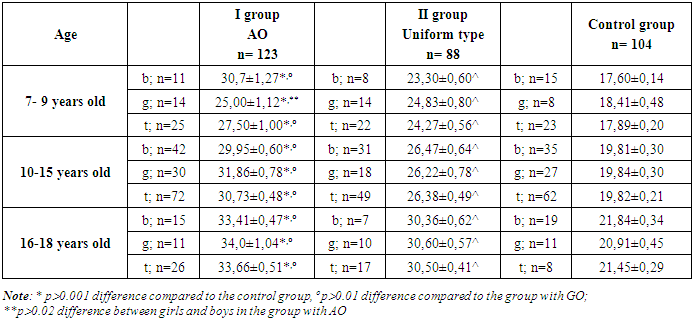
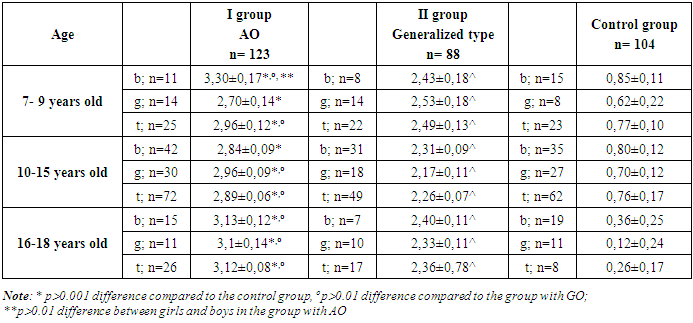
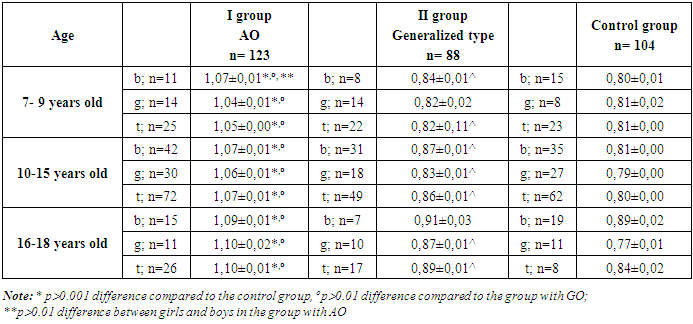
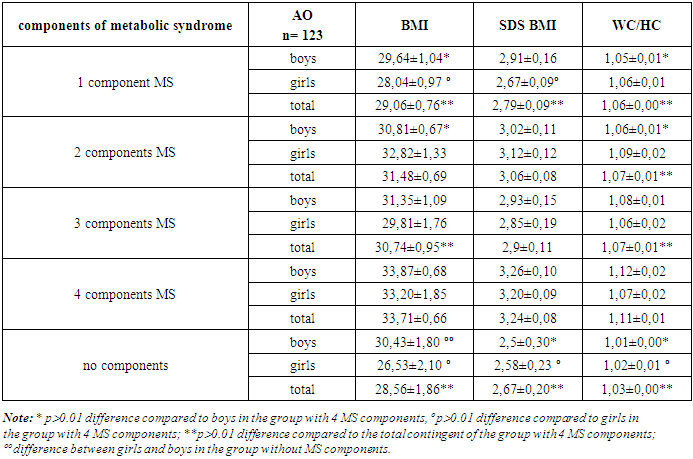
- We examined 211 children with primary exogenous constitutional obesity, aged from 7 to 18 years (12.29±0.28 years), of which 114 were boys (54.0%) and 97 girls (46.0%), as well as 104 children with normal body weight of similar age composition (12.36±0.31 years), with the distribution of boys 61 (58.6%) and girls 43 (41.3%).The diagnosis of obesity was made based on WHO recommendations; the standard deviation (SD) of the body mass index (BMI) was calculated taking into account the sex and age of the children [6].In accordance with the aim of the study, we formed the following groups: Group I - 123 children with abdominal obesity (visceral obesity, complicated obesity) with a waist circumference (WC) over the 90th percentile for the corresponding age and gender (BMI 30.61±0.83 kg/m2). Group II consisted of 88 children with a uniform type of obesity (simple obesity) with a WC below the 90th percentile, respectively, for age and gender (BMI 25.96±0.45).An anthropometric examination of children was conducted to determine BMI, WC, hip circumference (HC), and the WC/HC ratio.Waist circumference (WC) was assessed according to percentile tables provided in the National Clinical Guidelines of the All-Russian Scientific Society of Cardiologists (ASS C Moscow 2009) [7]. Obesity was considered abdominal when WC was ≥90 percentile and above. The criterion for abdominal obesity in adolescents over 16 years old was WC≥80 cm in girls and WC≥94 cm in boys. The hip circumference (HC) was determined, as well as the WC to HC ratio (WHR - Waist-hip ratio) determined by dividing the waist circumference by the hip circumference. Normally, this ratio should be no more than 0.85 for girls, and 0.9 for boys (WHO).The diagnosis of metabolic syndrome was made based on the diagnostic criteria for MS in children and adolescents developed by the International Diabetes Federation (IDF).The results of the study of children with abdominal obesity showed that complete metabolic syndrome with a combination of Abdominal Obesity (AO) and 4 signs was observed in 20 children (16.2%), 3 components in 23 (18.7%) children with abdominal obesity, in combination of AO with 2 components occurred in almost 1/4 of children in the AO group (32 children - 26.0). The frequency of occurrence of 1 component of MS in children with AO was 1/3 of cases (39 children - 31.7%).Statistical processing of the obtained data was carried out on a personal computer using the Statistica 10 program. Methods of variational parametric and nonparametric statistics were used with the determination of the arithmetic mean (M), standard deviation (σ), standard error of the mean (m), and relative values (frequency, %). The statistical significance of the obtained measurements was determined using the Student criterion (t) with the calculation of the probability of error (P).
3. Results of the Study
- In accordance with the stated objective, we analyzed the anthropometric characteristics of children with abdominal obesity with manifestations of metabolic syndrome. The main characteristics depending on the type of distribution of adipose tissue are presented in Table 1.
|
|
|
|
|
4. Conclusions
- In boys aged 7-9 years with abdominal obesity, BMI and WC/HC ratio statistically exceeded the indicators of girls and approached the BMI and WC/HC ratio of senior school-age children, and also statistically exceeded the BMI and WC/HC ratio of boys with uniform obesity, which indicates a significant accumulation of body weight in boys with abdominal obesity even in primary school age and serves as a risk factor for the occurrence and progression of MS in children.The obtained data characterize the presence of a dependence of BMI and SDS BMI on the components of MS, while the anthropometric indicators in children with complete and incomplete variants were statistically different from the indicators of children with AO +1 component and with the absence of MS components, while the WC/HC indicator clearly depended on the number of MS components, having the greatest results in children with the complete variant of MS. Information about the source of support in the form of grants, equipment, and drugs. The authors did not receive financial support from manufacturers of medicines and medical equipment.Conflicts of interest. The authors have no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML