-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 1267-1269
doi:10.5923/j.ajmms.20251504.87
Received: Mar. 17, 2025; Accepted: Apr. 15, 2025; Published: Apr. 29, 2025

Indicators of Antiphospholipid Syndrome and Its Influence on IVF Results
Usmanova Khilolakhon Anvarovna 1, Maksudova Mukhayyo Mansurovna 1, Kayumov Abdurakhman Abdumavlyanovich 2, Ozoda Umarkulovna Achilova 3
1“Siz Ona Bo’lasiz Eku Markazi”, Tashkent, Uzbekistan
2Administration, Republican Specialized Scientific-Practical Medical Center of Hematology MoH RUz, Tashkent, Uzbekistan
3Department of Hematology (Clinic), Republican Specialized Scientific-Practical Medical Center of Hematology (RSSPMCH) MoH RUz, Tashkent, Uzbekistan
Correspondence to: Kayumov Abdurakhman Abdumavlyanovich , Administration, Republican Specialized Scientific-Practical Medical Center of Hematology MoH RUz, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

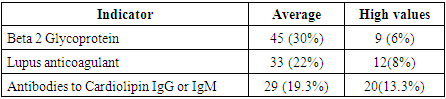
Antiphospholipid syndrome (APS) is an autoimmune disease with characteristic clinical manifestations, the main one being: the formation of blood clots in the vessels. One of the complications of this syndrome is miscarriage. In the structure of fetal losses, APS syndrome accounts for 22-27%, which is the main reason for studying its manifestation in habitual miscarriage. The aim of the study. To determine the indicators of APS syndrome and its impact on the results of “in vitro fertilization” (IVF). Materials and methods. The study included 150 women examined for habitual non-pregnancy at “Siz Ona Bo’lasiz Eku Markazi” Clinic. Of them, 100 with pregnancy termination more than 3 times at 4 to 39 weeks, and 50 patients with IVF failures more than 3 times. Results. A direct correlation between pregnancy loss and the level of antiphospholipid antibodies (APA) was revealed. Thus, in patients in the group with high antibody level there were more frequent fetal losses at early term up to 10 weeks in 30 (20%) patients (r=0.8), IVF failures in 28 (18.6%) patients (r=0.7), biochemical pregnancy after IVF without further pregnancy development in 9 (6%) (r=1.0). Meanwhile, the mean Betta2glycoprotein level in this group was 45±3.4U/ml, VA level was 1.7±0.4, cardiolipin IgG and/or IgM level was 27±4U/ml.
Keywords: Antiphospholipid syndrome (APS), “In vitro fertilization” (IVF), Pregnancy, Antiphospholipid antibodies (APA), IVF failures
Cite this paper: Usmanova Khilolakhon Anvarovna , Maksudova Mukhayyo Mansurovna , Kayumov Abdurakhman Abdumavlyanovich , Ozoda Umarkulovna Achilova , Indicators of Antiphospholipid Syndrome and Its Influence on IVF Results, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 1267-1269. doi: 10.5923/j.ajmms.20251504.87.
Article Outline
1. Introduction
- At the very beginning of the study of APS-syndrome was an autoimmune disease with characteristic clinical manifestations, the main of which was the formation of various blood clots in blood vessels. Today, APS syndrome is an interdisciplinary problem in medicine, which is addressed by rheumatologists, obstetrician-gynecologists and vascular surgeons [1,2]. At the dawn of the 20th century, autoimmune processes as the etiology of thrombosis were treated very skeptically. Basically in arterial thrombosis, atherosclerosis of vessels was sought, and venous thrombosis was characterized as mechanical insufficiency of vessel walls, changes in blood flow and blood rheology. Proof of the autoimmune nature of thrombosis in the 1980s was a real discovery, first of all for immunologists, and the same mechanism was demonstrated by nature in 2020 by the example of thrombosis in virus-associated COVID-19 pneumonias [3]. APS is usually divided into primary APS, manifested by repeated fetal loss, and secondary APS after systemic lupus erythematosus (SLE) and other autoimmune diseases - for example, 1/3 of patients with SLE have APS syndrome. This nature of thrombosis undoubtedly suggests an indication for anticoagulant therapy. However, the autoimmune nature of the lesion requires the combination of anticoagulant therapy with weak immunosuppressants. In EULAR (European Association of Rheumatologists) recommendations from 2023 [3], recommendations for the use of hydroxychloroquine sulfate for the treatment of APS syndrome are given and its safety in pregnant women is proved. According to literature data, among pregnant women with habitual fetal loss APS-syndrome is diagnosed in 27-42% of cases [6-8] and without immunosuppressant and anticoagulant therapy in 90-95% of women positive for antibodies to phospholipids pregnancy termination occurs. Thus, it became necessary to analyze the frequency of APS syndrome in women with habitual miscarriage [4-5].The aime To determine the severity of laboratory indicators of APS syndrome and its influence on the timing of pregnancy termination in patients with habitual miscarriage.
2. Main Body
2.1. Material and Methods of Study
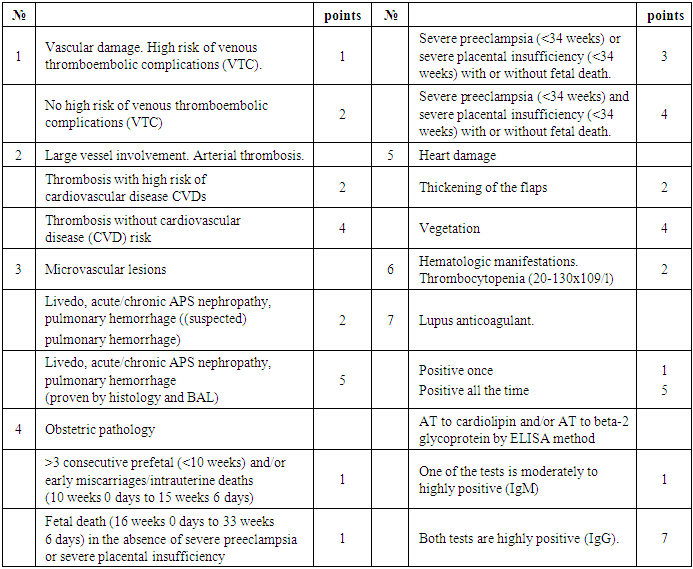
- The study included 150 women between 2023 and 2024 receiving therapy for habitual non-pregnancy at Siz She Bulasiz Clinic. Of them, 100 with pregnancy termination more than 3 times at 4 to 39 weeks, and 50 patients with IVF failures more than 3 times.The mean age of the women was 25.2 ± 4.2 years (29-45 years). Blood tests for cardiolipin IgG and IgM and to beta-2 glycoprotein were determined by enzyme-linked immunosorbent assay with reagents from “Orgentec Diagnostika GmbH” (Germany). Determination of “lupus anticoagulant” and screening tests of coagulogram (ACL, PTI (prothrombin index), fibrinogen, INR, thrombin time) was performed using coagulometer “ACL TOP-350” (Instrumental Laboratory, Spain). Data processing was performed using standard programs “Statistika”, EXCEL with identification of mean values. The diagnosis of APS syndrome was made according to the criteria of “EULAR 2023” [3], in the presence of a laboratory diagnosis of APS syndrome. [3], in the presence of laboratory criterion and clinical criterion according to the scores (Table 1).
|
2.2. Results of the Study
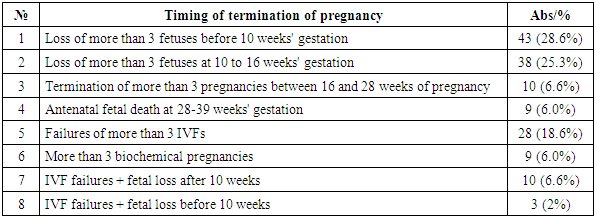
- Among the examined women there were women with loss of 3 pregnancies up to 10 weeks 43 (28.6%), with loss of 3 or more pregnancies from 10 to 16 weeks 38 (25.3%), fetal loss from 16 to 28 weeks 10 (6.6%) and 9 (6.0%), antenatal fetal death from 28 to 39 weeks, more than 3 unsuccessful results of IVF - 28 (18. 6%), more than 3x “biochemical” pregnancies 9 (6.0%), history of IVF failure and fetal loss after IVF up to 10 weeks 3 (2%), IVF failure and fetal loss above 10 weeks 10 (6.6%). The pattern of pregnancy loss is summarized in Table 2.
|
|
3. Conclusions
- According to various authors, antiphospholipid antibodies (APA) are found in 22–27% of patients with habitual miscarriage [5,6]. At the same time, all sources indicate a more significant effect of antibodies to beta2 glycoprotein on thrombogenesis and miscarriage. In our study, we fully confirmed these data, but it was also stated that with a high level of beta2 glycoprotein antibodies, there is a very high risk of miscarriage in the early stages, perhaps this is also associated with the tropism of these antibodies to embryonic cells. At a later stage, lupus anticoagulant and antibodies to cardiolipin played a major role in the genesis of fetal loss in our study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML