-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1628-1631
doi:10.5923/j.ajmms.20251505.73
Received: May 2, 2025; Accepted: May 23, 2025; Published: May 30, 2025

Criteria for Evaluating the Results and Long-Term Prognosis of Surgical Interventions in Ischemic Mitral Insufficiency
Ismatov A. A.1, Yarbekov R. R.2, Teshayev U. Sh.3, Muradov M. M.4, Akhmedov X. E.5, Nishonov N. A.4
1Cardiac Surgeon, Jizzakh Branch of the Republican Specialized Cardiology Center, Jizzakh, Uzbekistan
2Doctor of Medical Sciences, Republican Specialized Scientific and Practical Medical Center of Surgery named after Academician V. Vakhidov, Tashkent, Uzbekistan
3Doctor of Philosophy, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
4Doctor of Philosophy, American Hospital Clinic, Tashkent, Uzbekistan
5Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

It should be noted that as experience accumulates in the use of surgical methods for the treatment of MC diseases, there is a need for an objective assessment of the long-term prognosis and results of this intervention. Thus, patients whose share of total scarring after MI was less than 25%, with complete revascularization with MC intervention, survival rates increase. However, patients with IMR and a more severe increase in myocardial scarring have the highest risk of mortality despite surgical treatment.
Keywords: Revascularization, Mitral regurgitation, Aortocoronary bypass grafting, Transthoracic echocardiography, Tricuspid insufficiency, Infective endocarditis, Mitral valve
Cite this paper: Ismatov A. A., Yarbekov R. R., Teshayev U. Sh., Muradov M. M., Akhmedov X. E., Nishonov N. A., Criteria for Evaluating the Results and Long-Term Prognosis of Surgical Interventions in Ischemic Mitral Insufficiency, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1628-1631. doi: 10.5923/j.ajmms.20251505.73.
- This study analyzed mortality, early, and long-term outcomes after surgical intervention in patients diagnosed with ischemic mitral regurgitation (IMR). The research was based on both retrospective and prospective data.
1. Introduction
- Another unexplored issue, which is emphasized by clinicians, is the risk factors affecting mortality, immediate and long-term results after surgical intervention on the IC in patients with IMR. Due to the fact that despite significant advances in medical and surgical therapies, the risk of mortality associated with IMR after MI remains high [1], [2], [3], [4]. Also, current evidenc Interesting in this direction are the studies of R. Lorusso et al. Lorusso et al. (2008) in a multicenter retrospective registry evaluated postoperative outcomes of emergency surgical interventions for severe acute MI in 279 patients. In doing so, the authors found that early mortality among patients with ischemic etiology was higher than in other etiologies of acute MI, such as degenerative or infective endocarditis (26.9% vs. 14.8% and 22.7%, respectively). In addition, postoperative complications were more frequent in patients with acute MI, requiring longer ICU stays and a greater need for inotropes and mechanical support. It is worth noting that in this registry in multivariate analysis the main predictors of early death were acute endocarditis, LV dysfunction and CHD [5]. e suggests that surgical intervention of MI is associated with significant mortality.The indications for surgery for IMR are limited due to the lack of survival benefit. Therefore, surgical treatment of IMR is recommended only for patients who remain symptomatic despite optimal medical therapy [4], [6], [7].Of particular note is the study by N. Sharma et al (2021) involving 1000 consecutive patients admitted with MI in 2016/17 treated with percutaneous coronary intervention with transthoracic echocardiography before discharge. Compared to patients without MR, patients with MR were older (70 ± 12 vs. 63 ± 13 years; p < 0.001), with worse left ventricular ejection fraction (LVEF) (52 ± 15% vs. 55 ± 11%; p < 0.001) and creatinine clearance (69 ± 33 mL/min vs. 90 ± 39 mL/min; p < 0.001). They also had higher rates of hypertension (64% vs. 55%; p = 0.012), heart failure (3.4% vs. 1.1%; p = 0.014), previous MI (28% vs. 20%; p = 0.005), and severe flow limitation in the circumflex (50% vs. 33%; p <0.001) or right coronary artery (51% vs. 42%; p = 0.014). The prevalence and severity of MR were not affected by IM subtype. Revascularization later than 72 hours after symptom onset was associated with an increased likelihood of MR (33% vs. 25%; p = 0.036) in patients with non-ST-elevation myocardial infarction (NSTEMI). At a median of 3.2 years, 56 of 288 (19%) patients with untreated MR died. Age and LVEF independently predicted all-cause mortality. A number of authors have identified the following significant risk factors for complications and mortality in surgical treatment of moderate ischemic MI: severe heart failure (NYHA class IV), marked reduction in LVEF (less than 30%), large effective regurgitation orifice area (more than 70 mm2), excessively high natriuretic peptide level (more than 10 000 pg/mL), severe right ventricular failure (tricuspid annular plane systolic excursion less than 15 mm), high pulmonary hypertension or tricuspid annular plane systolic excursion, and severe concomitant comorbid pathology. tricuspid annular plane systolic excursion) less than 15 mm), high pulmonary hypertension or tricuspidal insufficiency and severe associated comorbid pathology (e.g., severe renal failure) [8], [9], [10]. Preserved annulus geometry and myocardial viability studies can help predict the likelihood of improvement in IMR after revascularization. It may also help identify patients who are more likely to benefit from revascularization combined with MC intervention [11], [12]. K. Kusunose et al (2017) conducted an observational cohort study to identify predictors of mortality in patients with percutaneous MC intervention (15 underwent MC replacement and 102 underwent MC repair).
2. Methods
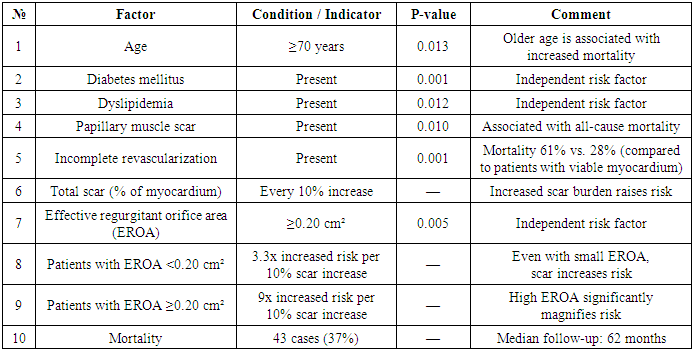
- Clinical, instrumental, and laboratory data from patients diagnosed with ischemic heart disease and mitral regurgitation were analyzed. Data from the multicenter retrospective registry conducted by Lorusso et al. (2008) and the prospective observation study involving 1,000 myocardial infarction (MI) patients conducted by N. Sharma et al. during 2016–2017 were included. Additionally, the observational cohort study by Kusunose et al. (2017), aimed at identifying mortality predictors in patients undergoing percutaneous mitral valve (MC) intervention, was used.Demographic characteristics, cardiac function parameters (left ventricular ejection fraction — LVEF), laboratory results (creatinine clearance, natriuretic peptide levels), and history of previous conditions (hypertension, diabetes, heart failure, prior MI) were evaluated.- The severity of ischemic mitral regurgitation was assessed by transthoracic echocardiography.- Myocardial viability and scarring were evaluated using cardiac magnetic resonance imaging (MRI).- Surgical interventions included percutaneous mitral valve procedures (repair or replacement) and emergency revascularization surgeries.- All patient information was kept confidential, recorded into individual registration forms, and transferred into electronic format for statistical analysis.During the study, magnetic resonance imaging (MRI) was used to assess LV remodeling and myocardial scarring. The effective regurgitant orifice area was calculated from the surface area of the proximal isovelocity using echocardiography. There were 43 deaths (37%) during follow-up (median, 62 months). In multivariate analysis, age ≥70 years (P=0.013), diabetes mellitus (P=0.001), dyslipidemia (P=0.012), papillary scar (P=0.010), incomplete revascularization (P=0.001), and total scar (%), effective regurgitant orifice area ≥0.20 cm2 (P=0.005) were independently associated with all-cause mortality. Although patients with effective regurgitant orifice area <0.2 cm2 at baseline demonstrated an increased hazard ratio of 3.3 for every 10% increase in scar, the hazard ratio increased to 9 for every 10% increase in scar in those with baseline effective regurgitant orifice area ≥0.20 cm2. Mortality was also significantly higher in patients with incomplete revascularization compared with patients with vascularized viable myocardium (61% versus 28%; P<0.001).
|
3. Conclusions
- Ischemic mitral regurgitation (IMR) following myocardial infarction remains a serious clinical problem associated with high mortality and morbidity despite advancements in medical and surgical treatments. Studies show that surgical interventions for IMR are linked with significant early and late mortality, particularly in patients with severe left ventricular dysfunction, extensive myocardial scarring, or incomplete revascularization. Identifying risk factors such as age, left ventricular ejection fraction, myocardial viability, degree of mitral regurgitation, and comorbidities like diabetes and renal failure is crucial for improving patient selection and outcomes.Recent evidence supports a more selective approach to intervention, favoring surgery or transcatheter therapies only for symptomatic patients unresponsive to optimal medical management. Imaging modalities like cardiac MRI provide valuable prognostic information and can guide therapy planning. However, recurrence of mitral regurgitation after surgical repair remains a major challenge, especially with restrictive annuloplasty techniques. Further research is needed to refine surgical strategies and to better personalize treatment to maximize survival and quality of life in this high-risk patient group.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML