-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1460-1462
doi:10.5923/j.ajmms.20251505.32
Received: Apr. 13, 2025; Accepted: May 11, 2025; Published: May 24, 2025

Morphological Analysis of Pseudoarthrosis in the Tibia: Vascular and Histological Perspectives
Mannonov Anvar Abduvakil Ugli1, Mamadiyarova Dilfuza Umirzakovna2
1Samarqand Davlat Tibbiyot Universiteti Patologik Anatomiya Kafedrasi Mustaqil Ilmiy Xodimi, O'zbekiston
2Samarqand Davlat Tibbiyot Universiteti Pedagogika va Psixologiya Kafedrasi Dotsenti, O'zbekiston
Correspondence to: Mannonov Anvar Abduvakil Ugli, Samarqand Davlat Tibbiyot Universiteti Patologik Anatomiya Kafedrasi Mustaqil Ilmiy Xodimi, O'zbekiston.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Surgical materials of 45 patients of different ages who underwent surgery for pseudoarthrosis of the tibia were subjected to pathomorphological examination. It was found that in the formation of pseudoarthrosis of the tibia, not only the blood vessels supplying the bone with blood, but also the state of the blood vessels of the surrounding tissues play an important role. One of the important factors leading to the formation of pseudoarthrosis is a long-term violation of hemodynamics in the bones and surrounding tissues, especially after post-traumatic fractures.
Keywords: Tibia, Pseudoarthrosis, Epiphysis, Diaphysis, Artery, Periosteum
Cite this paper: Mannonov Anvar Abduvakil Ugli, Mamadiyarova Dilfuza Umirzakovna, Morphological Analysis of Pseudoarthrosis in the Tibia: Vascular and Histological Perspectives, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1460-1462. doi: 10.5923/j.ajmms.20251505.32.
1. Introduction
- Congenital pseudarthrosis of the tibia is often associated with neurofibromatosis-1, an autosomal dominant disorder with a frequency of 1 in 4000 births. About 40 to 80% of cases of CPT are neurofibromatosis-1 carriers, but less than 4% of cases of neurofibromatosis-1 show the presence of CPT and bowing of the tibia [4]. The treatment of atrophic pseudoarthrosis with bone and soft tissue defects is particularly challenging and places high demands on reconstructive orthopedic and trauma surgery [9,7]. Atrophic pseudoarthrosis is associated not only with bone loss but also with trophic changes in soft tissues, which can lead to fracture stability and limb loss. In addition, the inability to save the limb can even lead to fatal consequences [3,6]. Due to prolonged hospitalization, delayed treatment, and the need for bone and soft tissue reconstruction, multiple surgical procedures, as well as loss of function of the affected limb, affect the quality of life of patients with health-related problems [8,10,11].Research objective: To identify pathomorphological changes in the structures of pseudoarthrosis of the tibia.
2. Materials and Methods
- The surgical materials of 45 patients of different ages who underwent surgery for false joint of the tibia at the Department of Pathological Anatomy of the Multidisciplinary Clinic of Samarkand State Medical University were subjected to macroscopic and microscopic examination. Of these, 38 were men (84%), 7 (16%) were women. Of these, 21 were 25-44 years old (young people) with an average time of injury and surgery of 6±2.0 months, 13 were 45-59 years old (middle-aged people) with an average time of injury and surgery of 10±2.0 months, and 4 were 60-70 years old (elderly people) with an average time of injury and surgery of 12 months or more. Bone tissues were decalcified in 10% nitric acid, and paraffin blocks were prepared from them. Sections 3-6 μm thick were taken and stained with hematoxylin-eosin. Morphological analysis of micropreparations was performed. Histological preparations were studied and photographed using a LeicaGME microscope (Leica, India) and a LeicaEC3 digital camera (Leica, Singapore) and a Pentium IV computer. Photo processing was performed using Windows Professional programs.
3. Results and Discussion
- It is known that the blood vessels of the periosteum are supplied with blood through blood vessels branching from the branches of the muscular and facial arteries. The vascular branches form peculiar tangles in the periosteum, from which small branches enter the compact layer of the bone through the channels. Some of them reach the endosteum and bone marrow. The tibia is supplied with blood from 3 sources (feeding artery, periosteal network and epiphyseal vessels). The diaphyseal zone is supplied with blood mainly through the periosteal network and intraosseous arteries. Arterial anastomoses are poorly developed in the epiphyseal and diaphyseal parts. The periosteal blood vessels are located less frequently in them than in the metaphyseal part. Pseudoarthrosis - we detect spasmodic blood vessels in the soft tissues around the joint, swelling of endothelial cells and pyknotic state of the nuclei. Sclerotic processes develop in the periosteum and walls of blood vessels within the bone of pseudo-joints that have not been eliminated for a long time (Figure 1, 2).
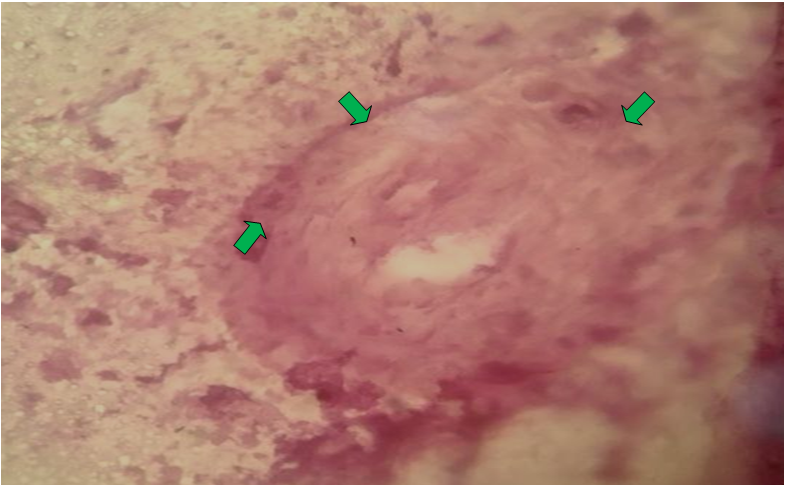 | Figure 1. Advanced sclerotic process of blood vessels in the periosteum. Stained with hematoxylin-eosin. Objective-40, eyepiece-10 |
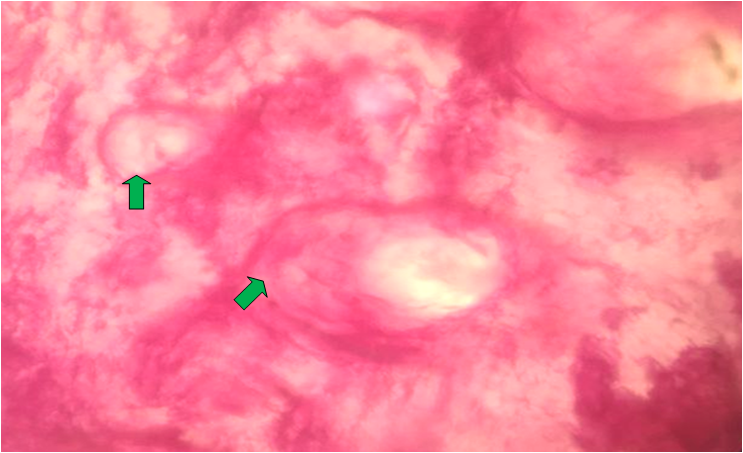 | Figure 2. Sclerotic process of the blood vessels of the periosteum. Stained with hematoxylin-eosin. Objective-40, eyepiece-10 |
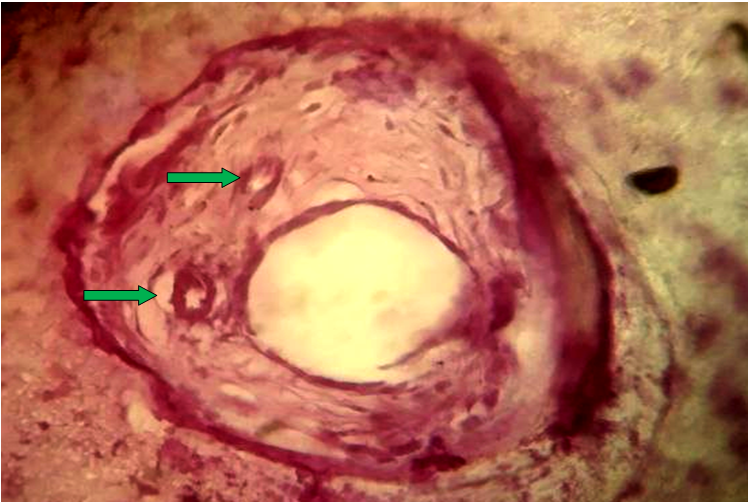 | Figure 3. Revascularization process in the pseudoarticular areas of the tibia. Stained with hematoxylin-eosin. Objective-40, eyepiece-10 |
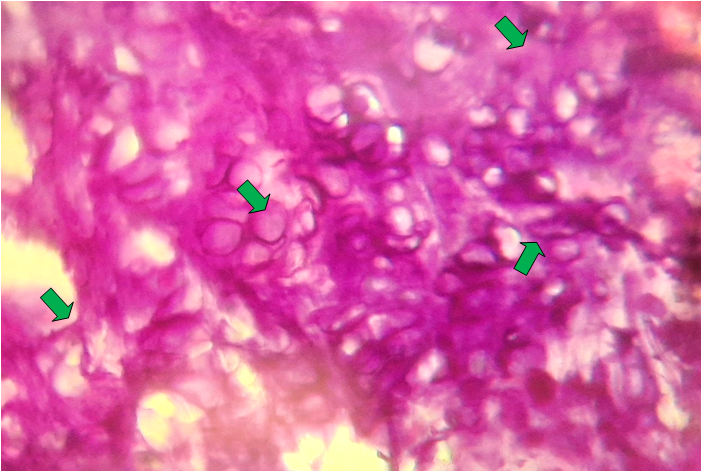 | Figure 4. Cartilage tissue (chondrocytes) in the area of pseudoarthrosis of the tibia. Stained with hematoxylin-eosin. Objective-40, eyepiece-10 |
4. Conclusions
- Thus, in the formation of pseudoarthrosis, not only the blood vessels supplying the bone with blood, but also the state of the blood vessels of the surrounding tissues play an important role. One of the important factors leading to the formation of pseudoarthrosis, especially after post-traumatic fractures, is a prolonged violation of hemodynamics in the bones and surrounding tissues. Sclerotic processes develop in the periosteum and walls of the intraosseous blood vessels of pseudo-joints, where the blood vessels of the bone have not been eliminated for a long time. Around them and between them, an increase in fibrous tissue cells is noted. Also, hypervascularization is noted in the areas where the bone mass is formed. Such hemodynamic disturbances should be taken into account in treatment measures.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML