Ochilova Donokhon 1, Kasimova Nodirabegim 2
1DSc, Associate professor in the 2nd Pediatrics, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
2Master in the 2nd Pediatrics, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan
Correspondence to: Kasimova Nodirabegim , Master in the 2nd Pediatrics, Bukhara State Medical Institute named after Abu Ali ibn Sino, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Congenital heart defects (CHD) are a group of diseases characterized by abnormalities in the structure of the heart that occur during fetal development. Surgical correction of CHD has significantly improved the prognosis for children with such diseases, but continued follow-up remains an equally important element of treatment. The purpose of this review is to consider the current literature on the importance of follow-up of children after surgical correction of CHD. The paper discusses the main problems associated with patient follow-up, as well as its impact on quality of life and long-term treatment outcomes. Various diagnostic and monitoring methods are considered, as well as the role of multidisciplinary teams in managing the condition of children with CHD after surgery. The conclusion emphasizes the need for ongoing monitoring for early detection of possible complications and improved treatment effectiveness.
Keywords:
Congenital heart defects, Surgical correction, Dispensary observation, Children, Long-term results, Monitoring, Complications
Cite this paper: Ochilova Donokhon , Kasimova Nodirabegim , Congenital Heart Defects: Importance of Improving Follow-up of Children After Surgical Correction (Literature Review), American Journal of Medicine and Medical Sciences, Vol. 15 No. 5, 2025, pp. 1315-1324. doi: 10.5923/j.ajmms.20251505.01.
1. Introduction
Congenital heart defects (CHD) are one of the most common forms of malformations (22% of all congenital malformations). Among malformations of internal organs, CHD rank second (after anomalies of the central nervous system). Of the total number of patients with CHD in the population, about 60% are children under 14 years of age. The proportion of all CHD (taking into account cases of intrauterine fetal death and early miscarriages) among malformations reaches 40%. CHD are often detected when the fetus dies in the early stages of gestation, while cases of fetal death in the final stages of pregnancy are more often caused by chromosomal pathology and severe developmental anomalies [7].The incidence of congenital heart disease (CHD) has remained high in recent years and it has become the most common congenital defect, becoming the leading cause of death and disability in infants and young children [1].Among all congenital malformations (CM) in children, CHD occupy the first place in terms of frequency of occurrence, accounting for 31.5% [15]. The most common cause of disability in children with CM are defects of the musculoskeletal system (27.2%) and congenital heart defects (20%), which make up almost half of the total number of congenital malformations that limit life activities [11].Any pathologies of the heart and main vessels are formed during the period of embryogenesis, that is, in the first 2 months of fetal development. CHDs can appear due to aggravated heredity, chromosome mutations, or due to the impact of teratogenic factors on the fetus. Despite the fact that the exact causes of intrauterine developmental disorders are not yet known, researchers suggest that the following external and internal factors can provoke heart defects: previous infections, among which rubella, flu, chickenpox, measles, herpes, cytomegalovirus, syphilis, mumps are especially dangerous; early toxicosis of pregnancy; receiving a dose of radiation, X-rays, undergoing a course of radiation therapy; acute vitamin deficiency of the mother; taking certain medications harmful to the fetus or drug overdose; smoking, drug addiction, alcoholism; the presence of severe chronic diseases in the mother and her age over 40 years; often a child with TMS has an underlying genetic disease, and most often it is Down syndrome [5].
2. Materials and Methods
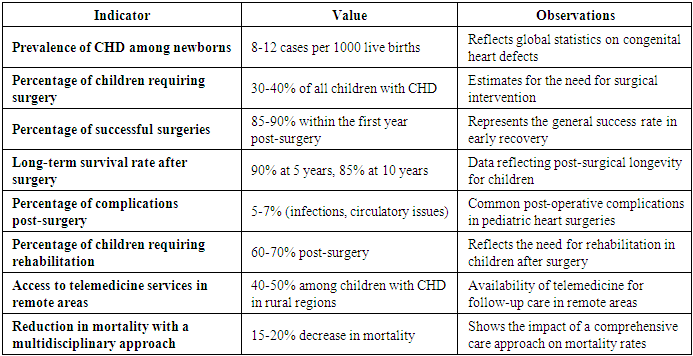
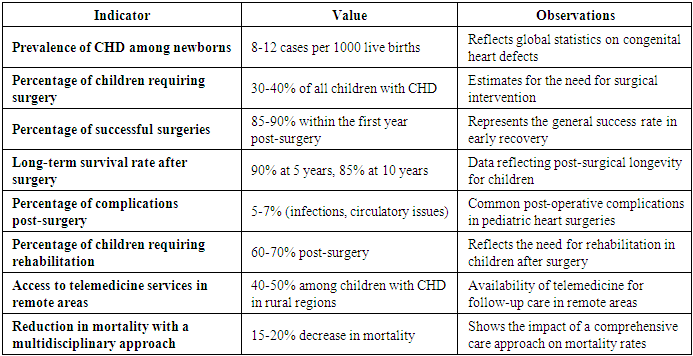
Цe performed a literature search with Google Scholar, PubMed and Web of Knowledge, using combinations of the following key words: “congenital heart defects”, “rehabilitation”, “postooperative condition”, “follow-up”, “quality of life” and “children”. This screening led to the selection 18 articles of the last 20 years. Articles were selected according to the following criteria: 1. Publication time - last 20 years.2. Emphasis was placed on the selection of articles that provide comprehensive useful information about the statistical data of congenital heart defects, especially postoperative conditions.3. Articles highlighting the weaknesses of postoperative management of patients and offering alternative methods for solving these shortcomings were also highlighted.Without surgical treatment, congenital heart defects are more likely to result in death in children in the first year of life than other congenital malformations. According to various authors, the prevalence of congenital heart defects ranges from 8 to 12 cases per 1000 newborns (Table 1). Due to the development of cardiac surgery in recent decades, the survival rate of patients with congenital heart defects has improved. At the same time, children after surgical treatment of congenital heart defects have a lower quality of life compared to their healthy peers, which may be associated with both the underlying and concomitant diseases, as well as psychological factors, overprotection by parents, and insufficient physical activity [11].Table 1. Statistical Data on Congenital Heart Disease in Children and Surgical Outcomes
 |
| |
|
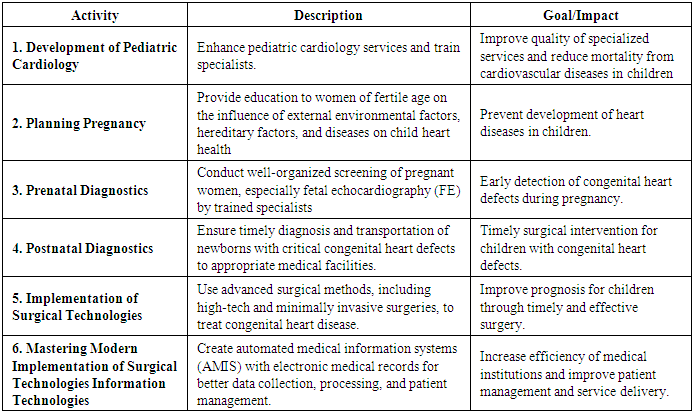
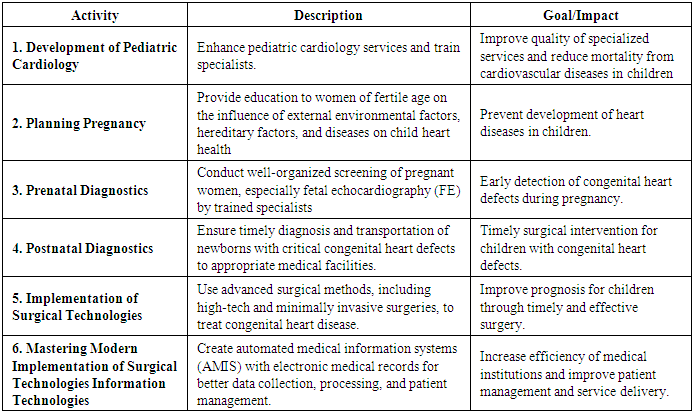
One of the most common congenital defects is the ventricular septal defect (VSD). This defect is characterized by severe heart failure and the development of pulmonary hypertension, which determines the need for early surgical correction. Cardiac surgery can improve the functional state of the child's body. However, even after surgery, such children show morphofunctional changes in the cardiovascular system, physical and neuropsychic development disorders, and decreased resistance [13].Experience of economically developed countries shows that the main condition for growth life expectancy population is a reduction in mortality from cardiovascular diseases. When reduction in the number of children prevalence of cardiovascular diseases in children in recent years increased more than 2 times [2].CHD: their early diagnosis, treatment, and management tactics are one of the main areas of work of the regional children's cardiorheumatology center [5].Advances in cardiovascular surgery now make it possible to correct all congenital heart defects, even the most complex ones. Pediatric cardiologists, neonatologists, pediatricians, and functional diagnostics doctors use all the possibilities for timely and early diagnosis of congenital heart defects [7].Prevention, diagnosis and treatment of cardiovascular diseases in childhood have of paramount importance for improvement health and life expectancy life [2].The vision of the global community is that every child born anywhere in the world with a congenital heart defect should have access to appropriate medical and surgical care. People with large atrial septal defects have a mortality risk of 5–15% until reaching the age of 30 [3].Thanks to the improvement of technology for the diagnosis and treatment of congenital heart disease, as well as the success of cardiac surgeries, surgical and interventional treatment can allow at least 85% of children with congenital heart disease to survive to adulthood [1].While in developed countries the focus has shifted from efforts to reduce postoperative mortality to improving quality of life and reducing morbidity, the rest The world still needs to ensure basic access to congenital heart care [3].Thanks to the development of cardiac surgery, the mortality rate of patients with CHD has decreased, including infant mortality; approximately 90% of children with complex forms of CHD survive to adulthood. After surgical treatment, patients with CHD require dynamic monitoring by a cardiologist and rehabilitation measures [12].The study of remote results of surgical treatment of congenital heart disease in children is a pressing issue of our time. There are still no unified criteria for assessing remote results of surgical correction of congenital heart disease in children that could be used by pediatricians and cardiologists in regions remote from cardiac surgery clinics. The issue of postoperative monitoring of this group of patients also remains relevant. To date, there is no system of postoperative restorative treatment for younger children and rehabilitation of older children [17].Of course, a successfully performed operation is of decisive importance in the fate of a patient with congenital heart disease. At the same time, following surgical treatment of patients with this pathology, the next stage begins, which includes a set of rehabilitation measures.Considering that with an optimally organized rehabilitation environment, children with congenital heart disease after a successful operation in most cases can become full-fledged individuals of our country. The main efforts in the postoperative period must be directed specifically at rehabilitation measures for such patients [15].Quality of life assessment is a comprehensive assessment of human health in three aspects: physical, mental and social activity, and is becoming an important indicator for assessing the physical and mental health of children. It reflects children's cognition and satisfaction with their current living conditions.A systematic review and meta-analysis showed that health-related quality of life was worse in postoperative CHD patients compared to healthy controls in all domains. Therefore, it is important to pay attention to the postoperative quality of life of children with CHD to understand their health status and improve their quality of life [1].Comprehensive restorative treatment helps to minimize the consequences of congenital heart disease and the impact of intraoperative aggressive factors (artificial blood circulation and ventilation, anesthesia), as well as prevent developmental disorders in children and reduce the risk of disability [6].The sanatorium stage is of great importance in rehabilitation, since it allows for a comprehensive approach to treatment, taking into account the biopsycho-physiological parameters of children’s health [7].Determination of rehabilitation potential and its dynamics play a significant role in assessing the effectiveness of the treatment. The rehabilitation potential of children with congenital heart disease is determined based on the results of a set of studies, including determination of the state of the cardiovascular system, morphological parameters, functional reserves of the body by conducting tests for dosed physical activity, and the psycho-emotional state of the child. A standardized approach to assessing the effectiveness of rehabilitation treatment at this stage in children after radical correction of congenital heart disease has not been developed [13].Children with CHD have poor blood transport and weaker gastrointestinal function due to heart failure, which leads to impaired nutrient intake. At the same time, energy intake in these children is higher than that of normal children of the same age, which leads to inadequate nutrient supply and growth retardation. The postoperative activities of children are limited, and postoperative wounds also affect the aesthetics, which may affect the future life and education of children. It also affects their quality of life to a certain extent. Studies have shown that the overall postoperative quality of life of children with CHD is lower than that of children without CHD of the same age. Therefore, it is worth paying special attention to the quality of life of this group of children [1].Pediatric cardiology care involves an individual approach to each patient. At the end of the inpatient part of the rehabilitation program, the decisive factor is the family's readiness for the child's rehabilitation activities at the outpatient stage. Publications by domestic and foreign researchers quite widely reflect the issues of the positive impact of rehabilitation of patients with congenital heart disease on tolerance to physical activity, performance and quality of life [11].The health of children in the remote period after surgical treatment of septal congenital heart disease at an early age is characterized by asthenovegetative and psychoemotional disorders, as well as functional disorders of the respiratory system and vegetative status. The reactions of the cardiovascular system to physical activity in children in the remote period after surgical treatment of septal congenital heart disease at an early age are characterized by unfavorable types in most children [13].However, to date, rehabilitation programs for children with congenital heart disease remain underutilized, and clinical research in this promising area is limited; questions also remain about the optimal structure of such programs and the participation of parents of children with congenital heart disease in them [11].More than 90% of the 1 million children born with congenital heart disease worldwide receive inadequate or no care. It is time to promote the treatment of patients with congenital heart disease and to reach out to those living in the developing world [4].Thanks to the continuous development of science, technology and medicine, more and more children with congenital heart disease survive after surgery. At present, we have a general idea of the current situation with the quality of life of postoperative children with congenital heart disease, but the lack of long-term follow-up makes the research results insufficiently deep and comprehensive. Therefore, it is necessary to conduct long-term observation of children and examine the current situation of children's life at different times after surgery in order to reliably reflect the quality of life and the process of its change after surgery [1].A number of researchers note that as a result of the rehabilitation program, patients experience improved tolerance to physical activity, an increase in the peak value of oxygen consumption during exercise, an increase in the power of the work performed, an improvement in growth parameters and body weight, and an improvement in metabolic processes in the myocardium. Of particular importance is the development of methods for assessing the rehabilitation potential and monitoring the effectiveness of rehabilitation of infants after radical correction of congenital heart disease [13].The rehabilitation environment surrounding a child after surgical correction of congenital heart disease combines the following levels: a cardiac surgery hospital, a specialized rehabilitation center, and the family. The latter plays a decisive role in strictly following the recommendations of medical specialists [15].Late diagnosis (32.7%) and, accordingly, late correction of congenital heart disease (19.8%) have a great impact on the unsatisfactory results of surgical treatment of congenital heart disease in children. The remoteness of regions from cardiac surgery centers is one of the serious reasons for late, surgical < treatment of congenital heart disease, the occurrence of postoperative complications. This dictates the need to develop regional cardiac surgery centers, improve specialized cardiac care for children with congenital heart disease [17].The prognosis is better in children with a family income that can afford good treatment conditions, provide good nutritional conditions and a comfortable and safe living environment. Access to quality social health services is also an important factor in improving the quality of life of children after surgery [1].Thus, based on the results of a systematic review of the MEDLINE/PubMed, EMBASE, Cardiosource Clinical Trials Database, and Cochrane Library information databases, Tikkanen AU et al. identified only 18 studies (2 of which were case reports) containing an analysis of the results of structured rehabilitation programs with elements of physical exercise for patients with CHD under 18 years of age. The authors emphasize that the optimal structure of pediatric cardiac rehabilitation programs remains unclear and are inclined to believe that, in addition to a combination of aerobic and strength exercises, programs should probably include additional treatment methods, breathing exercises, educational training, and psychological support. In addition, the studies reviewed did not take into account concomitant diseases, and also missed such an important aspect as the role of parents, which deserves more attention. As a result of their scientific review, Tikkanen AU et al. concluded that the underutilization of rehabilitation programs for children with CHD is due to limited technical and human resources, economic issues such as lack of insurance coverage for programs, underestimation of the importance of rehabilitation programs and lack of awareness of them by health care providers, and patient-related factors such as logistical issues, family costs, and parental anxiety [11]. The authors believe that addressing these issues will require changes at various levels of health care policy, protocols, and improved understanding of the importance of these programs among health care professionals and families of patients with CHD [11].Of course, one cannot but agree that “the collective work of the staff is of decisive importance in carrying out rehabilitation measures”, and the scientific basis of rehabilitation care is no less important [11].Children who have received correction for TMA correction even in optimal terms and in highly specialized cardiology centers have functional disorders of the cardiovascular system that progress and accumulate over time. These children have limitations in physical activity, sports, professional restrictions, women cannot give birth on their own. Therefore, these children regularly undergo medical and social examination to extend their disability [5].During surgical intervention, anatomical anomalies are eliminated, but cardiovascular dysfunction may persist; to normalize or improve it in the postoperative period, it is necessary to carry out a set of rehabilitation measures. However, at present, this is associated with significant organizational difficulties. Thus, a survey of parents of children with congenital heart disease conducted at the A.N. Bakulev National Center for Cardiovascular Surgery showed that in 28.3% of cases there is no pediatric cardiologist at the place of residence, and in 33.4% of cases, obtaining a cardiologist consultation requires a significant amount of time to make an appointment. Even according to the subjective opinion of parents, about 37.8% of them have information about the optimal level of physical activity for their child. Only 5.3% of children underwent rehabilitation in rehabilitation centers or sanatoriums. The latter is due to the extremely limited number of institutions accepting children with congenital heart defects [14].Children after surgical correction of congenital heart defects require follow-up observation with mandatory assessment of certain Doppler echocardiographic criteria depending on the initial type of hemodynamic disorder [17].Thus, over the past 10 years, there has been a significant increase in the number of operations and endovascular interventions on the heart and blood vessels, and significant advances in all areas of cardiovascular surgery. The solution to the problem of further development and improvement of cardiac surgical care for the population of the country is possible with the active support of the state, with the help of state social programs and voluntary insurance programs for expensive types of treatment [8].The integral components of the organizational and functional model of rehabilitation care for patients with congenital heart defects include the complex interaction of the organizational and structural model of the rehabilitation center for these patients, elements of the model of technical equipment of the rehabilitation center, models of the information structure and information environment [11].The organizational and functional model of rehabilitation care for patients with congenital heart defects includes 3 stages of rehabilitation: 1) in a cardiac surgery hospital after the provision of high-tech, specialized medical care; 2) rehabilitation in a specialized cardiac rehabilitation center, early recovery period; 3) rehabilitation in a specialized cardiac rehabilitation center, late recovery period [11].Modern approaches to patient management after surgical correction of congenital heart disease dictate the need to create and implement a system of medical rehabilitation for children with congenital heart disease in the country, taking into account the territorial proximity of children's rehabilitation centers to cardiac surgery clinics [11].The relevance of creating a modern concept of rehabilitation care for patients with congenital heart disease is emphasized by experts from the American Association of Cardiovascular and Pulmonary Rehabilitation, American Heart Association (AHA), British Cardiovascular Society, European Association for Cardiovascular Prevention and Rehabilitation, National Audit for Cardiac Rehabilitation, and well-known specialists from Russia, Belarus, and Ukraine. The need to develop medical aspects of treatment, physical, psychological, and social rehabilitation of GUCH patients is confirmed by the AHA data on the development of severe cardiac disorders in 25–40% of them in the late postoperative period, which requires a multidisciplinary approach to monitoring the state of health, rehabilitation, or repeated surgical interventions. Given that the socioeconomic effect of rehabilitation programs in such patients is delayed and may manifest itself only years later, when the operated children become adult members of society, the advisability of developing a strategic approach and creating specialized national and international GUCH centers is discussed [18].Currently, the clinical principles, methods and programs of rehabilitation of patients with congenital heart disease are well known, their effectiveness is proven and beyond doubt. The main problem of improving the quality and availability of rehabilitation care for this contingent of patients remains an organizational problem. To solve this problem, a necessary condition is government support, namely, setting priorities and tasks in the direction of improving rehabilitation care for the country's population, optimizing the legislative framework, and fulfilling these tasks [12].It is important to note that the majority of parents we surveyed consider compliance with the cardiologist’s recommendations and regular monitoring by medical specialists to be the most necessary conditions for the rehabilitation of a child with congenital heart disease (65.6% and 57.1%, respectively).Based on the analysis of parents' responses, the main types of violations of medical specialists' recommendations after a patient's discharge from a cardiac surgery hospital, their causes, possible consequences were determined, and ways to prevent and eliminate these violations were proposed [15].In our country, there is an uneven geographical distribution and an insufficient number of cardiac surgery clinics that perform the full range of operations on patients with congenital heart disease. Therefore, on a nationwide scale, the key point in improving medical care for children with congenital heart disease at the second stage of rehabilitation should be the creation of a network of specialized rehabilitation centers in accordance with the geography of the location of cardiac surgery clinics that provide high-tech medical care to such patients in the neonatal and early age in a volume of over 500 cases per year [12].The main violation of medical recommendations received by families of patients with congenital heart disease upon discharge from the cardiac surgery hospital was failure to comply with the schedule of visits to the pediatric cardiologist. Parents noted the following reasons for violating the schedule of visits to the cardiologist: - good health of the child; - territorial remoteness of the family's place of residence from the institution where the pediatric cardiologist works, and financial difficulties and a difficult journey associated with travel and accommodation; - distrust of parents in the qualifications of medical specialists at their place of residence; - uncertainty in the need for a consultation; - lack of clear information from parents on how to arrange an appointment and arrival for a consultation; - illness of the child (respiratory diseases); - lack of technical facilities, equipment of diagnostic equipment at the healthcare facility at the place of residence; - family problems: business trips of the spouse, transport breakdowns, vacations, the need to finish the school year, birth of children, etc.; - the only pediatric cardiologist in the area is on vacation or is absent due to illness. - a combination of the above reasons [15].We consider the main goal of creating the school to be providing families of patients with congenital heart disease with medical, social and psychological adaptation to life in society. There is no doubt that the school is in demand among parents of children with congenital heart disease. A child's path in a cardiac surgery hospital is very intense, and it is sometimes difficult for parents to figure it out on their own. Introductory instructions are necessary to introduce parents to the school, present the goals, tasks, functions of the CHD to parents, outline the prospects for interaction between parents and the CHD, as well as sign up for lectures and seminars, and to see a psychologist. In the future, we plan to post information about the CHD school in children's clinics in the city, maternity hospitals, a specialized maternity hospital for women with CHD, and children's clinical hospitals.Limited public awareness of the treatment of congenital heart disease leads to delays in the start of treatment, which affects the outcome of treatment and the quality of life of patients in the future [10].The components of the rehabilitation environment of a cardiac surgery hospital and a rehabilitation center for children with congenital heart disease include a spatial environment with the necessary material and technical support, a professional environment of qualified specialists, rehabilitation programs and technologies, and an automated information environment. The automated information environment includes the creation, storage, recording, reproduction, processing, reception, and transmission of information data in a medical institution using computer technologies: automated medical records, scientific databases, specialized programs for non-clinical units of a medical institution, and other work programs [15].The structural model of a rehabilitation center for children with congenital heart defects should reflect the structure of a cardiac surgery hospital, which will optimize routes and distribute patient flows. Providing rehabilitation care to children with congenital heart defects at a high level is impossible without modern, highly specific technical equipment of the center. The development of medical rehabilitation allows for the creation of a full cycle of effective medical care for children: early diagnosis - timely treatment - medical rehabilitation [11].Long hospitalization after surgery for congenital heart disease leads to the inappropriate use of surgical beds and additional financial costs that are not compensated by the surgical quota, reducing the availability of cardiac surgical care for other patients whose hospitalization is postponed due to the lack of free specialized beds. Follow-up treatment at the place of residence is often associated with organizational difficulties and the lack of sufficient experience of doctors in managing such patients [14].At present, there is no longer any doubt that, ultimately, the success of the treatment of children with congenital heart disease and their subsequent adaptation to life in society depends not only on a successful operation, and does not end with discharge from the cardiac surgery hospital. Of great importance here is informational support for the family on the problems of congenital heart disease at all stages of the child's treatment and observation [10].It is advisable to use the definition of functional classes of the cardiovascular system as an additional criterion for the integrated assessment of patients' health in the late period after surgical correction of congenital heart defects in the process of dispensary observation and individual rehabilitation. We believe that further study and development of modern models for objective assessment of the functional state of the cardiovascular system in children and adolescents with chronic cardiac pathology is promising [18].Indications and timing of medical rehabilitation of children after surgical treatment of congenital heart disease are determined by a cardiologist. At the same time, it is important to remember that from the moment of discharge from the cardiac surgery hospital after surgical treatment of congenital heart disease, responsibility for compliance with recommendations for rehabilitation of the patient in an outpatient setting mainly falls on his family [15].The work on treating a given patient is not limited to the fact of hospitalization. It is necessary to realize that our patients need qualified medical care after discharge from the hospital, at the stage of outpatient care, in the territories. Here, unfortunately, we experience a major shortage of qualified personnel and proper awareness of patients and their family members on the tactics of their further management [10].However, before the child enters school, it is advisable to conduct a test with a dosed physical load to determine the optimal regimen of physical education, especially in cases where attendance at sports sections or professional sports is assumed. It is important to explain to parents the objective condition of the child, since in some cases there are psychological and social problems in families, such as overprotection, limitation of normal physical activity, unjustified refusals to attend preschool institutions and the persistence of disability. Such patients, who after successful operations have good rehabilitation potential in the future, risk not receiving qualified rehabilitation care at their place of residence, which requires separate organizational measures when planning the 3rd stage of rehabilitation for them, including the possibility of feedback and continuous information support for their families [14].The results clearly show that children and families living with CHD face numerous challenges both in and outside of school. The concerns and recommendations raised by participants suggest that while many children and families found school to be a positive and enriching environment, others experienced ethical lapses and a lack of caring support, communication and knowledgeable school staff. When considering the results, it is evident that the present study has many implications for practice and policy development within the school system. The experiences of families living with CHD are unique and different from those living with other childhood illnesses as CHD is an unpredictable illness that forces families to live with constant uncertainty. Since parents will be justifiably hypervigilant and children with CHD have unique needs, schools must be prepared to provide support and meet these varied and changing needs. It is therefore imperative that schools are trained in CHD. Moreover, if school staff consider what we call the “Five Cs” of best practice (communication, confidentiality, coordination, competence, and compassion), the school experience and quality of life for children and families can be optimized [9].In some cases (impossibility of full correction of the defect, presence of a mechanical prosthesis, residual pulmonary hypertension, etc.) patients will have certain limitations; continuation of rehabilitation in this case is aimed at maximum improvement of the cardiovascular system function, psychological and social (including preparation for future work) adaptation. Thus, implementation of rehabilitation programs has both great humanistic and socio-economic significance for the state [14].In accordance with the types of rehabilitation care for children after surgical treatment of congenital heart disease, information from the database is grouped into sections on medical, psychological, educational, and social (socioeconomic) rehabilitation [15].Achieving high treatment results requires friendly cooperation between the patient and the medical staff. The staff must be in constant interaction with the patient. The main areas of work of the medical staff with the patient are as follows: patient education; ensuring patient safety and compliance with his constitutional rights; systematic analysis of the patient's opinion on the results of medical care.Patient safety is ensured by strict adherence to the technology of medical care. A significant role in creating safety guarantees is played by the patient's (or his parents') awareness of the nature of the proposed treatment and intervention. Registration of the patient's written consent for manipulations and operations, registration of stage and preoperative epicrises, which are agreed upon with the head of the clinical department, allow to exclude cases of insufficiently justified use of risky diagnostic manipulations and thus increase the safety of patients.Systematic analysis of patients’ opinions on the achieved treatment results and the general level of the clinic is a mandatory section of the administration’s work in the quality management system of the treatment and diagnostic process [10].Educators and school psychologists should also be encouraged to discuss how the needs of students with chronic health problems can be met. Professional development opportunities may need to be provided to educate psychologists, teachers, administrators, and support staff about the needs of children with chronic conditions such as CHD. Furthermore, by meeting with families living with chronic conditions and their health care providers, school nurses, and/or school counselors, educators and psychologists will learn about their needs and be better prepared to optimize their teaching and school experiences [9].It is important to emphasize that the effectiveness of rehabilitation care for children with congenital heart disease will increase when combining medical, social, psychological, psychotherapeutic, pedagogical, and professional measures into a single system, as well as with an individual approach to each child and his or her family. Perhaps, the primary task of medical rehabilitation is to motivate the family of each child with congenital heart disease to be on the same team with medical specialists. Teaching each family the rules of the team, especially outside the clinic, is the main task of medical specialists in the interests of the child with congenital heart disease. The team's efforts should also be aimed at transferring all the knowledge and skills obtained in the process of rehabilitation measures from the family to the child with congenital heart disease, in accordance with his or her ability to perceive this information at different stages of life. By the time a teenager with congenital heart disease is transferred to the healthcare system for the adult population, he or she should be maximally prepared to independently resolve possible problems arising in connection with the disease, clearly understand the need for further observation by a cardiologist and a healthy lifestyle, taking medications prescribed by a doctor, know all the necessary contact information for medical institutions and the sequence of actions in emergency situations. Preparing children and adolescents who have undergone surgical treatment for congenital heart disease to independently resolve these problems and improve their quality of life is the most important task of institutions providing rehabilitation care to this complex group of patients [11].In light of the changing attitude of higher authorities and increasing control over the quality of medical care provided, the openness of the clinic, the transparency of the system as a whole, and the availability of medical care are factors that equally protect us, as professionals, from possible risks, and us, as patients, minimizing the likelihood of medical errors at all stages of treatment.These and many other factors prompted us to think about creating a certain project, an information resource - a school for parents of children with congenital heart defects, including the development and implementation of training programs for relatives of patients with congenital heart defects, as well as providing them with psychological and legal assistance. Currently, on the issues of the cardiovascular system, a number of healthcare institutions have schools for patients with various diseases and risk factors, for example, "School of Prevention of Arterial Hypertension and Cardiovascular Diseases", "School for a Patient with Hypertension", "School for a Patient of the Cardiology Clinic of the St. Petersburg State Medical Academy named after I.I. Mechnikov. But these schools do not cover the range of issues that are of great interest to families of patients with congenital heart defects [10].For the purpose of improvement specialized medical care for children with diseases and congenital circulatory system defects a number of activities need to be carried out [2], (Table 2).Table 2. Key activities needed to improve specialized medical care for children with congenital circulatory system defects and diseases
 |
| |
|
Firstly, further development of pediatric cardiology is necessary services and training of specialists. With reliable influence of the quality of work specialized pediatric cardiology services to reduce mortality from cardiovascular pathology in childhood there is a real need at this age increasing the efficiency of such a service.Secondly, planning pregnancy. The main preventive measure an event aimed at preventing the development of heart disease in child, is planning pregnancy. Unfortunately, at present time this issue is in the masses population is understood extremely narrowly (more often in total within the framework of prevention unwanted pregnancy). At the local doctors and all workers in general Healthcare bears a heavy burden responsibility for conducting explanatory work with women of fertile age and provision information on the possible influence of factors external environment, hereditary factors, as well as diseases that women have risk of developing cardiovascular disease systems in a child and about measures prevention. Thirdly, prenatal diagnostics. Currently, diagnostics of anomalies of the heart can be performed both in the prenatal period and immediately after birth. What As for the issue of prenatal diagnostics, the basis for early detection of any congenital vice lies well organized screening of pregnant women. But qualified Fetal echocardiography (FE) can only be performed by specialists with sufficient experience in this area and, accordingly, owning methodology. Therefore, such specialists need to be train and concentrate in centers - inter-district, city, republican.Fourth, postnatal diagnosis. There is another area of influence - postnatal diagnostics, from timeliness on which in some cases the fate depends children born with critical congenital heart defects (hypoplasia left heart, critical stenosis aorta, aortic atresia, coarctation, atresia or pulmonary artery stenosis). The main thing is necessary timely diagnosis, correct transportation to the pediatric cardiac surgery department of the RKD and emergency surgery surgical correction of congenital heart disease.Implementation of modern surgical technologies. The prognosis for children with congenital heart disease is determined timely provision of surgical assistance using all existing, including high-tech ones, methods of treatment. It is also necessary to introduce them more widely into practice interventional interventions and minimally invasive surgery techniques VPS. Delay in this matter will require over time, increasingly serious financial, labor and professional costs.Mastering modern information technologies. The most important condition for increasing efficiency of the medical institution is the presence of accurate and versatile information on patient populations (registry patients), dispensary and preventive events, medical and diagnostic processes, as well as other aspects management. To achieve this, traditional methods of collection and processing information is impossible. The solution to this tasks can be accomplished only by creating automated medical information systems (AMIS), the basis of which should be become an electronic medical record.Carrying out the specified organizational activities will allow improve not only the quality of services medical care for children with cardiovascular diseases, including those with CHD, but also to reduce infant mortality from congenital malformations [2].A unified register of information on patients with congenital heart disease based on a rehabilitation center is necessary, first of all, for drawing up rehabilitation programs for patients with congenital heart disease, as well as for assessing the effectiveness of these programs. On the other hand, maintaining a unified register will allow creating statistical reports on treated, rehabilitated patients at the country level, as well as providing informational supplements to scientific research [15].The currently generally accepted methods of dispensary observation and rehabilitation of patients after surgical correction of congenital heart disease can be significantly improved and individualized, provided that an approach or system is created that generalizes all the characteristics of the operated heart, recreating its objective and complete morphofunctional portrait. The doctor must be able to qualitatively and consistently analyze not individual clinical and instrumental symptoms, but the entire set of specific changes caused by the anatomy and pathophysiology of a specific congenital heart disease, the nature and extent of cardiac surgical correction. It is extremely important to take into account the presence of residual or postoperative changes, complications, the state of the contractile myocardium, the cardiac conduction system, the level of markers of asymptomatic heart failure, destruction of cardiomyocytes, etc. The issues of implementing an effective practical program of dispensary observation and rehabilitation for children with congenital heart disease are relevant and require a solution [18].
3. Conclusions and Future Direction
Optimization of medical care for children after surgical treatment of congenital heart defects is a multifaceted process that includes not only surgical intervention, but also ensuring high-quality postoperative rehabilitation, effective coordination of the work of medical specialists and organization of accessible care for all categories of patients. It is important to consider that the success of treatment depends on a comprehensive approach, starting with early diagnosis and ending with long-term rehabilitation.While significant progress has been made in the surgical correction of congenital heart defects (CHDs), ensuring optimal long-term outcomes for affected children remains a challenge. Future directions in improving follow-up care for children after surgical correction should focus on several key areas:1. Development of Standardized Follow-up Protocols: There is a need for universally accepted guidelines that outline the frequency and types of follow-up assessments required for children post-surgery. These protocols should consider the type of CHD, the surgical procedure performed, and the individual needs of the patient.2. Multidisciplinary Care Teams: Establishing comprehensive, multidisciplinary teams involving pediatric cardiologists, surgeons, rehabilitation specialists, and mental health professionals is essential for providing holistic care. Regular collaboration among specialists will ensure that all aspects of the child's health—physical, emotional, and developmental—are addressed during follow-up.3. Long-Term Monitoring and Telemedicine: Implementing long-term monitoring systems using wearable technology or remote patient monitoring tools could help track the health of children after surgery. Telemedicine could play an essential role in providing accessible care to children who live far from specialized centers, improving follow-up adherence and outcomes.4. Psychosocial and Developmental Support: It is important to assess not only the physical health of children post-surgery but also their psychological and cognitive development. Future research should explore effective interventions to support children with CHDs, especially those who may face developmental delays or social integration challenges due to their condition.5. Patient and Family Education: Educating families about the importance of follow-up care, recognizing warning signs of complications, and understanding the long-term health implications of CHD is crucial. Educational programs should be tailored to each family's needs and should include accessible resources for managing the child's care at home.6. Personalized Medicine and Genomic Research: Advances in genomics and personalized medicine could offer more insights into the underlying causes of CHDs, as well as potential long-term effects of different surgical interventions. A better understanding of genetic predispositions and individual responses to treatments can guide more personalized follow-up care strategies.7. Improved Data Collection and Research: To optimize follow-up strategies, more data is needed on the long-term outcomes of children with CHDs after surgery. Large-scale, multicenter studies and registries can help identify patterns and trends that can be used to refine treatment protocols and improve outcomes for future generations.
References
| [1] | Dai, Wang-Sheng et al. “Postoperative health-related quality of life in children with congenital heart disease: a short-term follow-up study.” Journal of cardiothoracic surgery vol. 18.1 17. 11 Jan. 2023, doi:10.1186/s13019-023-02110-x. |
| [2] | Murzabaeva S.Sh., Karamova I.M., Yakovleva L.V., Malievsky V.A., Plechev V.V., Lukmanova T.V., and Nagaev I.A. "Current tasks of organizing specialized care for children with cardiovascular diseases" Medical Bulletin of Bashkortostan, vol. 2, no. 1, 2007, pp. 7-9. |
| [3] | Hasan, Babar S et al. “Recommendations for developing effective and safe pediatric and congenital heart disease services in low-income and middle-income countries: a public health framework.” BMJ global health vol. 8.5 (2023): e012049. doi:10.1136/bmjgh-2023-012049. |
| [4] | Tchervenkov, Christo I et al. “The improvement of care for pediatric and congenital cardiac disease across the World: a challenge for the World Society for Pediatric and Congenital Heart Surgery.” Cardiology in the young vol. 18 Suppl 2 (2008): 63-9. doi:10.1017/S1047951108002801. |
| [5] | Khomyakova O. I. , Silverstova L. A .. "Rehabilitation and dispensary care of sick children with transposition of the great vessels in the postoperative period in the regional children 's cardiorheumatology center of Tula" Symbol of Science, no. 7, 2017, pp. 90-94. |
| [6] | Carmona, Fabio et al. “Collaborative Quality Improvement in the Congenital Heart Defects: Development of the ASSIST Consortium and a Preliminary Surgical Outcomes Report.” Brazilian journal of cardiovascular surgery vol. 32.4 (2017): 260-269. doi:10.21470/1678-9741-2016-0074. |
| [7] | Clinical guidelines for the care of children with congenital heart defects. Ed. by L.A. Bokeria. Moscow: A.N. Bakulev National Center for Cardiovascular Surgery; 2014. |
| [8] | Bokeria L.A., Cardiology and cardiac surgery - innovative development. MATERIALS OF THE PRESIDIUM OF THE RAMS, 2012. |
| [9] | https://files.eric.ed.gov/fulltext/EJ 842008.pdf |
| [10] | Krupyanko Sofia Mikhailovna INNOVATIVE TECHNOLOGIES AS A FACTOR IMPROVING THE QUALITY OF TREATMENT FOR CHILDREN WITH CONGENITAL HEART DEFECTS, 2010, Abstract of a dissertation for the degree of Doctor of Medical Sciences, Moscow". |
| [11] | Bokeria L.A., Milievskaya E.B., Krupyanko S.M., Manerova O.A. Integral components of the optimal model for organizing rehabilitation care for patients after surgical treatment of congenital heart defects Federal State Budgetary Scientific Institution Scientific Center of Cardiovascular Surgery named after A.N. Bakulev, Moscow 11/25/2014. |
| [12] | Milievskaya E.B. "Prospects for the application of public-private partnership mechanisms to improve rehabilitation care for patients with congenital heart defects" Healthcare Manager, no. 1, 2015, pp. 28-34. |
| [13] | Khairetdinova, T.B. A.R. Khabibullina REHABILITATION POTENTIAL OF CHILDREN WHO UNDERWENT RADICAL CORRECTION OF SEPTAL CONGENITAL HEART DEFECTS Medical Bulletin of Bashkortostan. Vol. 12, No. 6 (72), 2017. |
| [14] | Bokeria, L.A. Organizational planning of the third stage of rehabilitation of children with congenital heart defects of different age groups / L.A. Bokeria, E.B. Milievskaya, S.M. Krupyanko, M.N. Nevedrova // Healthcare Manager. - 2015. - No. 9. - P. 20-27. |
| [15] | Bokeria L.A., Milievskaya Elena Borisovna, Krupyanko S.M., Shaikhutdinov M.I., Luzhetsky A.S., and Smirnov I.S. "Information database as a stage of creating a single register of patients with congenital heart defects" Problems of standardization in health care, no. 5-6, 2014, pp. 8-16. |
| [16] | Bokeria L.A., Krupyanko S.M., Milievskaya E.B., and Manerova O.A. "On the issue of staffing standards for a rehabilitation center for children with congenital heart defects" Healthcare Manager, no. 5, 2015, pp. 31-38. |
| [17] | Gorelik N.V., Antonenko F.F., Miroshnichenko V.A., Perelypteyn N.N., Stolina M.L., and Pavlov A.V. "Remote results of surgical treatment of congenital heart defects in children in Primorsky Krai" Acta Biomedica Scientifica, no. 4, 2005, pp. 107-112. |
| [18] | GONCHAR M.A., IMPROVEMENT OF DISPENSARY OBSERVATION OF CHILDREN AFTER SURGICAL CORRECTION OF CONGENITAL HEART DEFECTS. SCIENTIFIC NEWS Series Medicine. Pharmacy. 2014. No. 18 (189). |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML