-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1445-1447
doi:10.5923/j.ajmms.20251505.27
Received: Apr. 18, 2025; Accepted: May 16, 2025; Published: May 24, 2025

Pathomorphical Aspects of Changes in the Placenta and Adjacent Uterine Structures During the Attachment of the Fetal Maternity Tissue to the Myometric and Serosa of the Uterus
Davronov Otabek To’ramurodovich1, Mamadiyarova Dilfuza Umirzakovna2
1Independent Researcher of the Department of Pathological Anatomy of Samarkand State Medical University, Uzbekistan
2Associate Professor, Department of Pedagogy and Psychology, Samarkand State Medical University, Uzbekistan
Correspondence to: Davronov Otabek To’ramurodovich, Independent Researcher of the Department of Pathological Anatomy of Samarkand State Medical University, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In order to determine the pathomorphological aspects of changes in the placenta and adjacent uterine structures when placental tissue adheres to the uterine myometrium and serosa, tissue fragments removed from the uterus of 26 women with uterine atony caused by the ingrowth of placental tissue into the myometrium were subjected to pathomorphological examination. It was found that in the part where the placental tissue has grown into the myometrium and serosa of the uterus, large foci of fibrinoid necrosis and proliferation of syncytiotrophoblasts and morphological signs of chronic placentitis are detected. Swelling and hemorrhagic imbibition are noted in the myometrium. Swelling and sclerotic changes are observed in the serosa.
Keywords: Uterus, Placenta, Myometrium, Serosa, Ingrowth, Sclerosis
Cite this paper: Davronov Otabek To’ramurodovich, Mamadiyarova Dilfuza Umirzakovna, Pathomorphical Aspects of Changes in the Placenta and Adjacent Uterine Structures During the Attachment of the Fetal Maternity Tissue to the Myometric and Serosa of the Uterus, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1445-1447. doi: 10.5923/j.ajmms.20251505.27.
1. Introduction
- True adhesion of the placenta to the myometrium is a serious complication of pregnancy and is associated with the risk of developing massive uterine bleeding if the tactics of management of pregnant women and childbirth are incorrectly chosen. The steady increase in the incidence of this pathology from year to year is especially noteworthy. The incidence of placental ingrowth into the myometrium varies from 0.04 to 0.2% of all newborns [1,2]. Depending on the depth of penetration of the chorionic villi into the myometrium, there are different types of placental adhesion: placenta accreta (superficial invasion of the chorionic villi), placenta increta (deep invasion of the chorionic villi) and penetration of the chorion through the entire wall of the uterus (placenta) [4]. The depth and area of placenta accreta are the main factors determining surgical tactics and the degree of surgical intervention [4,5]. From the mid-20th century to the present, the incidence of abnormal placental attachment (accretion) has increased tenfold: from 1:25,000–50,000 births to 1:500–1000 at present, and in specialized centers — up to 1:343 [6]. Such dynamics of the process is explained by the progressive increase in the incidence of operative abdominal births. The International Federation of Obstetricians and Gynecologists (FIGO) publishes strong epidemiological evidence that placenta accreta has now essentially become an iatrogenic condition as a result of the increase in the incidence of cesarean sections worldwide [7].The purpose of the study: To determine the pathomorphological aspects of changes in the placenta and adjacent uterine structures during the attachment of placental tissue to the uterine myometrium and serosa.
2. Materials and Methods
- Uteruses removed from 26 women in maternity hospitals in Samarkand due to uterine atony caused by placental tissue growing into the myometrium were studied at the Department of Pathological Anatomy of the Multidisciplinary Clinic of Samarakand State Medical University. Morphological and morphometric changes in the structures of the uterine myometrium were examined using macroscopic, microscopic, morphometric and statistical methods. Histological sections were stained with hematoxylin-eosin. Hematoxylin and eosin staining procedure:It is the most widely used method for staining histological sections.Sections are deparaffinized in chloroform, washed in distilled water, then a solution of hematoxylin is dripped onto the surface of the section and fixed for 3 minutes. It is washed in running water for 10 minutes and stained with eosin for 0.2 to 3 minutes. Dehydrated in 70° and 96° alcohol, transferred to carbol-xylene and xylene and covered with balsam. Result: cell nuclei are stained blue-black, cytoplasm - dark purple. Histological preparations were studied and photographed using a LeicaGME microscope (Leica, India) coupled with a LeicaEC3 digital camera (Leica, Singapore) and a Pentium IV computer. Photo processing was carried out using Windows Professional applications. Gallbladder adenoma was morphologically evaluated in prepared micropreparations.
3. Results and Discussion
- The results of the study show that 1 of 32 women had a history of intrauterine infection in their I pregnancy and I delivery. 6 had a history of chronic endometritis, intrauterine infection, and glandular hyperplasia of the endometrial layer in their II pregnancy and II delivery. 9 had a history of III pregnancy and III delivery, most of whom received treatment for intrauterine infection and adenomyosis. 6 had a history of IV pregnancy and II-III-IV delivery, and their history was determined to have submucosal myoma of the uterine body, and the remaining 3 had V-VI pregnancies and deliveries, and their history was recorded as pathological conditions such as chronic endometritis, endometriosis, and glandular hyperplasia. Microscopic examination of histological preparations prepared from the removed uterus reveals deep ingrowth of placental tissue into the uterine myometrium, engorgement of myometrial blood vessels in this area, development of sclerotic processes in the blood vessel walls, and hemorrhagic imbibition (Figure 1).
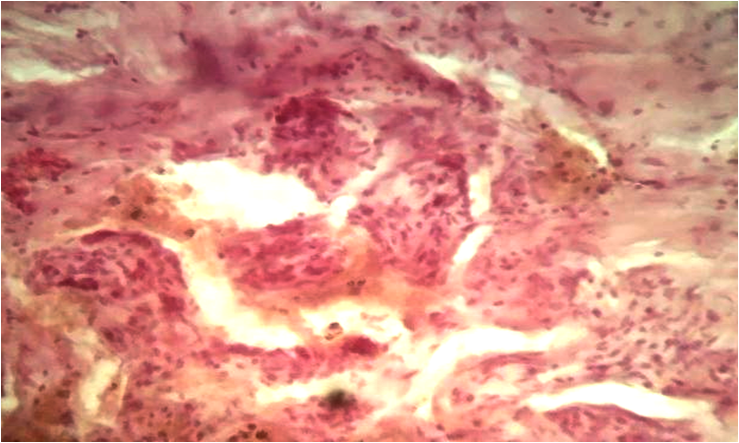 | Figure 1. True ingrowth of placental tissue into the uterine myometrium, hemorrhagic imbibition. Stained with hematoxylin-eosin. Ob.40, ok.10 |
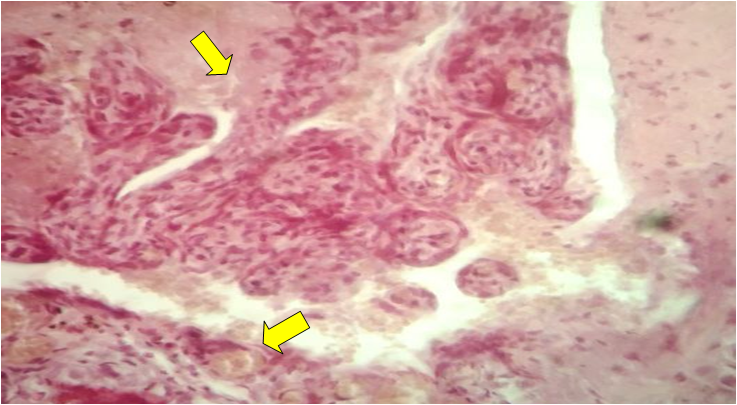 | Figure 2. Invasion of placental tissue into the uterine myometrium, vascularity. Stained with hematoxylin-eosin. Ob.40, ok.10 |
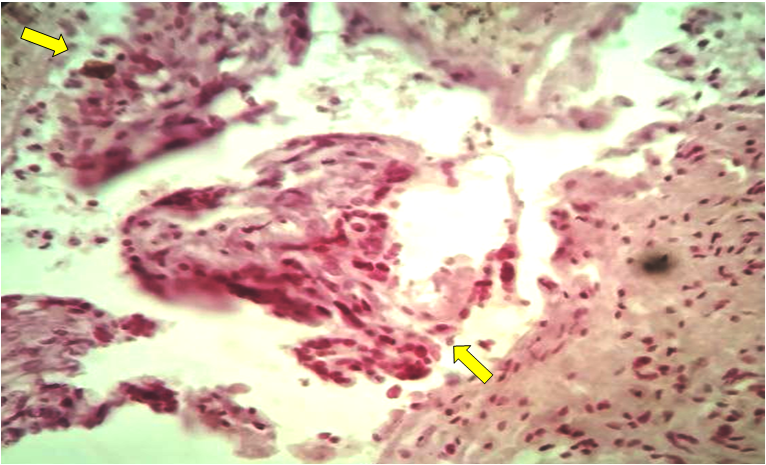 | Figure 3. Growth of terminal villi of placental tissue growing into the myometrial layer, proliferation of syncytiotrophoblasts. Hemorrhagic imbibition. Stained in hematoxylin-eosin. Ob.40, ok.10 |
4. Conclusions
- Thus, in the part of the placental tissue that has grown into the myometrium and serosa of the uterus, large foci of fibrinoid necrosis and proliferation of syncytiotrophoblasts and morphological signs of chronic placentitis are detected. Edema and hemorrhagic imbibition are noted in the myometrium. Edema and sclerotic changes are observed in the serosa.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML