-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1515-1518
doi:10.5923/j.ajmms.20251505.46
Received: Apr. 25, 2025; Accepted: May 23, 2025; Published: May 27, 2025

Clinical Differentiation Between COVID-19-associated Reactive Arthritis and Urogenital Etiology Classic Reactive Arthritis
Abdullaev Zh. U., Mirakhmedova Kh. T., Saidrasulova G. B.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

To evaluate clinical differences between reactive arthritis associated with COVID-19 and urogenital etiology. Materials and methods. The study included 195 patients. The first group consisted of 135 patients who had suffered COVID-19, the second group consisted of 60 patients with reactive arthritis of urogenital etiology. General clinical, laboratory and instrumental studies of patients were assessed. Results. It was found that the average age of patients in the first group is 1.45 times greater than in the second. In the study participated more women than men: in the first group there were 1.8 times more women than men. In contrast, in the second group there were 1.4 times more men than women. In the first group, the disease manifests predominantly in a polyarticular form, and in the second group - in a mono- or oligo-articular form. Conclusion. Reactive arthritis associated with COVID-19 occurs primarily in older adults, is relatively more common in women, and tends to be poly-articular form.
Keywords: COVID-19, Reactive arthritis, COVID-19 associated reactive arthritis, Urogenital etiology, Monoarthritis, Oligoarthritis, Polyarthritis, SARS-CoV-2 IgG
Cite this paper: Abdullaev Zh. U., Mirakhmedova Kh. T., Saidrasulova G. B., Clinical Differentiation Between COVID-19-associated Reactive Arthritis and Urogenital Etiology Classic Reactive Arthritis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1515-1518. doi: 10.5923/j.ajmms.20251505.46.
1. Introduction
- Coronavirus disease (COVID-19) is an infectious disease caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) virus [5]. SARS-CoV-2 affects people of all ages. However, patients older than 60 years and those with comorbid conditions are more likely to develop severe disease [3]. As with other respiratory diseases, patients with COVID-19 may experience various clinical symptoms in the musculoskeletal system. Arthralgia has been reported in more than 15% of patients with COVID-19, and myalgia in more than 45%. However, scientists have also emphasized that the extent of musculoskeletal damage is not related to the course and severity of COVID-19 [9]. However, the COVID-19 virus can trigger the production of various antibodies and cytokines in the body [15], and in patients with severe disease, autoantibodies against host cells may develop [14].There is also information about various diseases associated with COVID-19, such as antiphospholipid syndrome, myositis, and systemic lupus erythematosus. Recent research also investigates the development of reactive arthritis in COVID-19 patients.In their article, musculoskeletal injury in COVID-19: in Images, Chicago scientists studied muscles, nerves, joints, soft tissues, and bones using MRI, CT, and musculoskeletal ultrasound [8]. While signs of edema, necrosis, and atrophy were found in muscles, synovitis, and sometimes erosions were found in joints, hematoma, gangrene, COVID-finger, atypical ulcers, and signs of osteonecrosis and osteoporosis were found in soft tissues [9]. The most common symptom of the musculoskeletal system due to COVID-19 is myalgia, which is detected in almost 50% of patients [6]. Muscle damage is considered an important factor in the morbidity and mortality associated with RA [10]. Scientific sources from Indian scientists have highlighted the widespread involvement of the bone and joint system in COVID-19, similar to viral arthralgia [13]. Even after recovery from COVID-19, 27% of patients continued to have persistent joint pain [2].Post-COVID-19 disease has been associated with a high incidence of inflammatory arthritis. Ursini et al. reported that 51% of patients had asymmetric monoarthritis or oligoarthritis. Of these, 20% had RA-specific features and 11% had persistent axial symptoms [12]. Jacoppo et al. have suggested that post-COVID-19 syndrome may be a trigger for the development of inflammatory arthritis [4]. Some sources indicate that COVID-19 and its vaccine can also induce inflammatory arthritis [12] and various less severe systemic diseases such as vasculitis, Still's disease, and dermatomyositis [1].Three articles compared the clinical presentation, course, and laboratory parameters of COVID-19-associated reactive arthritis with arthritis of urogenital etiology.
2. Material and Methods
- The study was conducted in 2020-2024 at the Multidisciplinary Clinic of the Tashkent Medical Academy with the participation of patients who received inpatient and outpatient treatment in the departments of internal rehabilitation, rheumatology, cardiorheumatology and the Republican Rheumatology Center IADK. The study was carried out with a total of 195 participants. 135 patients with varying degrees of severity of COVID-19 and joint syndrome were selected for the study, and 60 patients with urogenital etiology diagnosed with ReA were chosen as the main group for comparison.One specific criterion for selecting patients for the study of joints in patients with COVID-19 was the presence of various degrees of severity of COVID-19 and joint syndrome after the disease, and the absence of other rheumatic diseases before being selected for the study.To confirm that patients with joint syndrome had been infected with COVID-19 and that joint syndrome was caused by SARS-CoV, SARS-CoV-2 IgG antibodies were detected in the blood serum. Patients with this antibody were included in the study. In group 2 patients, the detection of IgG to chlamydia and ureaplasma was one of the main criteria for confirming reactive arthritis of urogenital etiology. In addition, when selecting patients for the study of joint syndrome in patients with COVID-19, patients were excluded from the study in the following cases: with a history of other rheumatic diseases; patients with serologically positive results for chlamydia, ureaplasma, hepatitis B, C, AIDS; patients with positive serological markers such as RO, anti-ASSP, ANCA, ANA; patients with psoriasis or inflammatory bowel disease on examination or in history.Thus, patients aged 18-70 were selected for the study. Women who had recently given birth and were pregnant, patients with severe and very severe chronic heart, kidney, and liver failure, and patients with unstable general conditions were excluded from the study. In addition, patients receiving genetically engineered biological drugs (infliximab, adalimumab, etanercept, IL-17 inhibitors secukinumab, ixekizumab) and synthetic antirheumatic drugs (sulfasalazine, methotrexate, leflunomide, azathioprine) were also excluded from the study.Clinical, laboratory and instrumental examination methods were used in the general examination of patients. In the general clinical examination, the intensity of pain in the joints and the duration of morning stiffness were assessed using a visual analogue scale. Joint syndrome was assessed by the number of swollen joints, the number of painful joints. Laboratory examination methods included a complete blood and urine analysis, biochemical blood analysis, IgG chlamydia, ureaplasma; acute phase reactions: C-reactive protein (C-RP), rheumatoid factor - RF and ACCP, ANA (antinuclear antibody) to determine the presence of COVID-19 - IgG SARS-COV-2 was determined.
3. Results and Discussion
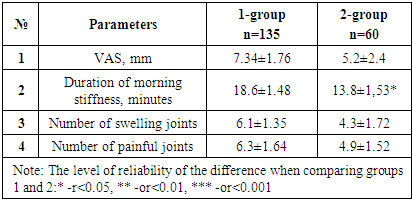
- The average age of the patients participating in the study was 46.25±7.6 (min-20, max-70 years). Group 1 patients were found to be 1.18 times larger than the general group and 1.45 times larger than group 2 patients (Figure 1).
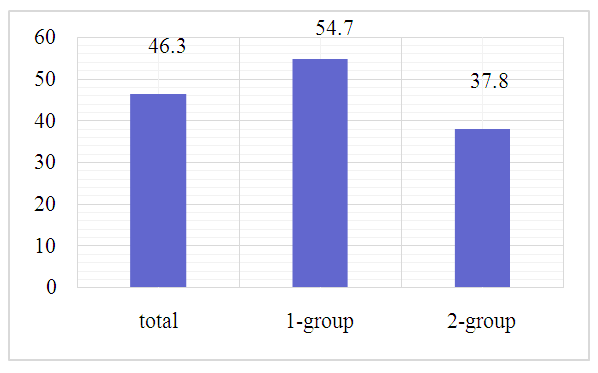 | Figure 1. Average age of patients participating in the study, years |
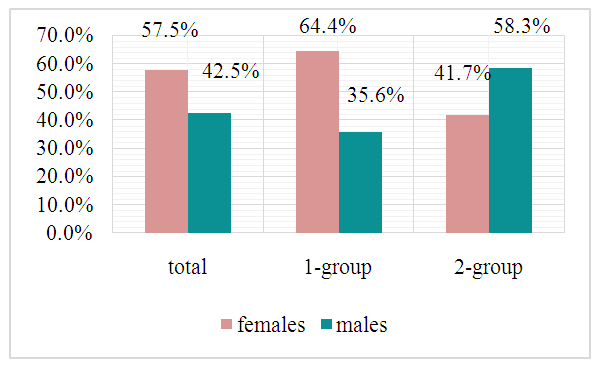 | Figure 2. Gender ratio of patients participating in the study |
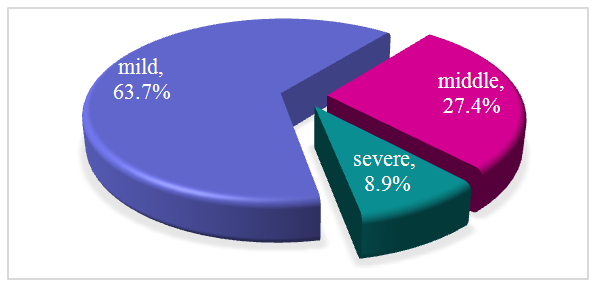 | Figure 3. Severity of COVID-19 by patient |
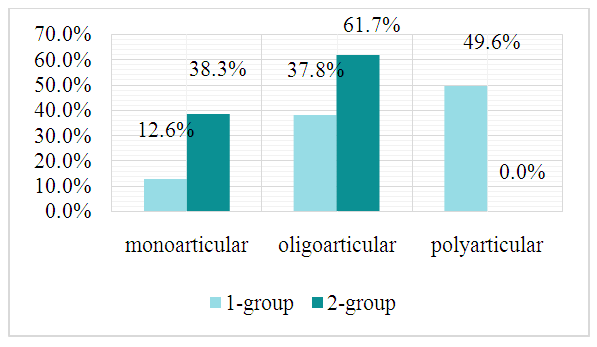 | Figure 4. Patterns of progression of reactive arthritis in patients |
|
4. Conclusions
- It is well known that arthritis of urogenital etiology occurs in a relatively young age group, affects men more often, and the disease has a mono-oligoarticular course. On the contrary, COVID-19-associated reactive arthritis occurs mainly in the elderly population, predominantly affects women, and has a tendency to polyarticular course, which is different from reactive arthritis of urogenital etiology in terms of its manifestation and course.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML