-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(6): 1683-1686
doi:10.5923/j.ajmms.20251506.11
Received: May 8, 2025; Accepted: May 26, 2025; Published: Jun. 5, 2025

Prespective Predicts for the Development of Endometric Hyperplasia of the Endometria in the Late Reproductive Period
Usmanova N. Yu.1, Nurkhanova N. О.2
1Obstetrician Gynecologist, Bukhara Branch of the Republican Scientific Center of Emergency Medical Care, Bukhara, Uzbekistan
2Assistant of the Department of Obstetrics and Gynecology in Family Medicine, Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Nurkhanova N. О., Assistant of the Department of Obstetrics and Gynecology in Family Medicine, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Currently, proliferative diseases of the endometrium are a known background for the development of endometrial cancer. In this regard, improving diagnostics, studying additional risk factors and predictors of endometrial hyperplasia, as well as methods for preventing this disease are important aspects of the prevention of cancer. This article presents our own results of the research.
Keywords: Endometrial hyperplasia, ROС- analysis, Dyslipidemia, Estradiol, Progesterone, Obesity
Cite this paper: Usmanova N. Yu., Nurkhanova N. О., Prespective Predicts for the Development of Endometric Hyperplasia of the Endometria in the Late Reproductive Period, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1683-1686. doi: 10.5923/j.ajmms.20251506.11.
1. Introduction
- Endometrial hyperplasia (EH) is a pathological condition characterized by abnormal proliferation of endometrial glands and stroma. The main characteristic feature of this disease is the proliferation of the inner layer of the uterus-endometrium, which leads to its thickening and increase in volume [1,5,8,11]. In the structure of gynecological pathology, endometrial hyperplastic processes (GPE) occur with a frequency of 15-40%. According to the referral data, the frequency of GPE varies depending on its form and the woman's age from 10 to 30% [4,6,12]. Endometrial hyperplastic processes are most often detected at the age of 45-55. According to some authors, this pathology occurs in 50% of patients in the late reproductive and perimenopausal period [1,2,11].Endometrial hyperplastic processes develop, as a rule, against the background of absolute or relative hyperestrogenemia or against the background of absolute or relative progesterone deficiency. Estrogens that normally cause proliferative changes in the endometrium, in the absence of sufficient progesterone effect on the endometrium, lead to the development of hyperplastic processes in it [3,7,10].Metabolic and endocrine disorders play a significant role in the pathogenesis of endometrial hyperplastic processes: changes in fat metabolism, sex hormone metabolism, immunity, and thyroid function during pathologies of the hepatobiliary system and gastrointestinal tract. In this regard, patients with endometrial hyperplastic processes often experience obesity, hyperlipidemia, diabetes mellitus, hypertension, and metabolic syndrome [4,9,12].Despite numerous scientific studies devoted to endometrial hyperplastic diseases, studying risk factors for malignization of the process, and management tactics, the issues of predicting, early diagnosis, and treatment of subclinical forms of GE have not yet been fully studied and scientifically substantiated.Purpose of the study: to identify significant predictors of endometrial pathology in women of late reproductive age.
2. Materials and Methods of Research
- The study included 137 women of late reproductive age (34-46 years old) who underwent examination and treatment in the gynecology department of the Bukhara branch of the Republican Scientific Center for Emergency Medical Care. The research period was from 2021 to 2024.Inclusion criteria included the presence of endometrial pathology, the absence of malignant neoplasms confirmed by morphological examination, and the presence of complete medical documentation. Patients with oncological diseases, severe somatic pathologies, hemostasis disorders, and complicated obstetric history were excluded.Statistical processing of the research results was carried out using the Statistica for Windows 6.0 software package (StatSoft, USA), as well as Microsoft Excel for constructing graphs and diagrams. All quantitative indicators were checked for compliance with the normal distribution using the Shapiro-Wilk criterion. In cases of normal data distribution, Student's t-test was used to assess statistically significant differences between groups. In cases where the data did not correspond to the normal distribution, the Mann-Whitney U-criterion was used, which allowed comparing independent samples by rank level.To determine the independent predictors of adverse treatment outcomes, a multifactorial analysis using logistic regression was conducted. Initial clinical and laboratory indicators, as well as the applied therapy methods, were considered as predictors. Assessment of the prognostic significance of individual indicators was carried out by constructing ROC-curves (Receiver Operating Characteristic) and calculating the area under the curve (AUC). This analysis made it possible to determine the sensitivity and specificity of the studied markers in diagnosing and predicting the outcome of the disease.Analysis of the obtained data allowed for an objective assessment of diagnostic and treatment approaches, identification of the most significant markers of inflammatory and hyperplastic changes in the endometrium, as well as assessment of the effectiveness of various treatment methods, taking into account the individual characteristics of patients.
3. Research Results
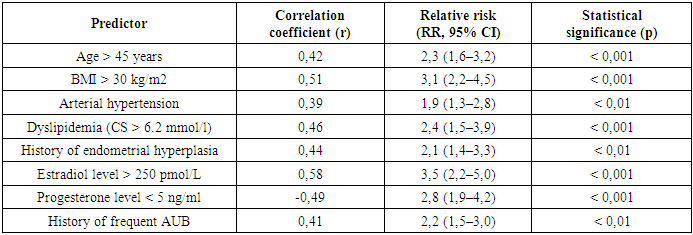
- The average age was 40.2 ± 3.8 years. The age distribution shows a tendency towards more frequent detection of the pathology in patients older than 38 years. The largest number of patients were represented in the age group 38-41 years (39.2%) and 42-46 years (39.1%).During the study, the main local causes of endometrial pathology in women of late reproductive age, as well as significant predictors of the unfavorable course of the disease, were identified. It has been proven that age-related changes in the hormonal background, the presence of metabolic syndrome, arterial hypertension, and obesity have the greatest impact on the development of hyperplastic processes and endometrial dysfunction.Statistical analysis showed that the frequency of abnormal uterine bleeding (AUB) among patients with endometrial pathology is 72.5%, which is 2.3 times higher than in the population of women of the same age without this pathology (p < 0.001). An important predictor of endometrial hyperplasia development is body mass index (BMI): in women with obesity (BMI > 30 kg/m2), the probability of detecting hyperplastic processes increases 3.1 times (OSH = 3.1; 95% CI 2.2-4.5; p < 0.001).Analysis of the hormonal status of patients showed that the level of estradiol in the proliferation phase in women with endometrial pathology was significantly higher (average 274.8 ± 35.6 pmol/l) compared to healthy women (193.2 ± 28.7 pmol/l, p < 0.05), which indicates hyperestrogenism as a risk factor. Conversely, the level of progesterone in the second phase of the cycle in patients with endometrial hyperplasia was lower (4.6 ± 1.2 ng/ml) compared to the control group (8.3 ± 1.5 ng/ml, p < 0.05), which confirms the deficiency of the lutein phase as a pathogenetic mechanism for the development of the disease.Arterial hypertension was also a significant risk factor: in women with hypertension, endometrial hyperplastic processes occurred 1.9 times more frequently (OSH = 1.9; 95% CI 1.3-2.8; p < 0.01), which is associated with vascular changes and impaired microcirculation in the endometrium. Dyslipidemia (total cholesterol level > 6.2 mmol/l) increased the risk of hyperplasia by 2.4 times (OSH = 2.4; 95% CI 1.5-3.9; p < 0.001), which confirms the metabolic basis of pathological processes.Among patients who underwent scraping due to endometrial hyperplasia, the risk of recurrence within a year was 28.6%. The most significant predictors of recurrence were the presence of obesity (OSH = 2.8; 95% CI 1.9-4.2; p < 0.001), hyperplasia without atypia in the anamnesis (OSH = 2.1; 95% CI 1.4-3.3; p < 0.01) and estradiol levels in the proliferation phase above 250 pmol/l (OSH = 3.5; 95% CI 2.2-5.0; p < 0.001).
|
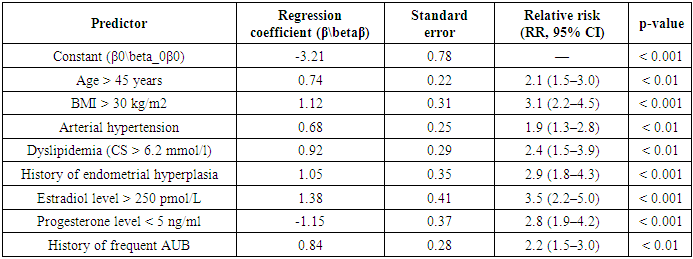
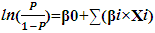 Where:• P - probability of endometrial hyperplasia development,• β0 - model constant,• βi - logistic regression coefficients for each predictor,• Xi - predictor values (1 - if the factor is present, 0 - if it is absent, or the actual value of the indicator).Based on statistical data processing, the following significant coefficients were obtained:
Where:• P - probability of endometrial hyperplasia development,• β0 - model constant,• βi - logistic regression coefficients for each predictor,• Xi - predictor values (1 - if the factor is present, 0 - if it is absent, or the actual value of the indicator).Based on statistical data processing, the following significant coefficients were obtained:
|
 At P > 0.5, the patient falls into the high-risk group and requires further in-depth diagnostics.The developed model allows for predicting the risk of endometrial hyperplasia with high accuracy (AUC = 0.87, sensitivity = 82%, specificity = 85%).
At P > 0.5, the patient falls into the high-risk group and requires further in-depth diagnostics.The developed model allows for predicting the risk of endometrial hyperplasia with high accuracy (AUC = 0.87, sensitivity = 82%, specificity = 85%).4. Conclusions
- Endometrial hyperplasia is the most frequently observed endometrial anomaly in patients with abnormal uterine bleeding in the late reproductive period. An important predictor of endometrial hyperplasia development is age-related changes in the hormonal background, including excessive estrogen production and decreased progesterone levels, the presence of metabolic syndrome, arterial hypertension, and obesity. These indicators and calculations allow us to assess the condition of the endometrium, which is prognostically valuable information for making a decision regarding the treatment of this pathology.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML