-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1737-1739
doi:10.5923/j.ajmms.20251506.22
Received: May 2, 2025; Accepted: May 25, 2025; Published: Jun. 5, 2025

Subclinical Hypothyroidism as a Predictor of Gestational Diabetes
Nasirova Shaxlo Shukhratovna
Bukhara State Medical Institute named after Abu Ali ibn Sina, Bukhara, Uzbekistan
Correspondence to: Nasirova Shaxlo Shukhratovna, Bukhara State Medical Institute named after Abu Ali ibn Sina, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

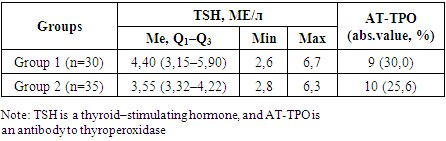
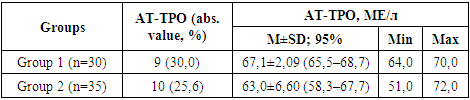
It is currently projected that 1 in 3 adults in the United States (USA) will have diabetes by 2025. The growing prevalence of type 2 diabetes is increasing significantly among adults, especially among young women of reproductive age who are diagnosed with this disease during pregnancy. The study is a prospective follow-up of 109 pregnant women since the detection of GDM. The diagnosis of subclinical hypothyroidism (CH) was made based on the levels of thyroid-stimulating hormone (TSH, >2.5 mED/L), as well as the presence of antibodies to thyroperoxidase (anti-TPO). Despite the pre-pregnancy euthyroid status in the presence of autoantibodies to thyroperoxidase and thyroglobulin, the increasing functional load on the thyroid gland during pregnancy contributes to the development of hypothyroidism.
Keywords: Gestational diabetes mellitus, Subclinical hypothyroidism, Anti-TPO, Thyroid-stimulating hormone
Cite this paper: Nasirova Shaxlo Shukhratovna, Subclinical Hypothyroidism as a Predictor of Gestational Diabetes, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1737-1739. doi: 10.5923/j.ajmms.20251506.22.
1. Introduction
- The International Diabetes Federation (IDF) estimated that more than 425 million people worldwide were diagnosed with diabetes in 2017 and that this number is projected to rise to 629 million by 2045 (World Health Organization, 2006) [4]. It is currently projected that 1 in 3 adults in the United States (USA) will have diabetes by 2025. The growing prevalence of type 2 diabetes mellitus is increasing significantly among adults, especially among young women of reproductive age who are diagnosed with this disease during pregnancy [5]. The prevalence of gestational diabetes mellitus (GDM) worldwide ranges from 5% to 25.5% and depends on race, ethnicity, age, physique, as well as screening and diagnostic criteria [6]. In the United States, approximately 1 out of every 10 pregnant women suffers from this disease, and almost 90% of cases of diabetes during pregnancy are associated with GDM [7]. The prevalence of GDM in Asian women is higher [8] than in US women. India ranks second in the world in terms of the number of diabetic patients and is one of the global epicenters of the diabetes epidemic. Diabetes mellitus is divided into three types: (1) Type 1 diabetes mellitus, (2) Type 2 diabetes mellitus (T2DM2), and (3) Gestational diabetes mellitus (GDM). In 90-95% of cases of diabetes mellitus in adults, T2DM was detected [4]. Diabetes during pregnancy causes permanent disorders of both maternal health and fetal growth [8].The purpose of the study consists to study the early diagnosis and metabolic abnormalities in gestational diabetes and to develop appropriate tactics for managing pregnancy and childbirth.
2. Material and Methods
- The examination and assessment of the patients' condition were carried out in accordance with the recommendations of WHO experts for the practical healthcare system [WHO, Geneva, 2012]. The study is a prospective follow-up of 109 pregnant women since the detection of GDM (Figure 1).
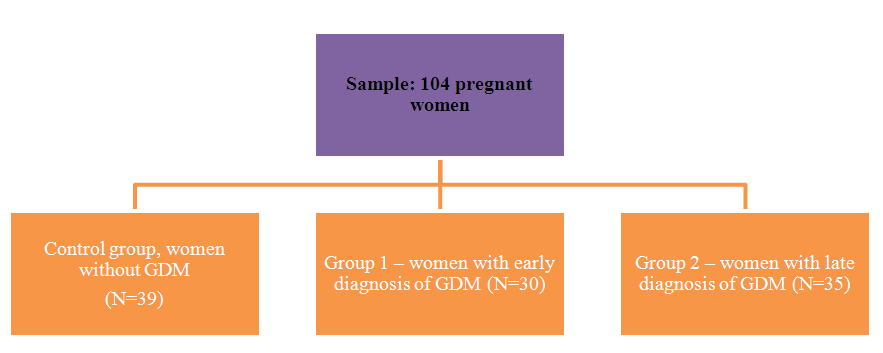 | Figure 1. Research design |
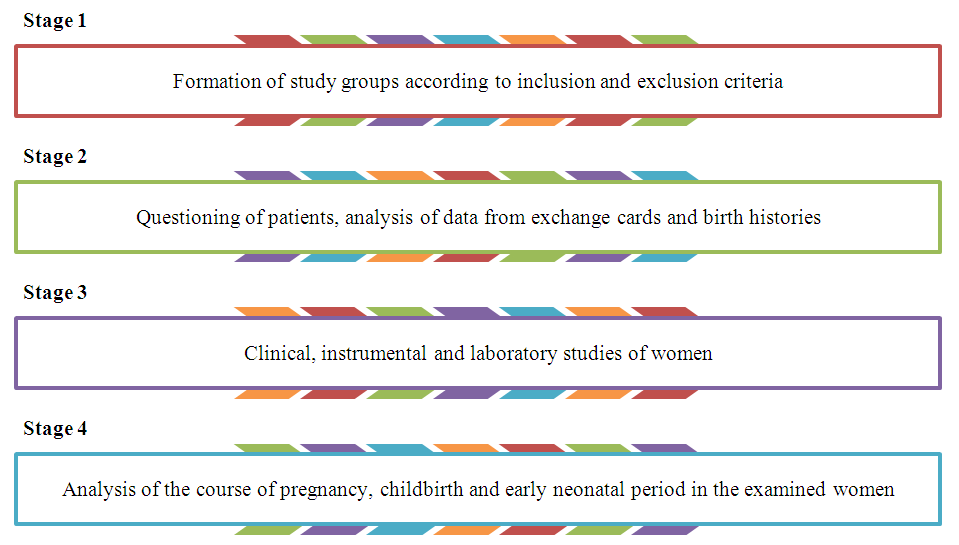 | Figure 2. Research program |
3. Results and Analyses
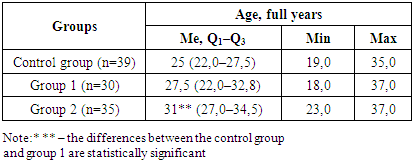
- An analysis of the study results showed that in the control group, the average age of the surveyed pregnant women was 25 (22.0–27.5) years (Table 1).
|
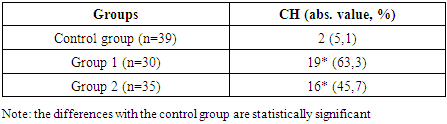
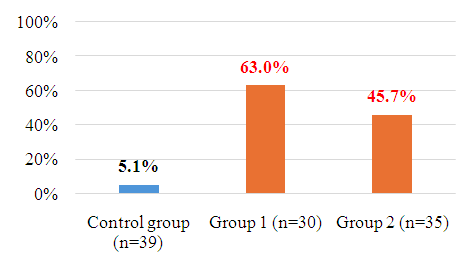 | Figure 3. The number of diagnosed subclinical hypothyroidism in the examined women |
|
|
|
4. Conclusions
- Perhaps one of the mechanisms of GDM development in HRT is a decrease in the activity of lipid and glucose metabolism enzymes due to a decrease in thyroid activity, followed by an increase in free fatty acid levels and an increase in blood pressure. Compensatory enhancement of deiodinase activity leads to an increase in endogenous glucose production, thereby closing the vicious circle. Startseva N. M. et al. suggested that GH and GDH are interrelated pathologies, and the TSH level of 2.7 IU/l is a predictor of GDH.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML