-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(5): 1348-1353
doi:10.5923/j.ajmms.20251505.07
Received: Apr. 3, 2025; Accepted: Apr. 28, 2025; Published: May 8, 2025

Approval of the Method of Treatment of Spontaneous Bacterial Asicite Peritonitis with Etiology of Liver Cirrhosis
Komilov Jahongir 1, Urokov Shuhrat 2, Khamroyev Khudoyshukur 3
1Bukhara Branch of the Republican Scientific Center of Emergency Medical Care, Bukhara City, Uzbekistan
2Bukhara State Medical Institute Named After Abu Ali Ibn Sino, Department of Surgery Diseases, Bukhara City, Uzbekistan
3Asian International University, Bukhara City, Uzbekistan
Correspondence to: Komilov Jahongir , Bukhara Branch of the Republican Scientific Center of Emergency Medical Care, Bukhara City, Uzbekistan.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Spontaneous bacterial ascites peritonitis (SBAP) is one of the most serious complications of liver cirrhosis, requiring urgent intervention. This article reviews current treatment options for SBAP with an emphasis on the etiology of liver cirrhosis. The focus is on the etiology of the disease, diagnostic approaches, and key principles of medical and surgical therapy. The role of preventing recurrence of SBAP in patients with liver cirrhosis is also discussed. Materials and methods: Data on the examination and treatment of 126 patients with spontaneous bacterial ascites peritonitis of liver cirrhosis etiology, who were treated during 2020-2024 in the surgical department of the Bukhara branch of the Bukhara State Medical Institute, Department of Surgical Diseases, Clinical Base, Bukhara branch of the Republican Scientific Center for Emergency Medical Care, were analyzed. All patients were divided into 2 groups according to the treatment method: I-comparison group (n=68) included patients with spontaneous bacterial ascites peritonitis of liver cirrhosis etiology, whose results of traditional treatment were retrospectively analyzed. In the II main group (n=58) in the treatment of patients with complications of spontaneous bacterial ascites peritonitis due to liver cirrhosis, in addition to the active conservative method, the effect of the Ulinastatin drug and puncture methods were used comprehensively. Conclusion: The prognosis for patients with SBAP depends on many factors, including the degree of cirrhotic transformation of the liver, the speed of treatment initiation, age, and comorbidities. It is important to remember that if treatment is not timely or adequately provided, SBAP can lead to sepsis, multiple organ failure, and death. Modern approaches to the treatment of SBAP include early diagnosis, empirical antibacterial therapy, supportive care, and relapse prevention. However, despite advances in medicine, the task of improving treatment outcomes through personalized approaches and prevention of complications remains relevant.
Keywords: Spontaneous bacterial ascites peritonitis, Liver cirrhosis, Treatment, Antibacterial therapy, Relapse prevention, Diagnostics
Cite this paper: Komilov Jahongir , Urokov Shuhrat , Khamroyev Khudoyshukur , Approval of the Method of Treatment of Spontaneous Bacterial Asicite Peritonitis with Etiology of Liver Cirrhosis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1348-1353. doi: 10.5923/j.ajmms.20251505.07.
Article Outline
1. Introduction
- Nowadays, worldwide, spontaneous bacterial ascites peritonitis (SBAP) is one of the complications of liver cirrhosis that can be encountered in many cases, but it is difficult to diagnose, and with its high mortality rate, it is one of the urgent problems of modern surgery. At the global level, the lack of correct and accurate diagnostic criteria for this pathology and the fact that a clear course of treatment has not been determined, causes the death rate to increase even more. Spontaneous bacterial ascites peritonitis with liver cirrhosis etiology is the damage of ascitic fluid by microorganisms, and it is a complication observed with the absence of an obvious source of abdominal infection without breaking the anatomical integrity of the abdominal organs and requiring surgical treatment [2,14,20,40].Liver cirrhosis is the main pathogenetic factor of spontaneous bacterial peritonitis, which is the transfer (translocation) of microorganisms from the intestinal cavity to local lymph nodes, lymph and blood flow. In addition, factors such as portal hypertension and increased intra-abdominal pressure, excessive development of microorganisms in the intestinal cavity, increased permeability of the intestinal wall, decreased local immune response, decreased phagocytic activity of the liver's reticulo-endothelial system, and decreased protective function of ascites fluid contribute to bacterial translocation. also causes [17,19,21,22].The phenomenon of bacterial translocation can occur in healthy people without causing clinically significant consequences, but with the development of JTs, bacterial translocation increases significantly and is an important link in the pathogenesis of liver cirrhosis itself and its complications [8,10,15,32,39]. When physiological bacterial translocation is observed in people without problems with the immune system, it is eliminated by local immune systems [30,40]. This phenomenon makes it possible to stimulate the immune system in healthy people [27,29].In patients with cirrhosis of the liver, the phenomenon of bacterial translocation increases the risk of rapid development of microorganisms in the body and leads to an increase in the systemic inflammatory response, which in turn leads to aggravation of portal hypertension with increased hemostasis and microcirculation disorders [1,12,15,31].Overgrowth of bacteria in the intestinal cavity of patients with liver cirrhosis leads to a decrease in intestinal motility, hypochlorhydria when using proton pump inhibitors (PNIs), impaired secretion of bile acids accelerates these processes [3,23,32].Microorganisms overcome the barrier of the intestinal wall and encounter resident macrophages, which represent the first line of defense of the abdominal cavity. If macrophages fail to destroy colonizing bacteria, the complement system is activated and cytokines are released [4,29,35].The involved neutrophils recognize and destroy these microorganisms. But in the conditions of liver failure and the development of the cirrhotic process, due to the failure of the reticuloendothelial system, neutrophil dysfunction is observed, which cannot stop the colonization of bacteria and leads to the development of infection.The absence of clinical symptoms in patients does not exclude infection in ascitic fluid (AS). The diagnosis of SBP is based on counting the number of neutrophils in AS. The number of neutrophils in AS with microscopic examination methods is significant. The determination of the culture of microorganisms not only confirms the diagnosis, but also makes it possible to use antibiotics rationally [20,23]. Empirical appointment of antibacterial drugs, after clarification of the microorganism culture, use of narrow-spectrum antibiotics gives a clear result in the treatment of this pathology. Even a single dose of broad-spectrum effective antibiotics can reduce AS cultures by 86% after 6 hours. In these cases, it is very important to determine the characteristics of resistance of microorganisms [29,37].Diagnosis of SBAP patients based only on objective clinical data, without bacteriological examinations of AS, is not considered sufficient in patients with JTs and ascites [23]. Of course, it is advisable to conduct a paracentesis in patients and make a diagnosis by identifying neutrophils and microorganisms in AS. However, some clinicians do not perform paracentesis in patients with coagulation disorders because of the risk of bleeding. Scientists emphasize the importance of an individual approach to paracentesis in patients with JTs [21,27]. Paracentesis is mandatory for all patients with primary ascites, as well as for patients with persistent ascites or hospitalization for any complications of JTs [25,41].
2. Purpose of the Research
- For the purpose of paracentesis, a puncture of the abdominal wall is performed 2 cm below the navel, on the right or left costal edge of the mid-corinal line, 2-4 cm above the anterior upper costal transition and medially. If possible, paracentesis should be performed under the control of ultrasound examination, as this method helps to find the safest area for puncture, it is necessary that a sufficient amount of ascites fluid is collected in this area and there are no intestinal rolls or parenchymatous organs. This is especially important for patients who are overweight or have scars on the anterior abdominal wall after multiple surgeries [18,19,29].The accuracy of calculating the total number of leukocytes and the number of neutrophils in the ascitic fluid is entirely related to the high level of expertise of the specialist conducting the research. In addition, the implementation of cell counting and differentiation in ascitic fluid requires very responsible and strict control [28,33]. In carrying out this research, special conditions should be created for the doctor.
3. Materials and Methods
- Data on the examination and treatment of 126 patients with spontaneous bacterial ascites peritonitis of liver cirrhosis etiology, who were treated during 2020-2024 in the surgical department of the Bukhara branch of the Bukhara State Medical Institute, Department of Surgical Diseases, Clinical Base, Bukhara branch of the Republican Scientific Center for Emergency Medical Care, were analyzed.All patients were divided into 2 groups according to the treatment method:I-comparison group (n=68) included patients with spontaneous bacterial ascites peritonitis of liver cirrhosis etiology, whose results of traditional treatment were retrospectively analyzed.In the II main group (n=58) in the treatment of patients with complications of spontaneous bacterial ascites peritonitis due to liver cirrhosis, in addition to the active conservative method, the effect of the Ulinastatin drug and puncture methods were used comprehensively.It should be noted that this main group includes patients treated in 2023-2024. In addition, in order to maintain the synchronicity of the patient groups involved in our study, patients with the following additional conditions were excluded: severe liver failure, hepatic encephaloptysis grade III, ascites resistant type, extrahepatic PG, older than 70 years, platelets below 50 x10^9, if the spleen size of patients is below 160 cm2, additional cardiovascular diseases, patients with diabetes mellitus, cases with oncological and serious serious diseases were not included.
4. Results and Discussion
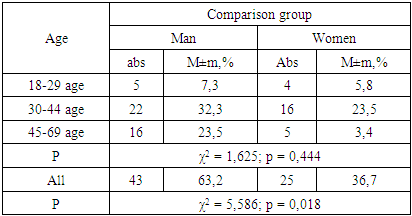
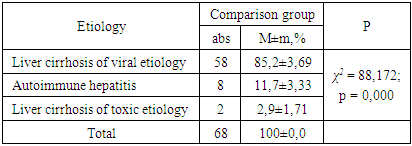
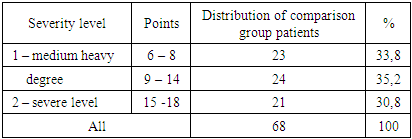
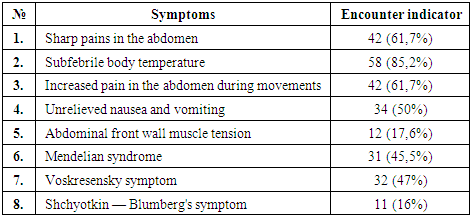
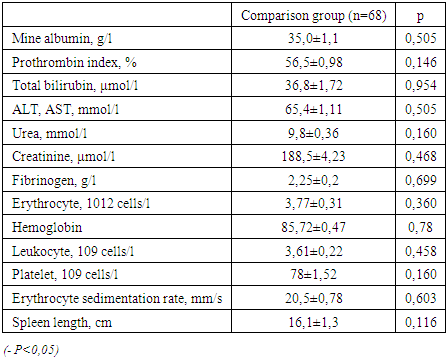
- The comparison group of our study included 566 patients with ascites peritonitis of liver cirrhosis etiology who were treated in the Bukhara branch of the Bukhara State Medical Institute during 2020-2022 and who underwent complex treatment using traditional methods. As a result of retrospective analysis, it was shown that 68 of these 566 patients received treatment for spontaneous bacterial ascites peritonitis on the background of liver cirrhosis.Therefore, the results of a retrospective analysis of the examination and treatment data of 68 patients with spontaneous bacterial ascites peritonitis of liver cirrhosis etiology were included in this comparison group. The average age of the patients was 44.3±1.1 years. Among the patients, there was a predominance of males - 22 people. In all cases, PG had the character of intrahepatic block, i.e., JC, the cause of which was viral infection in 91.3% of cases and alcoholic and autoimmune liver cirrhosis in 8.7%. The comparison group of patients was analyzed according to gender in the following order: men - 43 (63.2%), women - 25 (36.7%) patients (Table 1).
|
|
|
|
|
|
5. Conclusions
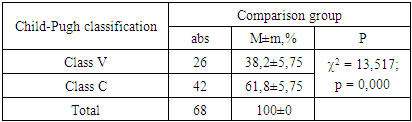
- Bacterial overgrowth in the small intestine against the background of liver cirrhosis, bacterial translocation, spontaneous bacterial peritonitis, development of systemic inflammation in the body leads to polyorgan failure, Child-Pugh class V and C mortality rate is 24% (r=0.002).In the comprehensive treatment of spontaneous bacterial ascites peritonitis caused by liver cirrhosis, the use of the drug ulinostatin reduces the systemic inflammatory reaction in the body, stabilizes changes in the immune system, increases the ability to regenerate liver cells, and at the same time eliminates liver failure.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML