-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1711-1713
doi:10.5923/j.ajmms.20251506.17
Received: May 19, 2025; Accepted: Jun. 2, 2025; Published: Jun. 5, 2025

The Significance of Clinical and Electrophysiological Criteria in Diagnosing Knee Flexion Contractures in Children with Cerebral Palsy
Khamroev Farhod1, Eshmatov Mirlaziz2, Kholiqov Shavkatbek3
1DSc., Professor, Republican Children’s Neuropsychiatric Hospital, Uzbekistan
2Senior Lecturer, Andijan State Medical Institute, Andijan, Uzbekistan
3PhD., Associate Professor, Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Eshmatov Mirlaziz, Senior Lecturer, Andijan State Medical Institute, Andijan, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: This study aims to assess the clinical and electrophysiological criteria in diagnosing knee flexion contractures in children with cerebral palsy (CP) and to determine the diagnostic value of combined instrumental assessments. Methods: A total of 122 children with spastic diplegia were divided into two groups: the main group (n=54) and the control group (n=68). Assessment methods included clinical scales (GMFCS, Ashworth), EMG, goniometry, Hamstring test, and radiological imaging. Results: Strong correlations were found between clinical scales and contracture severity (r=0.82, p<0.01). EMG revealed dominant spastic activity in flexor muscles, and goniometry indicated reduced passive movement. Radiographs confirmed anatomical deformities. BEA coefficients over 1.5 indicated surgical candidacy. Post-treatment EMG showed a significant reduction in muscle hyperactivity. Conclusion: A multimodal diagnostic approach combining clinical and electrophysiological methods ensures accurate evaluation of contracture severity and guides optimal surgical planning in CP rehabilitation.
Keywords: Cerebral palsy, Knee flexion contracture, Electromyography, GMFCS, Ashworth scale, Goniometry, Spastic diplegia
Cite this paper: Khamroev Farhod, Eshmatov Mirlaziz, Kholiqov Shavkatbek, The Significance of Clinical and Electrophysiological Criteria in Diagnosing Knee Flexion Contractures in Children with Cerebral Palsy, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1711-1713. doi: 10.5923/j.ajmms.20251506.17.
1. Introduction
- Cerebral palsy (CP) in children is one of the leading causes of disability resulting from central neuromotor disorders. Pediatric cerebral palsy (PCP) is a complex clinical syndrome associated with static perinatal injuries to the central nervous system. This condition manifests as persistent motor function limitations, muscle tone disorders, and various forms of contractures. Orthostatic and motor deficits caused by CP not only limit a child's mobility but also hinder their social adaptation [1,3]. Among the clinical manifestations of CP, knee flexion contractures play a significant role. These contractures severely impair walking ability, causing difficulties in foot placement, initiating steps, dynamic imbalance, and orthopedic complications [4,5]. Such impairments increase the level of disability and complicate treatment approaches [6].Modern medicine emphasizes individualized treatment strategies based on the neurophysiological state of each patient. Surgical indications identified through electromyography (EMG) and clinical assessment scales (GMFCS, Ashworth) may lead to improved outcomes. Various functional, clinical, electrophysiological, and imaging methods have been developed to diagnose and manage knee flexion contractures. Enhancing these methods remains a vital task in contemporary clinical practice [7,8].The increasing number of children diagnosed with CP in Uzbekistan and the difficulty of achieving full rehabilitation in many of these patients highlight the urgency of addressing contractures requiring immediate and effective correction [2,9]. In such circumstances, early and accurate detection of knee flexion contractures and the development of individualized treatment strategies are of paramount importance.
2. Materials and Methods
- A total of 122 children diagnosed with cerebral palsy were selected for the study. They were divided into two groups: the Main Group comprised 54 children with knee flexion contractures who underwent clinical, instrumental, and functional examinations for diagnostic purposes; the Control Group consisted of 68 children with similar contractures examined using identical diagnostic and functional criteria.
3. Results and Discussion
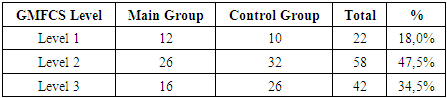
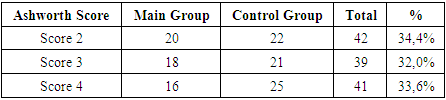
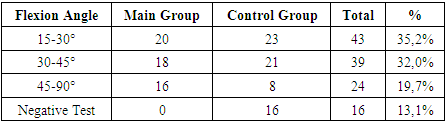
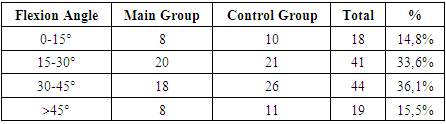
- The study included 122 children with cerebral palsy, among whom 54 were in the Main Group and 68 in the Control Group. All had knee flexion contractures. The children ranged in age from 4 to 15 years, and all exhibited spastic diplegia of GMFCS levels II–IV. Gross motor function was assessed using the Gross Motor Function Classification System (GMFCS), while muscle tone was evaluated using the Ashworth scale. Patients with GMFCS levels IV–V were excluded due to undeveloped orthostatic function.Hamstring test results revealed the following: 43 children (35.2%) had flexion angles of 15–30°, 39 (32.0%) had 30–45°, and 24 (19.7%) had ≥45°, with fixed contractures (≥45°) more frequently observed in GMFCS level 3 and Ashworth level 4 patients. All patients underwent EMG to assess the bioelectric activity (BEA) of the gastrocnemius and anterior tibial muscles and tibial nerve conduction. The degree of synergy and antagonism, as well as BEA coefficients, provided reliable electrophysiological markers for contracture pathogenesis. In muscles with high BEA and a BEA coefficient >1.5, indications for aponeurotic extension were established, based on motor function and pathogenesis.All patients also underwent anteroposterior and lateral X-ray imaging. In 66 children (54.1%), moderate flexion angles (20–40°) were identified, and in 56 (45.9%), severe contractures (≥45°) were observed. A strong correlation was found between radiographic data and clinical indicators (GMFCS, Ashworth scores) with a coefficient of r=0.82; p<0.01. Muscle function was preserved during surgery in the Main Group, and active walking ability improved significantly.
|
|
|
|
4. Conclusions
- A comprehensive assessment using clinical and instrumental diagnostic tools is essential in evaluating knee flexion contractures in children with cerebral palsy. The combination of Ashworth and GMFCS scales, EMG, goniometry, and radiographic analysis ensures accurate diagnosis of contracture severity and associated anatomical alterations. Goniometry and radiology are crucial methods for detecting tissue and bone changes caused by spastic contractures and play a key role in planning effective treatment strategies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML