-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1273-1277
doi:10.5923/j.ajmms.20251504.89
Received: Apr. 6, 2025; Accepted: Apr. 25, 2025; Published: Apr. 29, 2025

Tactics of Reconstructive and Plastic Surgical Operations in Diabetic Foot Syndrome
Matmuratov Kuvondik Jumaniyazovich , Sattarov Inayat Saparbaevich , Atajоnov Tulkinbek Shavkatovich , Safarov Farkhod Abdukhalilovich, Norzhigitov Sarvar Abdukayumovich
Tashkent Medical Academy, Uzbekistan
Copyright © 2025 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Inadequate surgical intervention technique selection in the construction of an appropriate foot is linked to high rates of reoperations and the prevalence of postoperative sequelae. The selection of the surgical technique based on the affected area is crucial for the formation of a weight-bearing foot. It is also important to maintain the integrity of the nutrient artery in a particular area of the foot, which is vital for feeding the foot's tissues. An adequate assessment of the peripheral arterial bed is crucial in this case. The aim of this research focused to enhance the outcomes of treating wound defects in diabetic foot syndrome by employing a distinct method to foot surgery.
Keywords: Diabetes mellitus, Neurotrophic ulcers, Reconstructive plastic surgery
Cite this paper: Matmuratov Kuvondik Jumaniyazovich , Sattarov Inayat Saparbaevich , Atajоnov Tulkinbek Shavkatovich , Safarov Farkhod Abdukhalilovich, Norzhigitov Sarvar Abdukayumovich , Tactics of Reconstructive and Plastic Surgical Operations in Diabetic Foot Syndrome, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1273-1277. doi: 10.5923/j.ajmms.20251504.89.
1. Introduction
- Diabetes mellitus (DM) is one of the main health problems of the 21st century. The number of patients with diabetes has been steadily increasing over the past three decades, and this growth is likely to continue over the next few decades: from about 463 million patients aged 18 to 99 in 2019 to about 700 million people in the same age group in 2045 worldwide [2,11].Modern aspects of the development of blighty health care include a number of measures aimed at improving the treatment outcomes of patients with DM and DFS, who need constant monitoring due to the introduction of modern principles of intensive care, surgical tactics and improvement of reconstructive operations [1,6].One of the most severe disabling complications of diabetes mellitus is DFS, which manifests itself in the development of widespread purulent-necrotic processes in the lower extremities, which are observed in 35-60% of patients with DM [3,8].Timely and adequate surgical treatment of patients with purulent-necrotic complications of DFS largely determines the course and outcome of the disease. Improvement of the results of surgical treatment of purulent-necrotic diseases of the feet in diabetes mellitus is currently associated with the maximum possible preservation of the опорной function of the affected limb. The most difficult patients are those with the neuroischemic form of DFS, whose condition is aggravated by both ischemia of the foot and progressive infection against the background of various concomitant diseases associated with deep neuropathy [5,11].When a purulent-necrotic process is present on the foot in the neuropathic form of DFS, the patient needs to undergo radical surgical treatment, if it is feasible, along with simultaneous closure (plastic surgery) of the surgical wound. This is crucial for patients who have lower extremity gangrene.Treatment for lower extremity gangrene in the context of diabetes that results in a demarcation line consists of sophisticated conservative therapy that includes necrectomy and phased procedures. Disarticulation of the finger is carried out with resection of the proximal portion of the corresponding metatarsal bone if the course of diabetic gangrene is quite favorable, which occurs after 7–10 days of conservative therapy and the emergence of a distinct line of demarcation.The literature data analysis revealed that there is still much work to be done in order to improve the tactical aspects of DBS surgical treatment. Regretfully, there are currently no studies that describe the methodology for preoperative planning and postoperative monitoring in patients with adverse prognostic variables and in this severe category of patients.Inadequate surgical intervention technique selection in the construction of an appropriate foot is linked to high rates of reoperations and the prevalence of postoperative sequelae. The selection of the surgical technique based on the affected area is crucial for the formation of a weight-bearing foot. It is also important to maintain the integrity of the nutrient artery in a particular area of the foot, which is vital for feeding the foot's tissues. An adequate assessment of the peripheral arterial bed is crucial in this case.The aim of this research focused to enhance the outcomes of treating wound defects in diabetic foot syndrome by employing a distinct method to foot surgery.
2. The Main Part
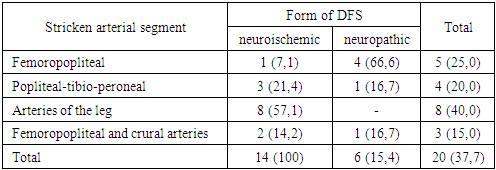
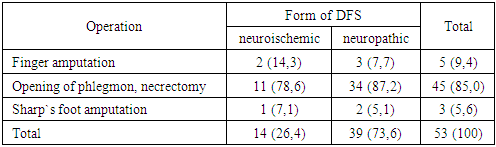
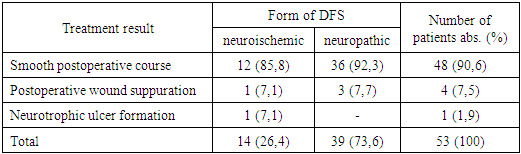
- In present-day surgery, the risk of developing postoperative complications in the early postoperative period persists despite the detailed development of methods for reconstructive plastic surgery of the foot against the backdrop of DFS. This forces us to search for new ways to perform this surgical intervention. This situation prompted a unique scientific investigation to develop a reliable technique for performing it and preventing an adverse course of the postoperative period in patients who have undergone reconstructive plastic surgery and have purulent-necrotic lesions of the foot.Following reconstructive plastic surgery, patients must go through a rehabilitation period that corrects the function of metabolic disorders and is necessary for them to resume their social lives. Reconstructive plastic surgery techniques vary depending on the amount of healthy tissue present. The goal is to maintain the foot's function as much as possible, optimize the biomechanics of the foot to stabilize it, make it suitable for orthopaedic prosthetics, and avoid complications like postoperative trophic ulcers. Reconstructive plastic surgery kinds and techniques vary in surgical practice depending on how and when each of the above stages will be executed.Indications for reconstructive plastic surgery and aspects of wound care following surgery, contingent on the foot's placement, are critical problems for the operating surgeon to solve in complex clinical scenarios. Patients in this category may see an increase in quality of life if their problems are promptly resolved and a new, distinct surgical intervention technique is developed, contingent upon the location of the foot wound defect [4,9].This study analyzed the results of surgical treatment of 53 patients who received inpatient treatment in the department of purulent surgery of the multidisciplinary clinic of the Tashkent Medical Academy in 2021-2022, for whom reconstructive plastic surgery on the foot was performed using improved technology (depending on the location of the wound defect and the affected part feet).
|
|
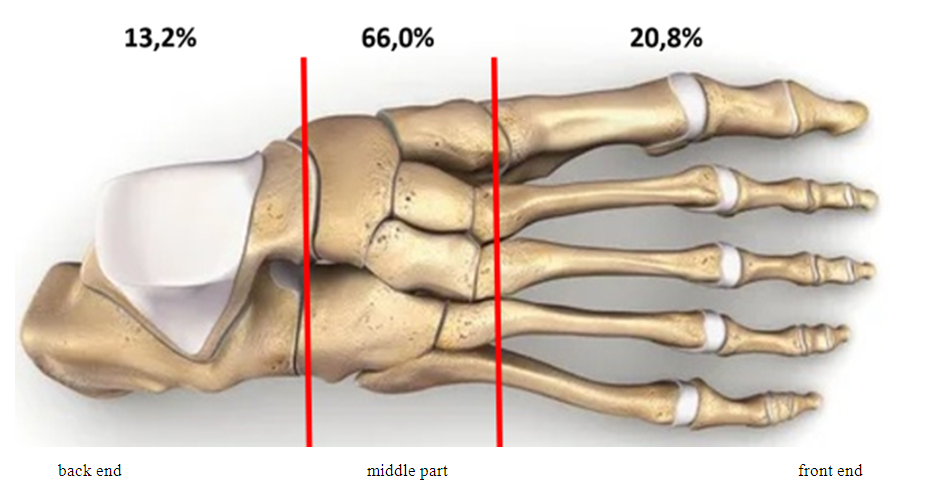 | Figure 1. Number of operations performed on parts of the foot |
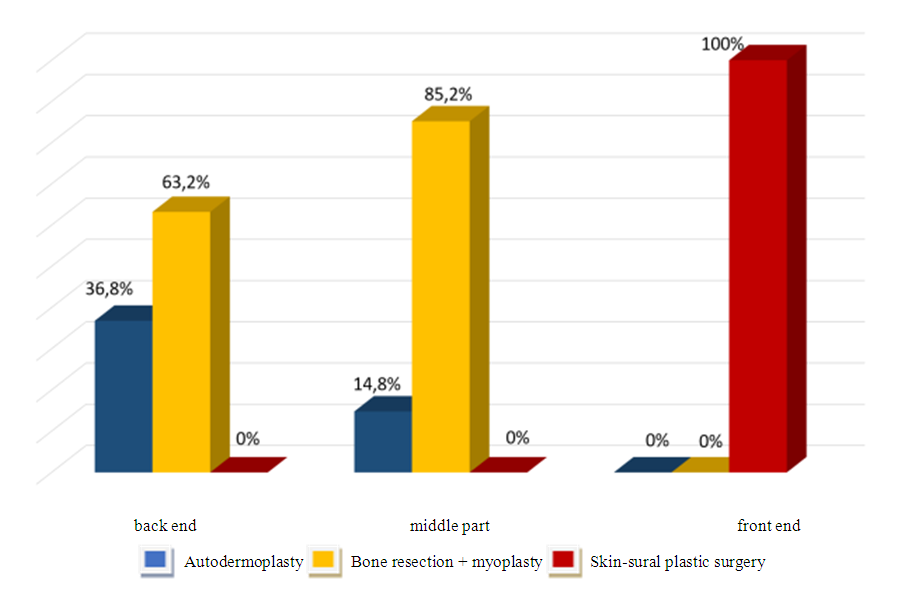 | Figure 2. Surgical interventions performed on parts of the foot |
|
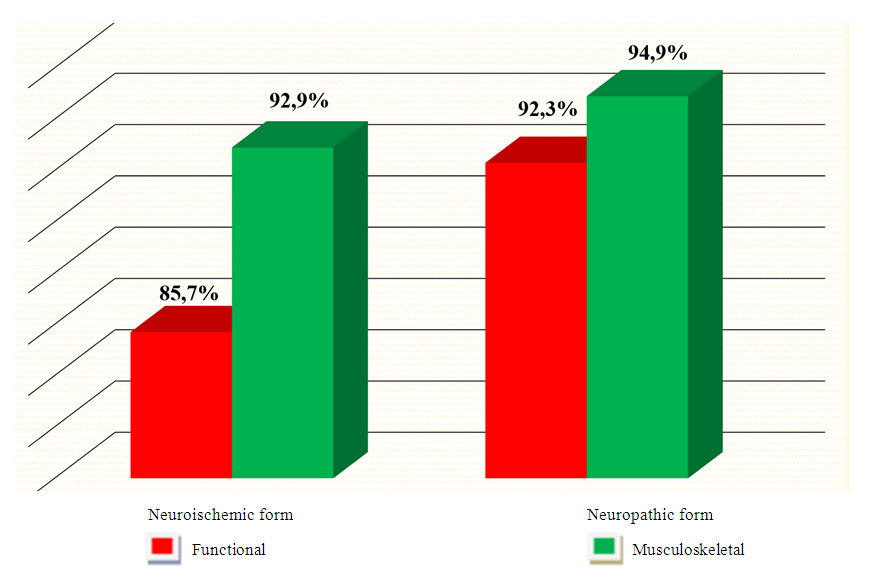 | Figure 3. Preservation of the foot in patients depending on the form of DFS |
3. Conclusions
- 1. The initial results (up to 3 months) in the comparison group (n=62) demonstrated that primary healing of the postoperative wounds occurs in 70.9% of cases (p>0.05) when patients with DBS undergo reconstructive plastic surgery using the standard method. 8.1% (p>0.05) of patients experienced purulent problems throughout the postoperative period. In 21.0% of patients (p>0.05), neurotrophic ulcers were seen to develop on the surgical foot soon after. Neurotrophic alterations were seen in 84.6 and 15.4% of cases with DFS in the neuropathic form, respectively, which is more common than the neuroischemic type.2. Modifications to the foot's biomechanics and supporting point brought on by bone loss are the primary factor in the etiopathogenesis of neurotrophic ulcers against the background of DFS. Patients with purulent-necrotic foot lesions resulting from DFS should avoid potential complications after surgery by utilizing the best reconstructive surgical techniques in a timely manner.3. Patients in the main group (n=53) who underwent differentiated reconstructive plastic surgery based on the location of their foot deformity experienced primary healing in 90.6% of instances (p>0.05), a considerably higher percentage than patients in the group comparison (70.9%). Neurotrophic ulcers were rare in this patient group throughout the postoperative phase, occurring in 1.9% of cases compared to 21.0 % in the comparator group (p>0.05).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML