-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1398-1402
doi:10.5923/j.ajmms.20251505.17
Received: Feb. 9, 2025; Accepted: Mar. 11, 2025; Published: May 13, 2025

Dental Examination of Deaf and Mute Children: Experience and Study Results in the Bukhara Region
Yuldashev Forrux Farxod Ugli1, Quryozov Akbar Quramboyevich2, Khabibova Nazira Nasulloevna3
1Department of Stomatology, Urganch Branch of the Tashkent Medical Academy, Uzbekistan
2PhD, Department of Stomatology, Urganch Branch of the Tashkent Medical Academy, Uzbekistan
3DSc, Professor, Bukhara State Medical Institute Department of Therapeutic Stomatology, Uzbekistan
Correspondence to: Khabibova Nazira Nasulloevna, DSc, Professor, Bukhara State Medical Institute Department of Therapeutic Stomatology, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

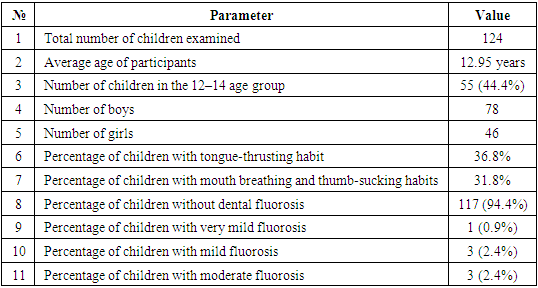
Introduction: The article analyzes the findings of a cross-sectional study conducted at the Department of Dentistry of the Bukhara State Medical Institute. The study aimed to assess oral health and treatment needs among children with hearing and speech impairments. The sample included 124 students from specialized boarding schools in the Bukhara region, comprising 78 boys and 46 girls aged 6 to 18 years, with an average age of 12.95 years. A cross-sectional study was conducted to evaluate the oral health status and treatment needs of children with hearing and speech impairments at the Department of Dentistry, Bukhara State Medical Institute. Results: Table 1 presents the sociodemographic characteristics of the study participants. The study involved 124 schoolchildren with hearing and speech impairments aged 6 to 18 years, with a mean age of 12.95 years. Conclusion: Children with hearing and speech impairments show higher caries prevalence, poorer periodontal health, and greater unmet dental care needs compared to healthy children.
Keywords: Children, Hearing impairment, Speech impairment, Oral health, Dental examination, Treatment needs, Specialized schools, Bukhara region, Disabilities, Clinical diagnostics, Questionnaires, Demographics
Cite this paper: Yuldashev Forrux Farxod Ugli, Quryozov Akbar Quramboyevich, Khabibova Nazira Nasulloevna, Dental Examination of Deaf and Mute Children: Experience and Study Results in the Bukhara Region, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1398-1402. doi: 10.5923/j.ajmms.20251505.17.
Article Outline
1. Introduction
- Oral health, as an integral part of overall health, significantly impacts a person’s general well-being [1]. Oral and dental diseases affect various aspects of quality of life, with their influence being particularly pronounced among individuals with systemic disorders or specific conditions [2]. In 2000, the Director-General of the World Health Organization (WHO) emphasized the need for equity in health access. However, persons with disabilities have historically faced discrimination, limiting their participation in societal and social activities [3].A child with a disability is defined as an individual who, due to their physical limitations, is unable to fully participate in age-appropriate activities [4]. According to WHO estimates from 2018, over 466 million people worldwide experience hearing loss, including 34 million children [5]. In India, based on the 2011 census, more than 3 million individuals suffer from hearing impairments, while over 1.2 million face speech disabilities [6]. Hearing loss impacts the ability to interpret speech sounds, leading to delays in language development, communication barriers, and economic, educational, and social inequities [7]. Visual impairments range from low vision to total blindness, defined as a visual acuity of less than 3/60 or a visual field reduction to less than 10 degrees in the better eye with best correction [8]. Among the 38 million blind individuals globally, approximately 6 million reside in India [9].Oral diseases can have a destructive impact on individuals with systemic conditions [10]. Dental care remains the most unmet healthcare need for children with disabilities, as their families are often emotionally, physically, and financially focused on managing the child’s primary medical condition, leaving oral health issues neglected [11]. Barriers to receiving dental care include treatment costs, accessibility, fear of procedures, and insufficient awareness of dental needs among children and their parents [12].Children with hearing, speech, or visual impairments face a higher risk of oral health issues, posing unique challenges in their dental management. This underscores the necessity of well-planned preventive strategies with a focus on primary prevention by primary healthcare providers [13]. These children often exhibit poorer oral hygiene and higher prevalence of gum diseases and dental caries. Effective evaluation of their oral health needs can enhance the accessibility of primary healthcare, which is considered the foundation of an efficient healthcare system, leading to improved oral health outcomes. Therefore, the present study aims to assess the oral health status, treatment needs, knowledge, attitudes, and oral hygiene practices among hearing-impaired children in the Bukhara region.
2. Methodology
- A cross-sectional study was conducted to evaluate the oral health status and treatment needs of children with hearing and speech impairments at the Department of Dentistry, Bukhara State Medical Institute.The study included children from two specialized boarding schools for deaf and mute children located in the Bukhara region. All registered students from these schools were examined, resulting in a total sample size of 124 children, including 78 boys and 46 girls. To assess the feasibility and applicability of the questionnaire and clinical examination methods, a pilot study was conducted on 30 children. Permission to conduct the study was obtained from the parents of the children involved. The research protocol was approved by the Ethics Committee of the Republic of Uzbekistan and the Supervisory Board of the Bukhara State Medical Institute. Informed consent was obtained from the principals of the respective schools in either the national or Russian language prior to the clinical examinations.
2.1. Questionnaire
- Data on demographics, dietary habits, sugar exposure, oral hygiene knowledge, attitudes, and practices were collected using a specially designed structured questionnaire. All questions were explained to the children in their native language, and responses were recorded directly by the examiner.
2.2. Clinical Examination
- Oral health status and treatment needs were assessed according to the WHO Oral Health Assessment Form (1997) [14]. The children were examined while seated upright in sufficient natural daylight using Type III examination. The examination was conducted with the help of a dental mirror and a Community Periodontal Index (CPI) probe. Instruments were sterilized in an autoclave before examining each child.
2.3. Statistical Analysis
- Data analysis was performed using SPSS v16.0 software. Cohen's kappa coefficient was used to assess examiner reliability. Descriptive statistics, including mean, standard deviation, and percentages, were calculated. Associations were evaluated using the chi-square test, with P-values < 0.05 considered statistically significant.
3. Results
- Table 1 presents the sociodemographic characteristics of the study participants. The study involved 124 schoolchildren with hearing and speech impairments aged 6 to 18 years, with a mean age of 12.95 years. The majority of participants, 55 (44.4%), belonged to the 12–14-year age group.
|
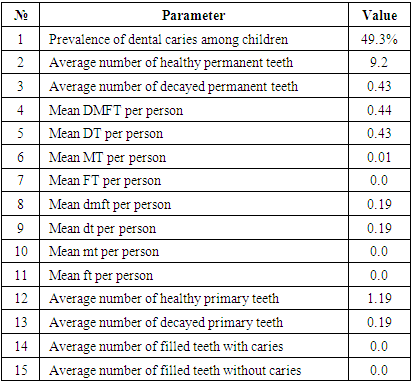
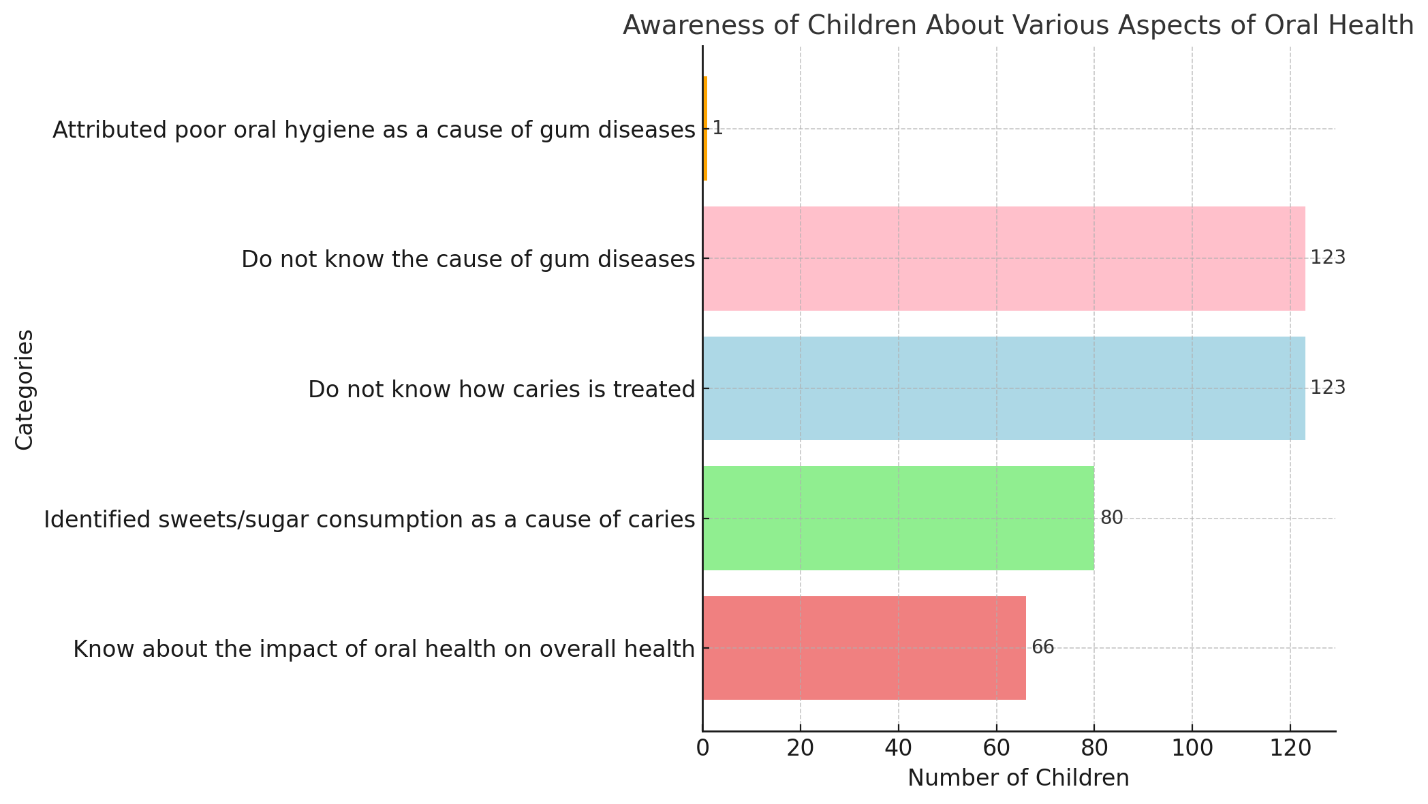 | Figure 1. Knowledge and attitudes towatd oral healt among deaf and mute children |
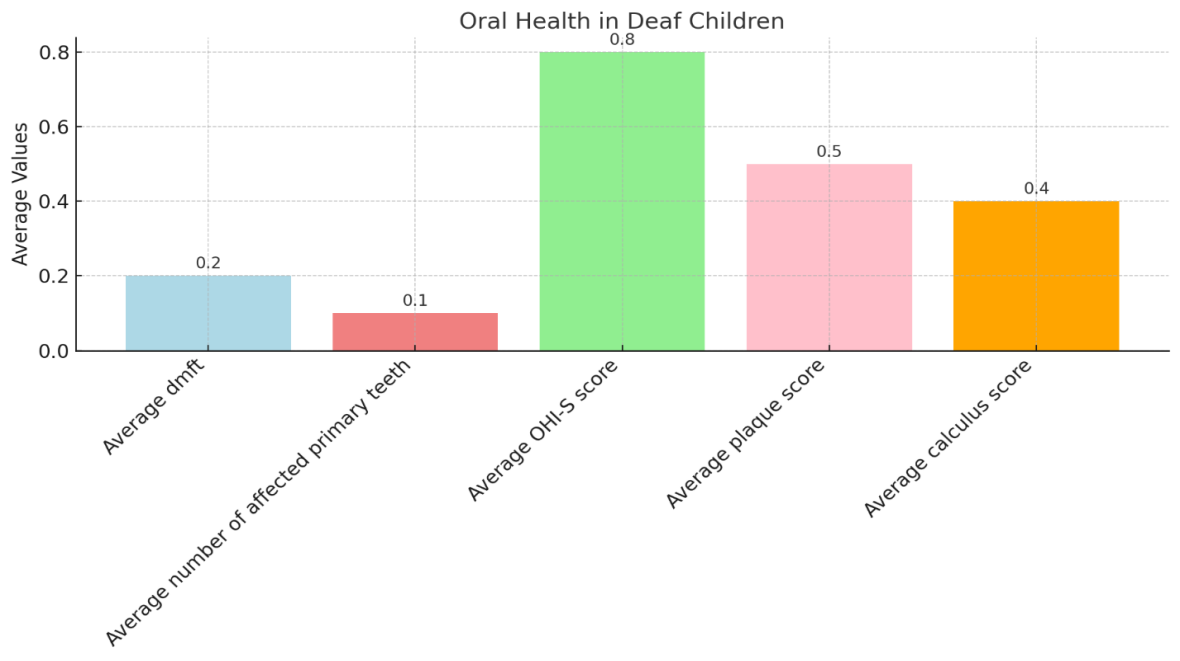 | Figure 2. Interpretation of Dental Caries and Oral Hygiene Status |
|
4. Discussion
- Oral health is a crucial component of overall health and well-being. Individuals with special needs have the same rights to good oral health as other citizens. Unfortunately, due to their condition and lack of awareness, oral diseases in such children often go undiagnosed, leading to a high unmet need for dental care. This study aimed to assess the oral health status and treatment needs of deaf and mute children in the Bukhara region.Maintaining good oral hygiene practices from early childhood is key to ensuring oral health. In this study, 85.7% of deaf-mute children used a toothbrush, while 14.3% cleaned their teeth with their fingers. These results align with a study in Russia where 85.3% used a toothbrush, and 14.67% used fingers. In contrast, a study in India found that 97.37% of children used a toothbrush, likely due to greater awareness in developed communities.Dental fluorosis was observed in 5% of participants, consistent with a study in Kuwait, which reported 10% prevalence. Calculus was found in 78.5% of children, similar to the 91.7% observed in an Indian study.On average, participants had 1.75 sextants with healthy periodontal status, which was lower than the 3.02 ± 2.39 reported in Udaipur, but the number of sextants with calculus was higher — 3.59 compared to 0.51 ± 0.98 in Udaipur. This highlights a higher prevalence of periodontal disease among children with hearing and speech impairments (87.4%) compared to 67% in Udaipur.Children with special needs can learn and practice oral hygiene as effectively as other children, provided their caregivers and teachers are educated about their unique needs. The findings emphasize the importance of adapting approaches to suit the individual needs of these patients.In this study, 36.3% of children required superficial fillings, 4.2% needed crowns, 2% required pulp therapy, and only 1% needed tooth extraction. These results highlight the need for greater awareness, better access to dental care, and preventive programs.This study underscores the significant unmet dental needs among children with hearing and speech impairments, necessitating further research and the development of targeted educational and preventive strategies.
5. Conclusions
- Children with hearing and speech impairments show higher caries prevalence, poorer periodontal health, and greater unmet dental care needs compared to healthy children.• Efforts must be made to improve access to dental services and educate parents and caregivers about oral health care.• Future initiatives should focus on educational programs, preventive interventions, and enhancing the quality of dental care for children with special needs.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML