Fozilov Uktam Abdurazzoqovich, Eronov Yoqub Quvatovich
Bukhara State Medical Institute named after Abu Ali Ibn Sino, Bukhara, Uzbekistan
Correspondence to: Eronov Yoqub Quvatovich, Bukhara State Medical Institute named after Abu Ali Ibn Sino, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
In children with disabilities, maxillary protrusions account for 36.8% of all maxillofacial deformities. Early diagnosis and effective treatment of these pathologies in orthodontic practice are one of the urgent problems awaiting a solution. In recent years, there has been an increase in the number of class II deformities according to Engel's classification and a decrease in class III deformities, which is associated with changes in chewing pressure loads.
Keywords:
Disabled children, Upper jaw protrusions, Tooth-jaw system deformations
Cite this paper: Fozilov Uktam Abdurazzoqovich, Eronov Yoqub Quvatovich, Indicators of Prevalence Depending on Age of Maxillary Protrussions in Children with Disabilities, American Journal of Medicine and Medical Sciences, Vol. 15 No. 6, 2025, pp. 1658-1662. doi: 10.5923/j.ajmms.20251506.05.
1. Introduction
In children with disabilities, upper jaw protrusions are dominated by combined anomalies during the period of changes in the tooth-jaw system, which occur in 34.02%, but in the period of permanent bite, data on their percentage increasing to 39.58% are presented in scientific sources. Deformations in the tooth-jaw system make up 14.08% of dental diseases, which decrease to 11.2% during permanent bite. Anomalies in the period of temporary occlusion constitute 4.35%, 1.4% in the period of exchange occlusion, 0.89% in the period of permanent occlusion, and in the defects of tooth rows, these pathologies make up only 1.3% of the total number.Postnikov M.A. (2020) et al. anomalies in the structure of hard dental tissues prevail (43.48%) during temporary bite occlusion. In 2.4% of the total number of dental-jaw system deformations, anomalies in the size of teeth are detected, they are detected mainly during the period of teeth change, 2.8% during permanent bite, these anomalies are observed to increase in 2.22% of cases [1,3,5,7,9].Karpanova A.S. (2018), co-authored by others, it was found that during the period of permanent occlusion, dental anomalies increased in 9.78% of cases, in the period of alternating occlusion, in 1.87%, and in 5.63% of cases, compared to the period of temporary occlusion. In addition, the prevalence of maxillary protrusions is 49.16% in the period of alternating occlusion, 47.63% in the period of temporary occlusion, and 46.2% in the period of permanent occlusion.Ayupova F.S. (2020) and the data of other co-authors show that mesioocclusion occurs in 2.72% during permanent bite, 5.08% during alternating bite, and mesioocclusion in 3.85%. In permanent bite, deep pricus is observed in 26.63%, in mixed bite in 18.22%.Fozilov U.A. (2023) and others, co-authored, showed that the early clinical sign of the development of maxillary protrusions in children aged 4-5 years is the location of the distal surfaces of the second primary molars in a vertical plane. Also, the functional impact on the lower jaw during the sucking function in infancy helps to increase its length and forward movement. After the eruption of the milk teeth, their closure returns to normal [2,4,6,8,10,12]. With the eruption of the milk teeth I-II, an increase in the alveolar height is observed. Thus, the study of the origin and distribution of various types of anomalies of the dento-maxillary system has provided us with information about the presence of malocclusions in scientific research.
2. Research Object
In the orthodontic department of the Bukhara Regional Specialized Children's Dentistry Center in 2020-2024, 184 children with maxillary protrusion in children with disabilities aged 4 to 18 years were recruited. Children with maxillary protrusion in children were examined using objective, subjective and dental examination methods (Dolgopolova, Tonn, Snagina, Gerlach, Tanaka-Johnson methods), as well as anthropometric methods and intraoral scanning, photometric and CAD/CAM technology using the Exocad program.
3. Results and Analyses
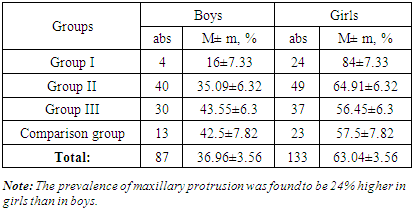
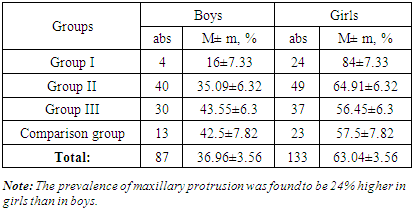
In our scientific study, sick children were divided into 3 main groups and a comparison group.of group I, a study was conducted using the Dolgopolova method on 28 sick children aged 4 to 6 years during the period of eruption of deciduous teeth.of group II, 89 patients aged 7 to 13 years old during the period of Almanach bite were analyzed using the Corkhouse, Tonn, Snagina, Tanaka-Johnson methods, as well as TRG lateral projection, intraoral scanning impression taking, photometric and CAD/CAM technology using the Exocad program.In children with disabilities of group III, 67 children aged 14 to 18 years were examined using the Korkhaus, Tonn, Pon-Linder-Hart, Gerlach, Snagina and TRG lateral projections, intraoral scanning impression taking, photometric and CAD/CAM technology using the Exocad program. When examining patients with maxillary protrusion using additional orthodontic examination methods, it was found that the incidence of the disease was higher in girls than in boys.The comparison group included patients aged 4 to 18 years. 36 people tooth-jaw system Anthropometric examination methods of patients with anomalies were taken.The distribution of children with maxillary protrusions by age and gender is shown in Table 1.Table 1. Maxillary protrusions in children with disabilities by age and gender
 |
| |
|
In addition to traditional examination methods, we considered it appropriate to conduct intraoral scanning, impression taking, photometric and CAD/CAM technology using the Exocad program in the examined sick children. In addition, the main and additional examination methods were used in the examined sick children. In the objective examination, attention was paid to the harmony of the face according to the author Persin L.S.In this case, a straight line is drawn from the tip of the nose to the chin on the side of the patient. The position of the upper and lower lips relative to the line is assessed. The facial profile is examined according to Dreyfus. In children with maxillary protrusion, the KPF angle is also determined [11,13].Genetic factors play an important role in the prevalence of maxillary protrusions. The study of distal occlusion involves assessing the location of the teeth in the dentition and the relationship of the teeth when they are in contact. Correct occlusion is characterized by a number of factors. The upper jaw parameters that characterize distal occlusion are the size of the upper and lower jaws, the shape of the teeth, the congenital absence of tooth rudiments (primary edentia), the location of tooth rudiments in the jaw bones, and the size of the teeth.Table 2. Up jaw of protrusions in the spread antenatal pathologies
 |
| |
|
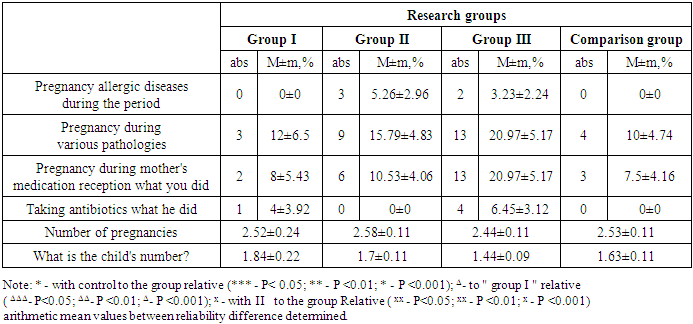
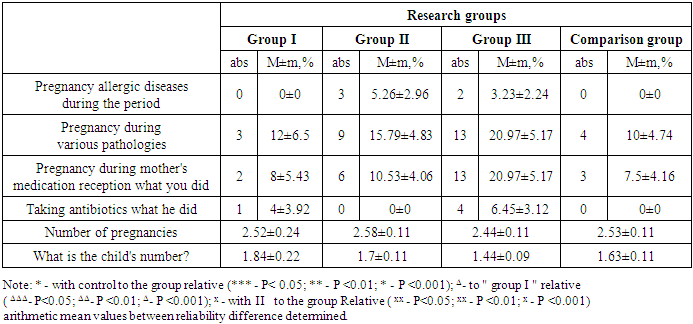
1. Hereditary disproportion of the size of the teeth and jawbone, as well as the dense arrangement of the teeth (with a lack of free space) or the presence of teeth and diastemas (gaps between the teeth).2. The incorrect position, shape, or size of the upper jaw is also considered a genetic factor.The genetic nature of these factors, as well as environmental factors (for example, bad habits), contribute to the high intensity of the manifestation of this pathology. The leading role of heredity in the formation of the following indicators has been proven: the size and shape of the teeth, the width and length of the teeth, the height of the palatal arch, the state of the deep bite, the profile of the face, the shape of the skull and facial parameters, including the upper and lower parts of the face, changes in the ratio of the jaws. In patients with maxillary protrusions, the premorbid background, that is, concomitant diseases, was also identified as one of the methods of our study, and the results of the data on the premorbid background are presented in Table 3.Table 3. Intergroup distribution of comorbidities in patients with maxillary protrusion
 |
| |
|
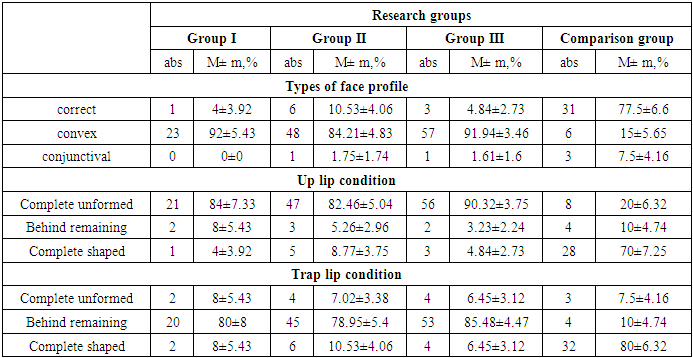
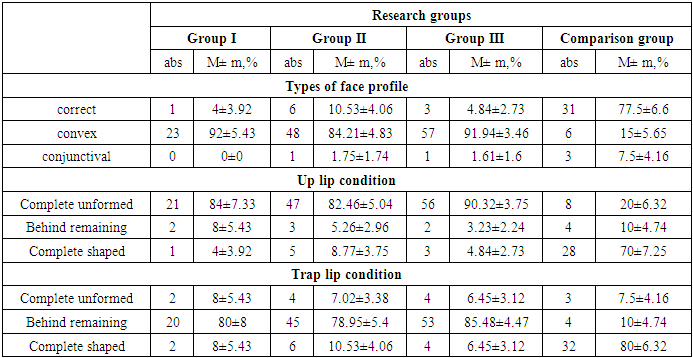
Attention was also paid to the morphological structure of the upper and lower jaws, the interior of the mouth, and the location of the teeth in the tooth rows. The subjective examination was carried out by asking the parents of children with maxillary protrusion (the criteria for the transition of the condition during pregnancy, types of delivery, types of feeding of the child, up to what age the child used a pacifier, what types of harmful habits he had, whether he had chronic diseases of the upper respiratory tract and how long the disease lasted). Additional examination methods were TRG in lateral projection, OPG radiography and intraoral scanning with impression taking and photometric, anthropometric examination methods using CAD / CAM technology using the Exzocad program.In patients with maxillary protrusion, changes in the maxillary region have a detrimental effect on the normal physiological state of chewing. Data on changes in the facial profile, position of the upper and lower jaws, cheekbones, upper and lower lip folds, and tongue position in the examined patients are presented in Table 4.Table 4. Changes in the protrusions of the upper jaw (facial profile, position of the upper and lower lip)
 |
| |
|
In the study participating in patients high jaw of protrusions pricus state in the spread, high and lower lip tongue, tongue in the state pathological changes results are in table 5 own expression found Under investigation facial profile types in our patients straight, convex conjunctival forms, high lip of the situation complete unformed, from formation behind remaining, complete shaped types was studied. Also the bottom lip of the situation complete unformed, from formation behind remaining, complete shaped types intergroup and comparison groups according to interest quantities studied and inspection results based on necessary practical recommendations given.Table 5. Inspection take going in patients (pricus condition, high and lower lip tongue, tongue condition ) pathologies
 |
| |
|
Up jaw protrusions with sick pricus condition in patients side of teeth normal occlusion II and comparison group, retrogeny in groups I-III, right pricus all group in patients this of pathologies high degree owner that research to the results was determined.Inspection take visited first group in our patients high lip toy 12% short, 12% wide, short combination in 16% of patients met. Second group in patients high lip toy short 12.28%, wide 15.79%, short united 29.82% of cases were observed. Third group in patients short 4.84%, wide 19.35%, short combination was found in 25.81% and comparison group in our patients and, high lip toy short 17.5%, short 7.5% and short the merger is 22.5% in inspections studied.First group in our patients high lip toy width 8%, short combination in 16% of patients met. Second group in patients high lip toy short 21.05%, wide 12.28%, short united 22.81% of cases were observed. Third group in patients short 14.52%, wide 14.52%, short combination was found in 24.19% and comparison group in our patients and, high lip toy short 10%, short 7.5% and short 20% of the amount determined and clinical signs of the disease with analytical results compared.In the first group of children with maxillary protrusion, the upper lip was short in 20%, wide in 36%, and short in 36% of patients.
4. Conclusions
In the second group of patients in our study, the upper lip was short 33.33%, wide 31.58%, and short-fused 31.58%. In the third group of patients, it was short 4.84%, wide 19.35%, and short-fused 25.81%. In the comparison group of patients, the upper lip was short 25%, short 10%, and short-fused 62.5%, and the protrusion state was compared with the morphofunctional disorders of the maxillofacial structure. In addition, recommendations were given based on a preventive program in patients whose pathological changes in the maxillofacial structure were studied.
References
| [1] | Arunachalam, S. Orthodontic appliances and oral hygiene: Are we asking the right questions? / S. Arunachalam, J. Sharan, I. Sivakumar [et al.] // Amer.j. of orthodontics and dentofacial orthopedics. - 2018. - Vol. 154, № 2. - P. 155- 156. |
| [2] | Ardani, I. G. Cephalometric Characteristic of Skeletal Class II Malocclusion in Javanese Population at Universitas Airlangga Dental Hospital | I. G. Ardani, M. L. Sanjaya, J. Sjamsudin // Contemp. Clin. Dent. - 2018. - Vol. 9 (Supp l.2).- P. 342-346. |
| [3] | Alobeid, A. Comparison of the force levels among labial and lingual self-ligating and conventional brackets in simulated misaligned teeth / A. Alobeid, T. El-Bialy, S. Khawatmi [et al.] // Eur. J. Orthod. - 2017. - Vol.39 (4). - P. 419-425. |
| [4] | Bazarova, K. M. Ortodontic problems in the treatment of patients with dental defects / K. M. Bazarova, R. A. Zhartybaev, B. B. Salymbekov, M. K. Iskakova // В сборник: Stience and educationA problems and innovations/ сборник стaтeй VII Meждунapoднoй нaучнo-пpaктичeскoй кoнфepeнции. - neroa, 2021. - C. 117-125. |
| [5] | Cantarella, D. Changes in the midpalatal and pterygopalatine sutures induced by microimplant-supported skeletal expander, analyzed with a novel 3D method based on CBCT imaging / D. Cantarella, R. Dominguez-Mompell, S. M. Mallya, [et al.] // Prog Orthod. - 2017. - P. 18-34. |
| [6] | Vorobeva, M. V. Causes behind distal occlusion / M. V. Vorobeva, S. V. Konnov, N. V. Bulkina, [et al.] // Archiv EuroMedica. - 2019. - Т. 9. № 1. - С. 191-193. |
| [7] | Choi, S. H. Effect of malocclusion severity on oral health-related quality of life and food intake ability in a Korean population / S. H. Choi, J. S. Kim, J. Y. Cha [et al. ] // Am J Orthod Dentofacial Orthop. - 2016. - №149 (3). - P. 38490. |
| [8] | Felter, M. Comparative study of the usability of two software programs for visualization and analysis of digital orthodontic models / M. Felter, M. M. Lenza, M. G. Lenza [et al.] // J. Dent. Res. Dent. Clin. Dent. Prospects. - 2018. -Vol.12 (3). - P. 213-220. |
| [9] | Postnikov, M. A. Functional evidence-based dentistry in osteopathic correction of distal occlusion / M. A. Postnikov, O. N. Pavlova, F. G. Klochkov, E. O. Guseva // International Research Journal. - 2021. - № 4-2 (106). - C. 148-152. |
| [10] | Gay, G. Root resorption during orthodontic treatment with Invisalign®: a radiometric study / G. Gay, T. Ravera, F. Castroflorio, [et al.] // Prog. Orthod. -2017. - №18(1). - P. 12. |
| [11] | Hourfar, J. Influence of interradicular and palatal placement of orthodontic mini-implants on the success (survival) rate / J. Hourfar, D. Bister, G. Kanavakis [et al.] // Head Face Med. - 2017. - Vol.13. - P. 14-18. |
| [12] | Ishchenko, T. The instant diagnostics of obstruction of the upper airway for children with distal occlusion / Ishchenko T., Kharke M., Kharke V.V. // В книге: мaтеpиaлы Х Междутародной таучной конференции. Российский университет дружбы тародов. 2019. С. 83. |
| [13] | Jayaratne, Y. S. Maxillary incisors changes during space closure with conventional and skeletal anchorage methods: a systematic review / Y. S. Jayaratne, F. Uribe, N. Janakiraman // J. Istanb. Univ. Fac. Dent. - 2017. - Vol. 51 (3 Suppl 1). - P. 90-101. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML