-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1369-1372
doi:10.5923/j.ajmms.20251505.11
Received: Apr. 9, 2025; Accepted: Apr. 28, 2025; Published: May 8, 2025

Results of Histological Examination of the Cyst Membrane in Patients with Maxillary Sinus Cysts
Jamolbek Djuraev , Sunnatilla Mirzaev , Ilyosjon Soatov
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

To determine the specific features of the histological structure of retention cysts in the maxillary sinus in patients with various associated diseases of the nasal cavity and paranasal sinuses, we analyzed the results of histological examinations using the general sampling method. Morphological examination was conducted on all operated patients in the groups, with a total of 140 histological studies performed. Bilateral removal of maxillary sinus retention cysts was carried out in 27 patients. In the medical history of patients, allergic rhinitis was observed in 38 cases, nasal aerodynamic disorders in 95 cases, and recurrent bacterial sinusitis in 42 cases.
Keywords: Maxillary sinus, Cyst, Endoscopy, Allergic rhinitis, Morphological examination, Retention cyst
Cite this paper: Jamolbek Djuraev , Sunnatilla Mirzaev , Ilyosjon Soatov , Results of Histological Examination of the Cyst Membrane in Patients with Maxillary Sinus Cysts, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1369-1372. doi: 10.5923/j.ajmms.20251505.11.
1. Introduction
- Currently, in surgical practice for chronic maxillary sinusitis, failure to consider the patient's anatomical features can be viewed as a lack of understanding regarding the significance of nasal cavity structural anomalies in the development of maxillary sinus pathological conditions. Anatomical anomalies can complicate access to the maxillary sinus and may contribute to and sustain the exacerbation of the chronic process [1,4]. Therefore, when an anatomically significant pathology is detected in the area of the nasal septum and nasal turbinates, it is recommended to perform additional surgical procedures, ranging from septoplasty to submucosal resection, to correct the altered anatomical structures. This allows for improved visibility of the surgical field and ensures better mobilization.Various modifications of trocars have been developed for performing microhaimorotomy through the anterior wall of the maxillary sinus, allowing its complete restoration as a result of trepanation of the anterior wall of the maxillary sinus and subsequent reparative regeneration of bone tissue [5]. Experimental studies conducted on cadaveric material showed a high damaging effect of any trocar on the anterior wall of the maxillary sinus. This can subsequently lead to the development of postoperative conditions, such as “operated maxillary sinus” syndrome or “post-Caldwell-Luc” syndrome [4]. In cases of chronic rhinitis, operations are performed on the lower nasal turbinates: submucosal vasotomy, conchotomy, lateralization, turbinoplasty, and others.
2. Materials and Methods
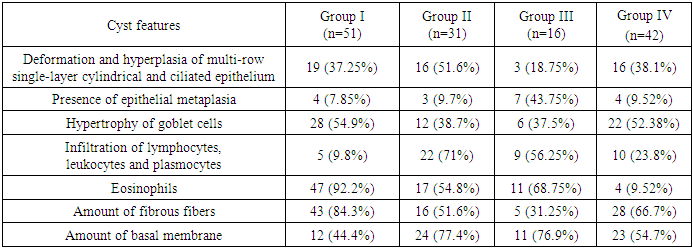
- In cases of chronic rhinitis, operations are performed on the lower nasal turbinates: submucosal vasotomy, conchotomy, lateralization, turbinoplasty, and others [5]. During the surgical procedure, the removal of maxillary sinus cysts was carried out using the following methods, and the patients were divided into 4 groups:1) endonasal endoscopic haimorotomy through the natural ostium of the maxillary sinus in 51 patients;2) endonasal endoscopic haimorotomy through the inferior nasal meatus in 31 patients;3) microhaimorotomy through the anterior wall of the maxillary sinus in 16 patients;4) endonasal endoscopic maxillary sinusotomy through the crista conchalis in 42 patients. The results of the histological examination are presented in Table 1.
|
3. Result
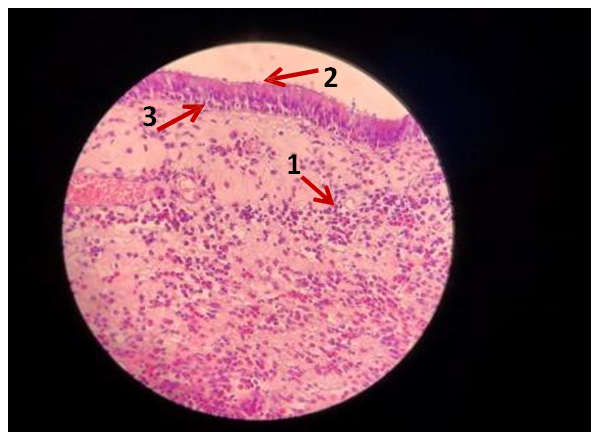
- The first type of morphological changes in the maxillary sinus cyst membrane was observed in patients with allergic rhinitis, and the following results were analyzed: deformation and hyperplasia of the multilayered single-layer cylindrical and ciliated epithelium in 19 (37.25%), hypertrophy of goblet cells in 28 (54.9%), fibrosis of the submucosal layer in 43 (84.3%), pronounced eosinophilic infiltration in 47 (92.2%), and hyperplasia of the respiratory epithelium in 12 (44.4%) [8]. (Figure 1).
4. Discussion
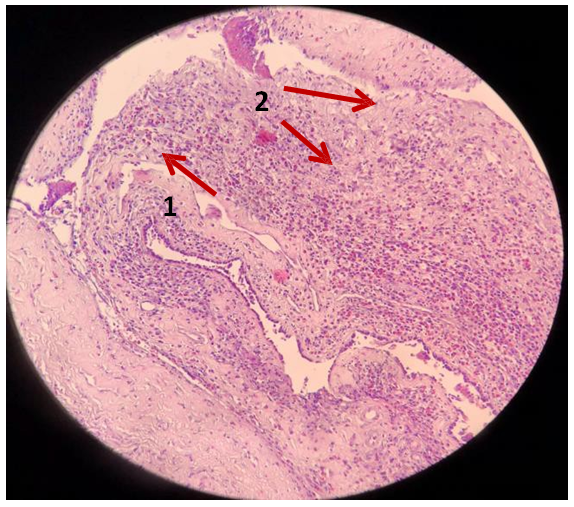
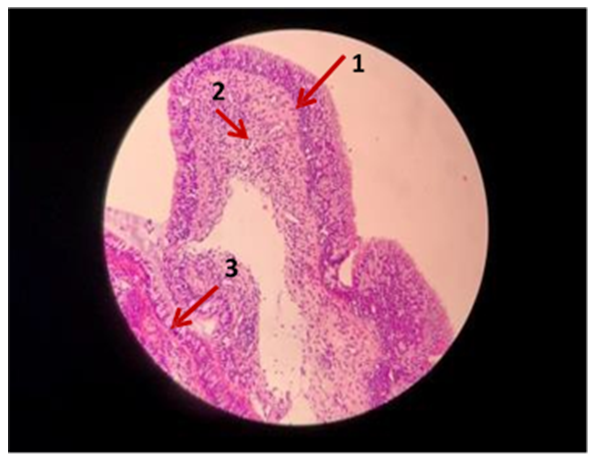
- The histological examination of maxillary sinus cyst membranes presented in this study provides critical insights into the pathomorphological distinctions associated with various comorbid nasal and paranasal conditions. Our analysis identified three primary histological patterns of retention cysts, each correlated with a specific underlying pathology: allergic rhinitis, nasal aerodynamic disorders, and recurrent bacterial sinusitis.In patients with allergic rhinitis, the predominant histological features included extensive eosinophilic infiltration (92.2%), hypertrophy of goblet cells (54.9%), and hyperplasia of the respiratory epithelium (44.4%). These findings are consistent with earlier observations that associate eosinophilia and epithelial remodeling with allergic inflammation in sinonasal mucosa [6,8]. The elevated presence of goblet cell hyperplasia suggests increased mucus production, a hallmark of allergic rhinitis, which may contribute to cyst development and persistence. This subgroup demonstrates that allergic mechanisms lead to distinct tissue remodeling, supporting the role of immune-mediated epithelial damage in sinus cyst pathogenesis.Patients with nasal aerodynamic disorders exhibited a different histological profile. Pronounced fibrosis (51.6%) and leukocytic infiltration (71%) were the dominant features. These changes likely reflect chronic mechanical irritation and localized mucosal hypoxia due to altered airflow, leading to persistent submucosal inflammation and fibrosis. Similar histopathological findings have been reported in studies examining the effects of septal deviation and turbinate hypertrophy on maxillary sinus ventilation and drainage [5,7]. The high rate of basement membrane thickening (77.4%) also aligns with these chronic structural disturbances and suggests ongoing reparative processes.In contrast, the histological structure in patients with recurrent bacterial sinusitis showed a predominance of basement membrane thickening (76.9%) and moderate leukocyte infiltration (56.25%). The combination of these features is indicative of repeated inflammatory episodes and mucosal regeneration attempts. Fibrosis was less frequent (31.25%) in this group, potentially reflecting shorter or less consistent disease duration compared to chronic aerodynamic disorders. Prior research supports the association between basement membrane remodeling and chronic infection-driven inflammation in sinus pathology [2,3].Interestingly, Group III (patients undergoing microhaimorotomy through the anterior wall) exhibited the highest frequency of epithelial metaplasia (43.75%), which may point to greater surgical trauma or preexisting chronic epithelial stress. This observation warrants further investigation into the long-term effects of anterior wall access techniques on mucosal integrity and regenerative capacity.Overall, the study’s findings underscore the heterogeneity of histological presentations in maxillary sinus cysts and highlight the importance of correlating tissue pathology with the underlying etiology. Understanding these morphological distinctions is crucial for tailoring surgical approaches and predicting postoperative outcomes. For instance, in allergic patients, interventions might benefit from adjunctive anti-inflammatory therapies, while structural correction may be prioritized in patients with nasal airflow disturbances.Further studies with larger sample sizes and molecular profiling are recommended to validate these associations and to explore the role of specific cytokines and growth factors in the fibrotic and inflammatory processes observed.
5. Conclusions
- Thus, analysis of the histological structure of the maxillary sinus cyst membrane allowed us to distinguish four types of tissue histology in groups of patients with three different diseases, each characteristic of a particular pathology [2,3]. The first type of morphological structure of the maxillary sinus cyst membrane is characteristic of allergic rhinitis and is marked by: the presence of eosinophilic infiltration, hyperplasia of the respiratory epithelium, and hypertrophy of goblet cells. The second type of morphological structure of the maxillary sinus cyst membrane was most common in patients with nasal cavity aerodynamic disorders. The distinctive features of this cyst wall structure were: pronounced fibrosis, leukocyte infiltrate, and thickening of the basement membrane [6,8]. The third type of morphological structure of the maxillary sinus cyst is characteristic of patients with recurrent bacterial sinusitis, and the histological picture is characterized by: the presence of leukocytic, lymphocytic, and plasmacytic infiltration, as well as pronounced fibrosis and thickening of the basement membrane.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML