-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1407-1410
doi:10.5923/j.ajmms.20251505.19
Received: Apr. 14, 2025; Accepted: May 9, 2025; Published: May 15, 2025

Comparing of Monotherapy and Combination Therapy Effect on 24-Hour Profile of Blood Pressure in Glomerulonephritis
M. R. Ruzikulova, B. F. Mukhammedova, D. E. Abdujabborova
Republican Research Center of Emergency Medicine Tashkent, Uzbekistan
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to evaluate the effect of lisinopril and irbesartan monotherapy and combined therapy on the 24-hour blood pressure profile in patients with glomerulonephritis. Introduction. Arterial hypertension is one of the leading causes of cardiovascular disease affecting both adults and the elderly. In the group of patients with glomerulonephritis, symptomatic arterial hypertension is quite common and is a major factor in worsening the prognosis. Previous studies have shown that combined therapy with lisinopril and irbesartan may have a more efficient impact on the 24-hour blood pressure profile and improve nocturnal BP lowering compared with monotherapy. Material and Methods. 90 patients with chronic glomerulonephritis and lupus nephritis diagnosed with symptomatic arterial hypertension were included for the study. The mean age of the patients was 45 years (±10 years). All patients underwent a comprehensive evaluation including clinical examination, laboratory tests, and daily blood pressure monitoring. Results. The results of 24-hour blood pressure monitoring showed that the majority of patients (54.4%) had a “night-peaker” diurnal profile, i.e., with an increase in blood pressure at night. In 49.6% of cases, patients did not have a normal nighttime blood pressure drop, which corresponded to the non-dipper profile. Discussion. The results of this study showed that combination therapy with lisinopril and irbesartan has significantly greater efficiency in normalizing the diurnal blood pressure profile than monotherapy with each of these drugs. It was particularly shown to improve nocturnal reduction of blood pressure, which was critical for preventing the progression of renal failure and other organ lesions. Conclusions. Combined therapy with lisinopril and irbesartan is more efficient for normalizing the 24-hour blood pressure profile in patients with symptomatic hypertension and glomerulonephritis. Nighttime blood pressure reduction is important for prognosis and prevention of organ lesions, especially in the combined therapy group.
Keywords: Symptomatic arterial hypertension, Glomerulonephritis, Combined therapy, Lisinopril, Irbesartan
Cite this paper: M. R. Ruzikulova, B. F. Mukhammedova, D. E. Abdujabborova, Comparing of Monotherapy and Combination Therapy Effect on 24-Hour Profile of Blood Pressure in Glomerulonephritis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1407-1410. doi: 10.5923/j.ajmms.20251505.19.
Article Outline
1. Introduction
- Arterial hypertension (AH) is one of the leading causes of cardiovascular disease affecting both adults and the elderly. Its treatment is especially relevant in patients with chronic kidney disease, such as glomerulonephritis (GN), as this pathology is closely associated with the development of arterial hypertension, which, in turn, contributes to the progression of renal failure and increases the risk of cardiovascular complications. In a group of patients with glomerulonephritis, symptomatic arterial hypertension (SAH) is quite common and is a major factor in worsening prognosis [1].Various classes of antihypertensive drugs are used to treat SAH, among which ACE inhibitors and angiotensin II receptor antagonists (ARA II) are the most commonly used. Lisinopril and irbesartan, two widely used drugs from these groups, have different action mechanisms, but both efficiently lower blood pressure and have potential in slowing the progression of renal failure in patients with GN and SAH. However, it is still unclear how efficient they are in influencing the diurnal BP profile, especially the nocturnal BP decline, which is an important indicator for prognosis in patients with hypertension [2] [3].The diurnal BP profile is a dynamic characteristics of BP fluctuations over a 24-hour period. Its estimation is important because insufficient nocturnal BP reduction (the so-called “non-dipper” profile) may be associated with an increased risk of stroke, myocardial infarction and progressive renal failure. Thus, it is important not only to reduce BP levels but also to normalize the diurnal BP profile to achieve optimal therapeutic effects [4] [5]. In this regard, the study of the impact of different antihypertensive drugs on the daily BP profile in patients with glomerulonephritis is of particular importance.A previous studies have shown that combined therapy with lisinopril and irbesartan can more efficiently affect the diurnal BP profile and improve nocturnal BP lowering compared with monotherapy [6]. At the same time, existing data on how the combination of these drugs affects nocturnal and daytime BP in patients with SAH remain limited. It is well established that lisinopril and irbesartan lower BP but do not always provide normalization of the nocturnal BP profile, which represents an important challenge for further research in this area [7].Thus, this study aims to evaluate the effect of lisinopril and irbesartan monotherapy and combined therapy on the daily BP profile in patients with glomerulonephritis, which will help to expand the understanding of more efficient approaches to the treatment of SAH in this category of patients and minimize the risk of the disease progression.The aim of the study was to evaluate the effect of lisinopril and irbesartan monotherapy and combined therapy on the 24-hour blood pressure profile in patients with glomerulonephritis.
2. Material and Methods
- 90 patients with chronic glomerulonephritis and lupus nephritis diagnosed with symptomatic arterial hypertension were included for the study. The entire patient selection and research methods were conducted in accordance with ethical standards. The mean age of the patients was 45 years (±10 years). All patients underwent a comprehensive evaluation including clinical examination, laboratory tests, and daily blood pressure monitoring.The criteria for inclusion of patients in the study were as follows:• Diagnosis of symptomatic arterial hypertension based on clinical data.• Confirmed diagnosis of glomerulonephritis (chronic or lupus nephritis).• No contraindications to the use of lisinopril and irbesartan.• Patient consent to participate in the study.Exclusion criteria were as follows:• Acute cardiovascular diseases. • Azotemia (creatinine >0.3 mmol/l).• Allergy to drugs or their components.Patients were divided into three groups: • Group I (n=30) received lisinopril monotherapy at a dose of 20-40 mg/day.• Group II (n=30) patients were treated with irbesartan at a dose of 150-300 mg/day.• Group III (n=30) patients received combined therapy: lisinopril 20 mg/day and irbesartan 150 mg/day.The drugs were administered for 4 months. For BP monitoring, an automatic device for daily BP monitoring (DMBP) was used, which measured BP every 20 minutes during the day and every 30 minutes during the night. All the patients underwent repeated daily BP monitoring at the beginning and at the end of the study to evaluate the dynamics of changes.SPSS statistical program was used for data processing. All results were expressed as mean values ± standard deviation (SD). The Mann-Whitney test was used to estimate differences between groups, and the Pearson correlation coefficient was used to estimate correlation. A value of p < 0.05 was considered statistically significant.
3. Results
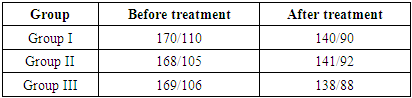
- The results of diurnal BP monitoring showed that the majority of patients (54.4%) had a “night-peaker” diurnal profile (with an increase in BP at night). In the group with hypertension at glomerulonephritis, this phenomenon had a significant impact on the progression of renal and other target organ lesions. In 49.6% of cases, patients did not have a normal nocturnal BP drop, which corresponded to the “non-dipper” profile.In the lisinopril group (Group I), a significant reduction in both daytime and nighttime BP was observed, with normalization of systolic (SBP), diastolic (DBP), and mean BP (mBP). However, nocturnal peak of BP persisted in the majority of patients. Daily BP variability was reduced, but not as efficient as with combination therapy (Group III).The results with irbesartan treatment (Group II) were similar to those with lisinopril one. The diurnal BP profile was improved, but patients continued to have elevated nocturnal BP values, which also reflected a lack of normalization of nocturnal hypertension.Combined therapy with lisinopril and irbesartan gave the best results (Group III). The daily BP profile in these patients became more normalized, with 66.7% of patients achieving a “dipper” profile. This phenomenon indicates normalization of the nocturnal decrease of BP and reduction of cardiovascular workload. BP variability was significantly reduced, and values returned to normal at the end of therapy (Tab. 1).
|
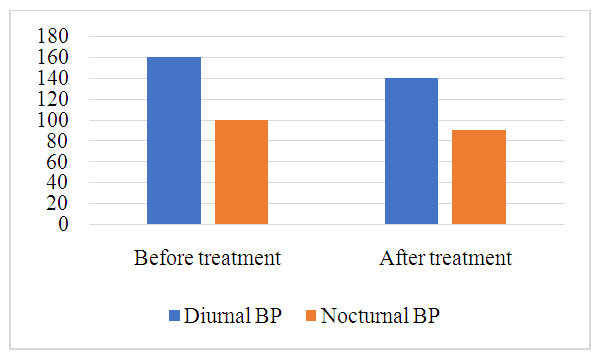 | Figure 1. The decrease of daily BP profile in the Group III |
4. Discussion
- The results of this study showed that combination therapy with lisinopril and irbesartan had significantly greater efficiency in normalizing the daily blood pressure profile than monotherapy with each of these drugs. Particularly, it was seen in the improvement of nocturnal BP reduction, which was critical for preventing the progression of renal failure and other organ lesions. It is supported by numerous studies which note that inadequate nocturnal BP lowering (“non-dipper” profile) is associated with worse prognosis in patients with hypertension, especially those ones with chronic kidney disease [8].In our study we found that patients who received monotherapy with lisinopril or irbesartan had a significant improvement of diurnal BP. However, despite this, nocturnal blood pressure remained elevated in most of them. It indicates continued hypertension at night, which may be due to the lack of effect of monotherapy on the nocturnal pressure profile. This phenomenon is supported by the results of other studies that indicate a more pronounced efficiency of combination therapy in normalizing nocturnal BP, which is important for preventing organ lesions such as left ventricular hypertrophy or progression of renal failure [9].In the lisinopril and irbesartan combined therapy group, nocturnal BP was normalized in the majority of patients. It emphasizes the more comprehensive effects of the drugs, which not only lower BP but also affect BP variability, providing a more stable and safer course of the disease. As other authors have noted, normalization of nocturnal BP can significantly improve clinical outcomes in patients with arterial hypertension and chronic kidney disease, reducing the risk of cardiovascular diseases and progression of renal failure [10].However, when using combined therapy, it is important to consider the possibility of side effects. There was an increase in the frequency of dry cough in the combined therapy group compared to monotherapy group in our study. This side effect is a known side effect of ACE inhibitors such as lisinopril and requires careful monitoring of the patient's condition. Similar results were obtained in other clinical studies, where the use of combinations of ACE inhibitors and ARBs was associated with an increased incidence of adverse reactions such as cough and hyperkalemia [8]. This highlights the importance of an individual approach to therapy, as well as the need for regular monitoring of patients' condition in order to minimize risks and select the best therapeutic strategy.Thus, combined therapy with lisinopril and irbesartan has a significant advantage in improving the diurnal BP profile, especially in normalizing the nocturnal BP decline, which is important for long-term control of arterial hypertension and preventing the progression of organ lesions. However, side effects remain an important aspect, requiring close monitoring and treatment adjustments if necessary.
5. Conclusions
- Combined therapy with lisinopril and irbesartan is more efficient in normalizing the daily BP profile in patients with symptomatic hypertension and glomerulonephritis.Nocturnal BP lowering is important for prognosis and prevention of organ lesions, especially in the combined therapy group.Monotherapy with lisinopril or irbesartan also lowers BP but does not provide optimal nocturnal BP reduction.Side effects such as dry cough require extra attention when prescribing combined therapy.
Ethical Approval and Consent to Participate
- Our institution's Research Ethics Board does not require review or approval of case reports. Our research was conducted in accordance with the World Medical Association Code of Ethics (Declaration of Helsinki).
Conflict of Interests
- The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
ACKNOWLEDGEMENTS
- The authors express their gratitude to the management of the multidisciplinary clinic of Republican Research Center of Emergency Medicine for the material provided for our study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML