-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1500-1503
doi:10.5923/j.ajmms.20251505.43
Received: Apr. 25, 2025; Accepted: May 20, 2025; Published: May 27, 2025

Efficacy of Acne Therapy Considering the Genotypes of the C174G Polymorphism in the IL-6 Gene
Malikova Nilufar Nusratullayevna1, Arifov Saidkasim Saidazimovich2, Boboev Kodirjon Tukhtabaevich3
1PhD, Department of Dermatovenereology and Cosmetology of the Center for the Development of Professional Qualification of Medical Workers, Uzbekistan
2DSc., Professor, Head of the Department of Dermatovenerology and Cosmetology of the Center for the Development of Professional Qualification of Medical Workers, Uzbekistan
3DSc., Professor, Head of the Department of Medical Genetics and Cytogenetics of the Republican Specialized Scientific-Practical Medical Center of Hematology, Uzbekistan
Correspondence to: Malikova Nilufar Nusratullayevna, PhD, Department of Dermatovenereology and Cosmetology of the Center for the Development of Professional Qualification of Medical Workers, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Acne vulgaris is a multifactorial inflammatory skin condition influenced by genetic, hormonal, microbial, and environmental factors. Recent studies have highlighted the role of cytokine gene polymorphisms, particularly in interleukin-6 (IL-6), in modulating inflammatory responses and individual susceptibility to acne. To assess the efficacy of acne therapy in relation to the genotypes of the C174G polymorphism in the IL-6 gene and to determine the potential of genotype-guided treatment strategies. A total of 133 patients with acne and 125 conditionally healthy individuals were genotyped for the C174G polymorphism in the IL-6 gene using real-time PCR. Patients were divided into two treatment groups: one received standard therapy, and the other received a newly developed method involving pulsed dye laser, oral Toitriazoline, and topical agents. Treatment efficacy was evaluated in correlation with genotype distribution. The C allele frequency was significantly lower in the acne group compared to the control group (67.3% vs. 83.6%, p = 0.01), suggesting a protective role. The C/C genotype was associated with the highest rates of clinical remission, regardless of therapy type. The developed treatment method showed superior results in terms of remission and significant improvement, especially among carriers of the C/C genotype (p < 0.01). The IL-6 C174G polymorphism contributes to acne susceptibility and treatment response. Genotype C/C is protective, while C/G and G/G are associated with increased risk. Therapy tailored to genetic background, particularly the use of the developed method in C/C carriers, may improve treatment outcomes.
Keywords: Acne, Acne vulgaris, Gene polymorphism, IL-6 gene, Personalized therapy, Inflammation
Cite this paper: Malikova Nilufar Nusratullayevna, Arifov Saidkasim Saidazimovich, Boboev Kodirjon Tukhtabaevich, Efficacy of Acne Therapy Considering the Genotypes of the C174G Polymorphism in the IL-6 Gene, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1500-1503. doi: 10.5923/j.ajmms.20251505.43.
1. Introduction
- Acne (number: vulgare eels, eels, acne) - polymorphic multifactorial chronic disease of the sebaceous glands and hair follicles [8]. 80% of adolescents and young people have acne [1]. According to most researchers, acne occurs with similar frequency in both males and females, although more severe forms are more often observed in males [5,9].The etiology and pathogenesis of acne are not fully studied. In modern dermatology, the etiology and pathogenesis of acne are considered as interrelated mechanisms: hormonal imbalance and hypersecretion of skin fat, change in its chemical composition, follicular hyperkeratosis, microbial colonization Propionibacterium acnes (P. acnes) and inflammation [10]. The authors indicate that the antigens of microorganisms (P. acnes and P. granulosum) contribute to the attraction of neutrophils, phagocytes into the duct of the sulfured follicle. Neutrophils, on the one hand, stimulating the complement system, through Thall-like receptors (TLR2) promote the synthesis of interleukins (IL-8 and IL-12) and stimulate monocytes for the synthesis of IL-8, TNF-α, IL-1β, IL-6) [2,3].Studies by Polish researchers have shown that polymorphisms in cytokine genes such as C>T polymorphism in IL-1A may contribute to acne pathogenesis [6].Under the influence of anti-inflammatory cytokines, an increase in the activity of cyclooxygenase occurs, as a result of which a mediator of the inflammatory process is formed - leukotriene B4 from arachidonic acid. Leukotriene B4 is able to activate monocytes, eosinophils, T-lymphocytes and other. cells that secrete hydrolytic enzymes. The latter cause the destruction of the wall of the suet gland, which leads to its content entering into surrounding tissue and development of inflammatory process. Clinically, this manifests as papular-pustular and nodular lesions [4].Therefore, different expression of the genes of interleukins can be associated with pathogenesis, clinical course and acne treatment.Several studies have shown a strong correlation between IL-6 levels and acne severity, suggesting IL-6 as a potential marker for disease progression and therapeutic response. [12,11,7]. For example, there was a significant difference in IL-6 levels in the group of patients with and without acne (95% DI 55.1 - 155.3, p < 0.001). The correlation analysis of IL-6 levels with acne severity was strictly positive (r = 0.951, p 0.001) [7].Therefore, the aim of this work was to analyze the efficacy of therapy taking into account the C174G (rs1800795) polymorphism genotypes of the IL6 gene.
2. Materials and Methods
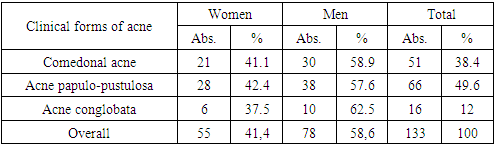
- We clinically monitored 133 acne patients aged 11 to 35 years. The average age was 19.8 + -1.3. There were 78 (58.6%) men and 55 (41.4%) women. The distribution of patients by clinical forms of acne is presented in table 1 (according to Plewig G., et al. 2000).
|
3. Results and Discussion
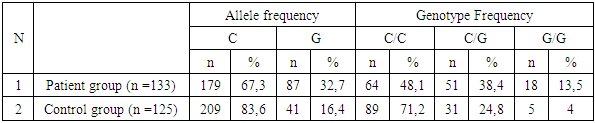
- The analysis of allele and genotype frequency distribution of the C174G polymorphism in the IL-6 gene revealed statistically significant differences between the study groups. The C allele was found significantly less frequently in the patient group — 67.3%, compared to 83.6% in the control group (χ² = 18.4; p = 0.01; OR = 0.4; 95% CI: 0.27–0.61). These findings suggest a potential protective effect of the C allele against the studied condition.The G allele was predominant in the patient group, accounting for 32.7%, compared to 16.4% in the control group (χ² = 18.4; p = 0.01; OR = 2.5; 95% CI: 1.64–3.75). The distribution frequencies of alleles and genotypes of the C174G polymorphism in the IL-6 gene among the acne patient group, its subgroups, and the control sample are presented in Table 2.
|
|
|
|
4. Conclusions
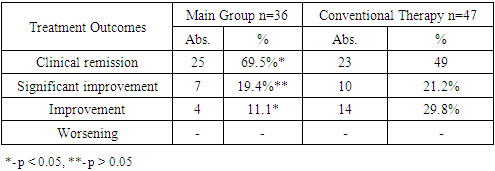
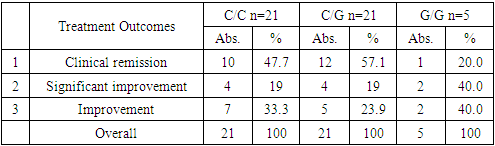
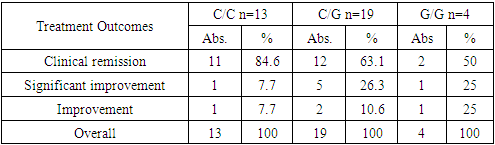
- A comparative analysis of the study results revealed that the best clinical outcomes were observed in patients with the protective C/C genotype, regardless of the treatment method used. Moreover, in terms of clinical remission and the overall positive outcome (defined as clinical remission plus significant improvement), the proposed therapy method demonstrated a statistically significant advantage over the conventional treatment (p < 0.01).Thus, the C174G polymorphism of the IL-6 gene plays a role in the predisposition to and regulation of the inflammatory process in acne. The C/C genotype exerts a protective effect, whereas the risk of developing acne increases 1.5-fold in carriers of the heterozygous C/G genotype and 3.4-fold in those with the homozygous G/G genotype. Treatment effectiveness is higher in carriers of the favorable genotype, regardless of the therapy method applied. The effectiveness of therapy was consistently higher among patients carrying the favorable C/C genotype, regardless of the treatment method applied. However, the developed treatment method which included pulsed dye laser therapy, oral Toitriazoline, and topical agents demonstrated a statistically significant improvement in clinical remission and overall positive outcomes (p < 0.01) compared to conventional therapy.These results suggest that genotyping for the C174G polymorphism in the IL-6 gene may serve as a valuable predictive tool in both assessing acne susceptibility and optimizing personalized treatment strategies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML