-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1544-1548
doi:10.5923/j.ajmms.20251505.52
Received: May 3, 2025; Accepted: May 22, 2025; Published: May 27, 2025

Risk Factors of Cardiovascular Complications Among Patients with Prediabetes in Andijan City and Markhamat District of the Republic of Uzbekistan According to Screening Data
Yusupova Sh. K.1, Abdurakhmanova R. Kh.2
1Associate Professor, Head of the Department of Hospital Therapy and Endocrinology, Doctor of Medical Sciences, Andijan State Medical Institute, Andijan, Uzbekistan
2Free Applicant of the Department of Hospital Therapy and Endocrinology, Andijan State Medical Institute, Andijan, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study examines the prevalence and risk factors for cardiovascular complications among individuals with prediabetes in Andijan city and Markhamat district of Uzbekistan. A total of 3400 individuals at risk were screened using anthropometric, clinical, biochemical, and instrumental methods. The analysis focused on body mass index, waist circumference, blood pressure, lipid profile, physical activity, and family history of diabetes and cardiovascular diseases. Results showed significant differences in the prevalence of type 2 diabetes mellitus and associated cardiovascular risks between urban and rural populations. Key predictors of cardiovascular complications included high BMI, increased triglyceride levels, chronic heart failure, and genetic predisposition. The findings emphasize the importance of early detection and targeted prevention strategies for high-risk groups.
Keywords: Risk factors, Type 2 diabetes mellitus, Prediabetes
Cite this paper: Yusupova Sh. K., Abdurakhmanova R. Kh., Risk Factors of Cardiovascular Complications Among Patients with Prediabetes in Andijan City and Markhamat District of the Republic of Uzbekistan According to Screening Data, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1544-1548. doi: 10.5923/j.ajmms.20251505.52.
Article Outline
1. Introduction
- Type 2 diabetes mellitus (DM 2) is a category of metabolic disorders characterized by hyperglycemia, which occurs when the pancreas stops producing enough insulin or when the body cannot use it. Diabetes causes many complications that are associated with increased morbidity and mortality [1,2]. Type 2 diabetes mellitus was prevalent in 9.3% of the world's population [3]. Mortality rates from type 2 DM decreased from 2000 to 2010, then increased from 2010 to 2016 in developed countries, while mortality rates from type 2 DM increased in low-income countries during both periods [4]. The increase in prevalence and incidence of DM 2 has been attributed to changes in urban habits that are associated with sedentary lifestyles [5].The last 2-3 decades have witnessed marked lifestyle changes with significant population growth and urbanization, which are major risk factors that have been repeatedly reported. Pre-diabetes mellitus (pre-DM) is a general term that refers to an intermediate state of abnormal glycemia. It is also known as impaired glucose regulation (IG), which includes 2 groups of individuals: subjects with impaired fasting glucose (IFG) and subjects with impaired glucose tolerance (IGT). [1]. It is increasing worldwide, and the number of people with pre-DM worldwide is estimated to reach 472 million by 2025, the authors noted in 2015. [2]. Pre-DM has received increasing attention in the literature in recent years as it has become a huge public health burden in general and in several countries where the incidence of Pre-DMhas reached 50.1% among adults. This has become a concern about the impact of Pre-DMon macrovascular events, and research is urgently needed to strengthen evidence-based treatment recommendations for patients with pre-DM 2. A recent systematic review concluded that UWG does not or only slightly increases the risk of cardiovascular disease, whereas a community-based study found that glycohemoglobin levels, not fasting glucose levels, are significantly associated with cardiovascular disease. Another significant study from Korea found that an increased risk of myocardial infarction was only seen with glucose levels characteristic of diabetes. At the same time, other researchers have noted that hyperglycemia within the nondiabetic glucose range is associated with an increased risk of cardiovascular disease [13]. As we all know, cardiovascular disease (CVD) is the leading cause of mortality and morbidity worldwide, and DM is a risk factor for serious chronic diseases, including CVD [5-7]. However, studies on the presence and accumulation of CVD risk factors in the NRH stage have been scarce and have not reached a general consensus. [8-12]. In addition, few articles were found in the literature on CVD risk associated with blood glucose. Therefore, the question arose about the association of risk factors for the development of CVDs in prediabetics in the Uzbek population.All of the above provided the basis for the present study.The aim of the study was to investigate risk factors for cardiovascular complications among prediabetic patients in Andijan city and Markhamat district of the Republic of Uzbekistan according to the screening data.
2. Material and Methods of Research
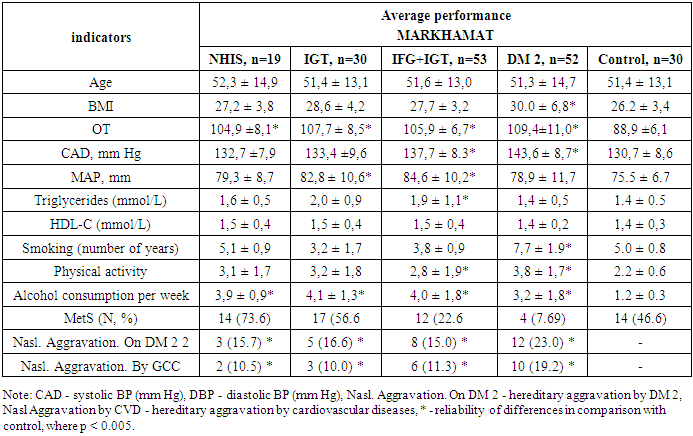
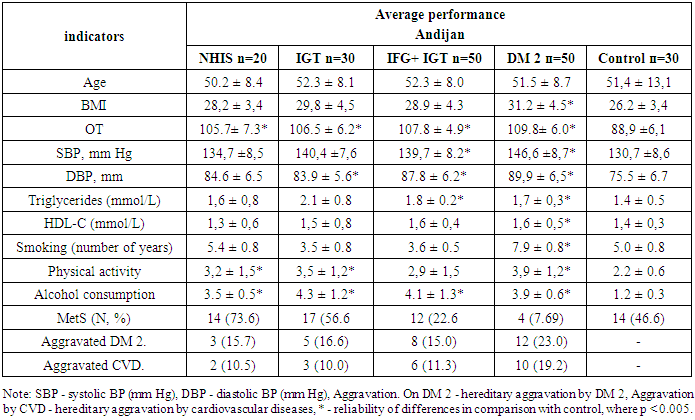
- The study was conducted on the basis of Andijan State Medical Institute. A total of 3400 persons of risk groups were examined, of which 1800 were residents of Markhamat district of Andijan region and 1600 residents of Andijan city. The control group consisted of 30 healthy individuals. Inclusion criteria: individuals over 20 years of age who were overweight, dyslipidemic, or hypertensive. Exclusion criteria: type 1 diabetes mellitus, other endocrine diseases, metformin use, severe autoimmune diseases, vasculitis, oncology. According to the design, the study was conducted in two phases.In Phase 1, according to the study design, cardiovascular risk factors including waist circumference, body mass index (BMI), blood pressure level, lipid profile, presence of diabetes mellitus and metabolic syndrome, and anamnestic information extracted from relevant medical records were analyzed. Patients were questioned using the Findrisk scale.At the 2nd stage, freshly collected biological material (venous blood) was collected and then promptly delivered to the laboratory for research.The study methods included general clinical approaches, biochemical testing (measurement of fasting blood glucose levels and two hours after meals, determination of glycated hemoglobin, bilirubin (both direct and indirect), as well as ALT, AST, PTI, coagulogram, C-reactive protein, urea, creatinine and lipid profile), hormonal tests (insulin and C-peptide levels in the blood as needed) and instrumental methods such as ECG, ultrasound of endocrine glands and internal organs, chest X-ray and other tests.Diabetes mellitus (DM) is diagnosed based on glucose levels 2 hours after a meal, as well as fasting glucose values or self-reported DM at initial screening. Impaired fasting glycemia (IFG) is defined as a fasting glucose level of 5.6 to less than 7.0 mmol/L and a 2-hour glucose level of less than 7.8 mmol/L. Impaired glucose tolerance (IGT) is defined as a 2-hour glucose level between 7.8 and less than 11.1 mmol/L. Both conditions, IFG and IGT, have boundaries corresponding to nondiabetic glucose levels both on an empty stomach and after 2 hours. Glucose dysregulation disorder (GDD) denotes the presence of IUGR or IGT, either alone or in combination.Hypertension was defined as mean blood pressure (with systolic pressure ≥140 mm Hg or diastolic pressure ≥90 mm Hg) or on the basis of self-reported presence of hypertension at baseline. Cardiovascular disease (CVD) was defined through self-reported diagnosis or medication use during the visit, and medical records were also reviewed when possible. This category included coronary heart disease and cerebrovascular disease. Coronary heart disease further included angina pectoris, myocardial infarction, coronary angiography abnormalities, cardiac procedures, and death due to or in combination with coronary heart disease. Cerebrovascular disease covered transient cerebral ischemic attack, stroke, cerebral infarction from any cause, and death associated with these conditions.Data were expressed as mean ± DM 2, n (%) or OR (95% CI), all statistical tests were two-sided, and a P value < 0.05 was considered statistically significant.
3. Results of the Study
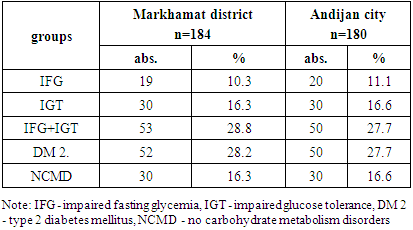
- Table 1 gives the distribution of patients of Markhamat district and Andijan city.
|
|
|
|
4. Conclusions
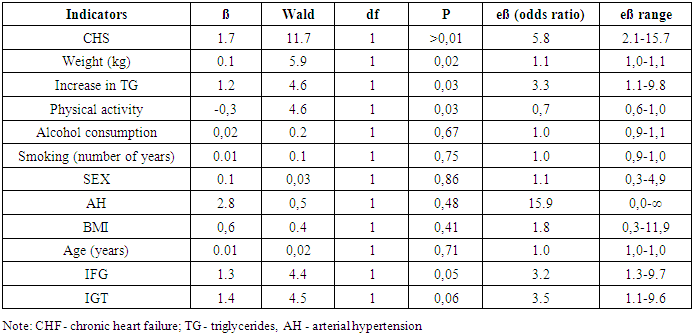
- 1. In this study, there was a significant difference in the cumulative prevalence of type 2 diabetes mellitus among the residents of Markhamat district and Andijan city, which was 7.3% and 8.7%, respectively.2. A binary logistic regression model with metabolic syndrome as the dependent variable showed a positive association with chronic heart failure, hereditary aggravation for type 2 diabetes mellitus and cardiovascular disease, weight, and physical activity. Gender, age, height, number of years of smoking, and reported alcohol consumption were not significantly associated.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML